Search
- Page Path
- HOME > Search
- Correlations between regional characteristics of counties and the ratio of intracounty to extracounty sources of COVID-19 in Gangwon Province, Republic of Korea
- Seungmin Jeong, Chaeyun Lim, Sunhak Bae, Youngju Nam, Eunmi Kim, Myeonggi Kim, Saerom Kim, Yeojin Kim
- Osong Public Health Res Perspect. 2023;14(3):219-223. Published online June 8, 2023
- DOI: https://doi.org/10.24171/j.phrp.2023.0014
- 1,334 View
- 32 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 
- Objectives
This study aimed to examine the correlations between the regional characteristics of counties in Gangwon Province, Republic of Korea and the ratio of intracounty to extracounty sources of coronavirus disease 2019 (COVID-19) infection.
Methods
The region of the infectious contact was analysed for each COVID-19 case reported in Gangwon Province between February 22, 2020 and February 7, 2022. The population, population density, area, the proportion of urban residents, the proportion of older adults (>65 years), financial independence, and the number of adjacent counties were assessed for each of the 18 counties in Gangwon Province. Correlation coefficients between regional characteristics and the ratio of intracounty to extracounty infections were calculated.
Results
In total, 19,645 cases were included in this study. The population, population density, proportion of older adults, and proportion of urban residents were significantly correlated with the ratio of intracounty to extracounty infections. A stratified analysis with an age cut-point of 65 years showed that the proportion of older adults had a significant negative correlation with the ratio of intracounty to extracounty infections. In other words, the proportions of extracounty infections were higher in countries with higher proportions of older adults.
Conclusion
Regions with ageing populations should carefully observe trends in infectious disease outbreaks in other regions to prevent possible transmission.
- Effectiveness of the COVID-19 vaccine in the Honam region of the Republic of Korea
- In-Sook Shin, Yong-Pyo Lee, Seung-Hoon Lee, Jae-Young Lee, Jong-Ha Park, Yoon-Seok Chung
- Osong Public Health Res Perspect. 2023;14(3):197-206. Published online June 8, 2023
- DOI: https://doi.org/10.24171/j.phrp.2022.0308
- 1,829 View
- 63 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 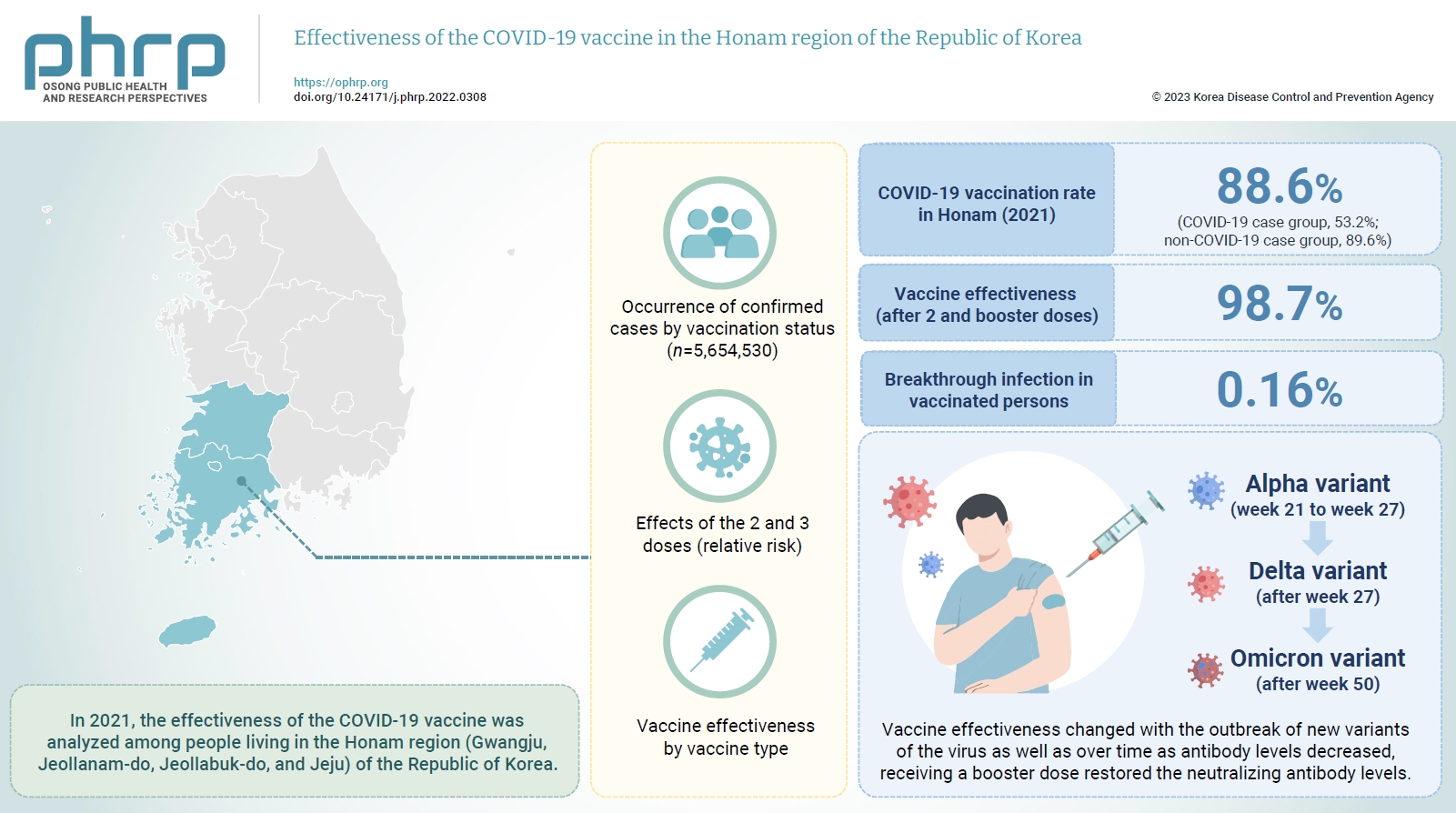
- Objectives
In 2021, the effectiveness of the COVID-19 vaccine was analyzed among people living in the Honam region (Gwangju, Jeollanam-do, Jeollabuk-do, and Jeju) of the Republic of Korea. And we investigated changes in the dominant virus strain.
Methods
This study used the data provided by the Korean Ministry of the Interior and Safety for individuals ≥12 years old in the Honam region, and the Integrated Disease and Health Management System of the Korea Centers for Disease Control and Prevention for COVID-19-vaccinated individuals as of December 31, 2021. Statistical analyzes were performed using IBM SPSS ver. 23.0. The occurrence of confirmed cases by vaccination status, the relative risk, and vaccine effectiveness by vaccine type were calculated.
Results
In 2021, the COVID-19 vaccination rate in Honam was 88.6%. The overall vaccine effectiveness (after 2 and 3 doses) was 98.7% (p<0.001). and the breakthrough infection rate was 0.16%. From week 21 to week 27 of 2021 (June 27 to July 3), the genome sequencing results were mostly alpha variants. The Delta variant emerged as the dominant variant after 27 weeks and the Omicron variant was found at 50 weeks (December 5–11).
Conclusion
Vaccine effectiveness changed with the outbreak of new variants of the virus as well as over time as antibody levels decreased. that the prevention effectiveness of vaccination in Honam was >98%, and the effect among persons who received 2 doses was >90% regardless of the vaccine type. Although vaccine effectiveness decreased because of reduced antibody levels over time (as observed in breakthrough infections), receiving a booster dose restored the neutralizing antibody levels.
- The first reported hepatitis E outbreak in a food manufacturing factory: Korea, 2022
- Hansol Yeom, Soonryu Seo, Youngsil Yoon, Jaeeun Lee, Myung-Guk Han, Deog-Yong Lee, Sun-Whan Park, Song A Park, Sook-Hyang Jeong, Jin Gwack
- Osong Public Health Res Perspect. 2023;14(1):15-22. Published online February 22, 2023
- DOI: https://doi.org/10.24171/j.phrp.2022.0305
- 1,621 View
- 135 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 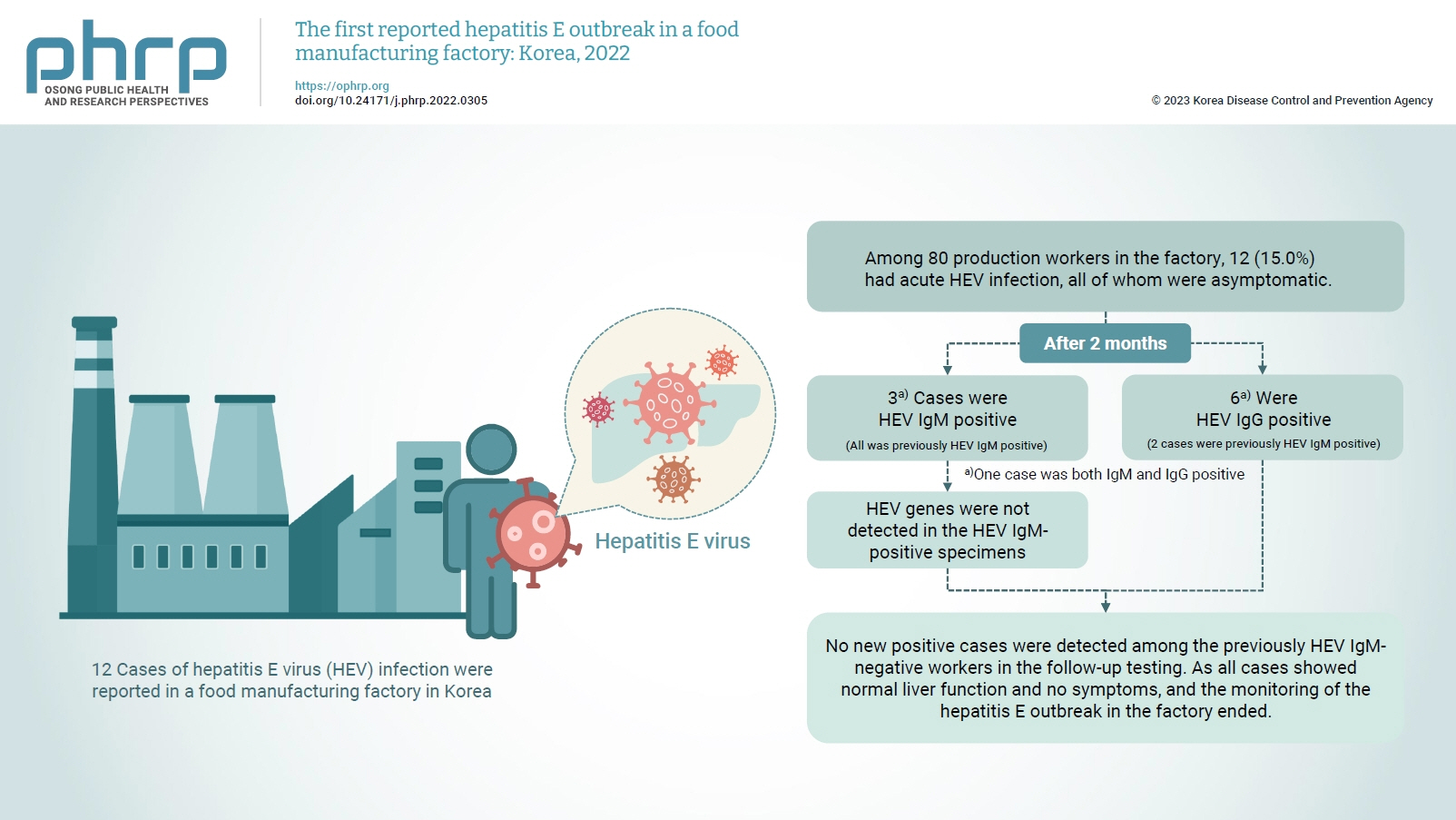
- Objectives
On February 16, 2022, 12 cases of hepatitis E virus (HEV) infection were reported in a food manufacturing factory in Korea. The aim of this study was to identify additional cases and to determine the source of this HEV outbreak. Methods: This study was an in-depth investigation of 12 HEV immunoglobulin M (IgM)-positive cases and their demographic, clinical, and epidemiological characteristics. On-site specimens were collected from the environment and from humans, and a follow-up investigation was conducted 2 to 3 months after the outbreak. Results: Among 80 production workers in the factory, 12 (15.0%) had acute HEV infection, all of whom were asymptomatic. The follow-up investigation showed that 3 cases were HEV IgMpositive, while 6 were HEV IgG-positive. HEV genes were not detected in the HEV IgM-positive specimens. HEV genes were not detected in the food products or environmental specimens collected on-site. HEV was presumed to be the causative pathogen. However, it could not be confirmed that the source of infection was common consumption inside the factory. Conclusion: This was the first domestic case of an HEV infection outbreak in a food manufacturing factory in Korea. Our results provide information for the future control of outbreaks and for the preparation of measures to prevent domestic outbreaks of HEV infection.
- A case-control study of acute hepatitis A in South Korea, 2019
- Jung Hee Hyun, Ju Young Yoon, Sang Hyuk Lee
- Osong Public Health Res Perspect. 2022;13(5):352-359. Published online October 12, 2022
- DOI: https://doi.org/10.24171/j.phrp.2022.0141
- 2,862 View
- 116 Download
- 1 Web of Science
- 4 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 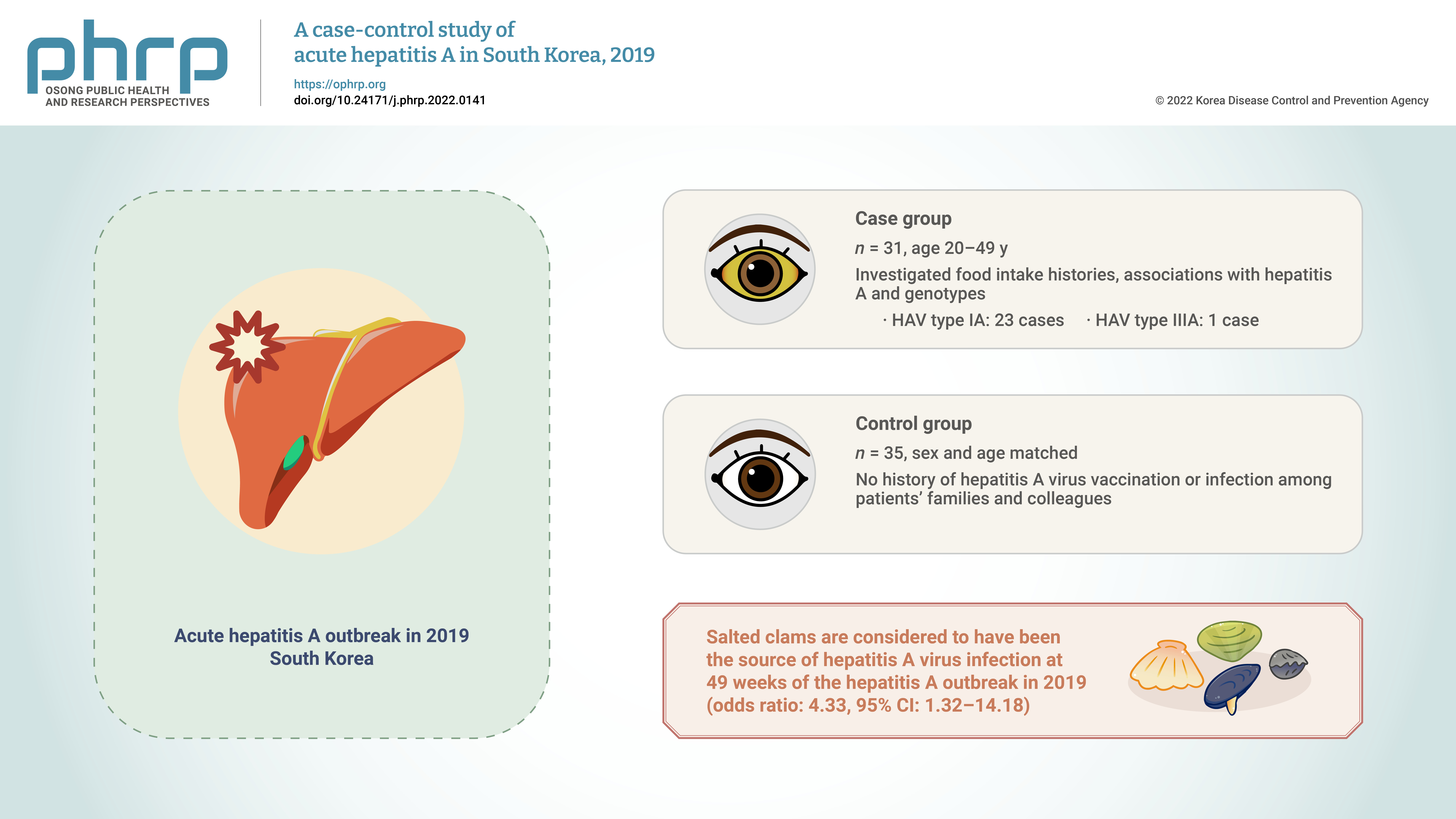
- Objectives
We aimed to reconfirm the source of hepatitis A virus (HAV) infection through epidemiological and genotype investigations of individual cases in a 2019 outbreak in South Korea. Methods: We investigated food intake histories, associations with hepatitis A, and genotypes of HAV in 31 patients with hepatitis aged 20 to 49 years registered in the integrated disease and health management system during December 1–7, 2019 (case group) and in 35 sex- and agematched people without a history of HAV vaccination or infection among patients’ families and colleagues (control group). Results: The consumption of salted clams was a significant factor (odds ratio, 4.33; 95% confidence interval, 1.32–14.18) in the risk factor analysis of food intake history. HAV genotypes were analyzed in 24 of 31 patients. Type IA and type IIIA were found in 23 and 1 cases, respectively. Conclusion: Salted clams are considered to have been the source of HAV infection at 49 weeks of the HAV outbreak in 2019; this result was consistent with that of a previous epidemiological investigation conducted by the Korea Disease Control and Prevention Agency in September 2019. Therefore, monitoring of the production and distribution of salted clams needs to be continued. -
Citations
Citations to this article as recorded by- Monitoring viruses and beta-lactam resistance genes through wastewater surveillance during a COVID-19 surge in Suwon, South Korea
Rajendra Singh, Jaewon Ryu, Sung Soo Park, Sungpyo Kim, Keugtae Kim
Science of The Total Environment.2024; 922: 171223. CrossRef - Prevalence of foodborne viruses and influenza A virus from poultry processing plants to retailed chickens
Daseul Yeo, Mengxiao Song, Md. Iqbal Hossain, Soontag Jung, Zhaoqi Wang, Dong Joo Seo, Min Suk Rhee, Changsun Choi
Frontiers in Sustainable Food Systems.2023;[Epub] CrossRef - A Study on the Detection Rate of Hepatitis A from Gastroenteritis Patients and the Genotype Analysis of Hepatitis A Virus in Busan
Sun Hee Park, Chanhee Kim, Summi Lee, Jihye Jeong, Junghye Choi, Seung Ju Lee
Journal of Bacteriology and Virology.2023; 53(2): 74. CrossRef - A Study on the Detection Rate of Hepatitis A from Gastroenteritis Patients and the Genotype Analysis of Hepatitis A Virus in Busan
Sun Hee Park, Chanhee Kim, Summi Lee, Jihye Jeong, Junghye Choi, Seung Ju Lee
Journal of Bacteriology and Virology.2023; 53(2): 74. CrossRef
- Monitoring viruses and beta-lactam resistance genes through wastewater surveillance during a COVID-19 surge in Suwon, South Korea
- Changes in the pattern and disease burden of acute respiratory viral infections before and during the COVID-19 pandemic
- Chungmin Park, Donghan Lee, Bryan Inho Kim, Sujin Park, Gyehee Lee, Sangwoo Tak
- Osong Public Health Res Perspect. 2022;13(3):203-211. Published online June 30, 2022
- DOI: https://doi.org/10.24171/j.phrp.2022.0144
- 4,361 View
- 168 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
We conducted a comparative analysis of the differences in the incidence of 8 acute respiratory viruses and the changes in their patterns before and during the coronavirus disease 2019 (COVID-19) pandemic. Methods: Three sentinel surveillance systems of the Korea Disease Control and Prevention Agency and data from the Health Insurance Review and Assessment Service were analyzed. The average numbers of reported cases and the related hospital admissions and outpatient data were compared between April 2018–2019 and 2020–2021. Changes in the disease burden and medical expenditures between these 2 time periods were evaluated. Results: During the COVID-19 pandemic, the number of reported cases of all acute respiratory viral infections, except for human bocavirus, decreased significantly. Data from the Health Insurance Review and Assessment Service also showed decreases in the actual amount of medical service usage and a marked reduction in medical expenditures. Conclusion: Non-pharmacological interventions in response to COVID-19 showed preventive effects on the transmission of other respiratory viruses, as well as COVID-19. Although COVID-19 had a tremendous impact on society as a whole, with high social costs, there were also positive effects, such as a reduction in the incidence of acute respiratory viral infections. -
Citations
Citations to this article as recorded by- Machine learning forecasts for seasonal epidemic peaks: Lessons learnt from an atypical respiratory syncytial virus season
Roger A. Morbey, Daniel Todkill, Conall Watson, Alex J. Elliot, André Ricardo Ribas Freitas
PLOS ONE.2023; 18(9): e0291932. CrossRef
- Machine learning forecasts for seasonal epidemic peaks: Lessons learnt from an atypical respiratory syncytial virus season
- Seroprevalence of immunoglobulin G antibodies against SARS-CoV-2 in children and adolescents in Delhi, India, from January to October 2021: a repeated cross-sectional analysis
- Pragya Sharma, Saurav Basu, Suruchi Mishra, Mongjam Meghachandra Singh
- Osong Public Health Res Perspect. 2022;13(3):184-190. Published online June 10, 2022
- DOI: https://doi.org/10.24171/j.phrp.2022.0014
- 5,154 View
- 77 Download
- 3 Web of Science
- 3 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 
- Objectives
The aim of this study was to assess changes in the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) immunoglobulin G (IgG) seroprevalence among children and adolescents in Delhi, India from January 2021 to October 2021. Methods: This was a repeated cross-sectional analysis of participants aged 5 to 17 years from 2 SARS-CoV-2 seroprevalence surveys conducted in Delhi, India during January 2021 and September to October 2021. Anti-SARS-CoV-2 IgG antibodies were detected by using the VITROS assay (90% sensitivity, 100% specificity). Results: The seroprevalence among 5- to 17-year-old school-age children and adolescents increased from 52.8% (95% confidence interval [CI], 51.3%−54.3%) in January 2021 to 81.8% (95% CI, 80.9%−82.6%) in September to October 2021. The assay-adjusted seroprevalence was 90.8% (95% CI, 89.8%−91.7%). Seropositivity positively correlated with participants’ age (p<0.001), but not sex (p=0.388). A signal to cut-off ratio ≥4.00, correlating with the presence of neutralization antibodies, was observed in 4,814 (57.9%) participants. Conclusion: The high percentage of seroconversion among children and adolescents indicates the presence of natural infection-induced immunity from past exposure to the SARS-CoV-2 virus. However, the lack of hybrid immunity and the concomitant likelihood of lower levels of neutralization antibodies than in adults due to the absence of vaccination warrants careful monitoring and surveillance of infection risk and disease severity from newer and emergent variants. -
Citations
Citations to this article as recorded by- Severe Acute Hepatitis of Unknown Etiology Presenting as Pediatric Acute Liver Failure: Analysis of Likely Etiology, Clinical Course and Outcome
Bikrant B. Lal, Vikrant Sood, Ekta Gupta, Reshu Agarwal, Rajeev Khanna, Seema Alam
Journal of Clinical and Experimental Hepatology.2023; 13(5): 912. CrossRef - Anti-SARS-CoV-2 antibody kinetics up to 6 months of follow-up: Result from a nation-wide population-based, age stratified sero-epidemiological prospective cohort study in India
Puneet Misra, Arvind Kumar Singh, Baijayantimala Mishra, Bijayini Behera, Binod Kumar Patro, Guruprasad R. Medigeshi, Hari Shanker Joshi, Mohammad Ahmad, Pradeep Kumar Chaturvedi, Palanivel Chinnakali, Partha Haldar, Mohan Bairwa, Pradeep Kharya, Rahul Dh
PLOS ONE.2023; 18(12): e0287807. CrossRef - Seroprevalence of SARS CoV-2 among children after the second surge (June 2021) in a rural district of South India: Findings and lessons from a population-based survey
Carolin Elizabeth George, Leeberk Raja Inbaraj, Shon Rajukutty, Roshni Florina Joan, Sangeetha Muthuraj, Sindhulina Chandrasingh
Frontiers in Pediatrics.2022;[Epub] CrossRef
- Severe Acute Hepatitis of Unknown Etiology Presenting as Pediatric Acute Liver Failure: Analysis of Likely Etiology, Clinical Course and Outcome
- Worldwide prevalence of fungal coinfections among COVID-19 patients: a comprehensive systematic review and meta-analysis
- Saber Soltani, Milad Zandi, Samireh Faramarzi, Ramin Shahbahrami, Mohebat Vali, Sara Akhavan Rezayat, Reza Pakzad, Pooneh Malekifar, Iraj Pakzad, Neda Jahandoost, Jalal Moludi
- Osong Public Health Res Perspect. 2022;13(1):15-23. Published online February 8, 2022
- DOI: https://doi.org/10.24171/j.phrp.2021.0293
- 7,456 View
- 117 Download
- 5 Web of Science
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Microbial coinfections can increase the morbidity and mortality rates of viral respiratory diseases. Therefore, this study aimed to determine the pooled prevalence of fungal coinfections in coronavirus disease 2019 (COVID-19) patients. Web of Science, Medline, Scopus, and Embase were searched without language restrictions to identify the related research on COVID-19 patients with fungal coinfections from December 1, 2019, to December 30, 2020. A random-effects model was used for analysis. The sample size included 2,246 patients from 8 studies. The pooled prevalence of fungal coinfections was 12.60%. The frequency of fungal subtype coinfections was 3.71% for Aspergillus, 2.39% for Candida, and 0.39% for other. The World Health Organization’s Regional Office for Europe and Regional Office for Southeast Asia had the highest (23.28%) and lowest (4.53%) estimated prevalence of fungal coinfection, respectively. Our findings showed a high prevalence of fungal coinfections in COVID-19 cases, which is a likely contributor to mortality in COVID-19 patients. Early identification of fungal pathogens in the laboratory for COVID-19 patients can lead to timely treatment and prevention of further damage by this hidden infection.
- Prevalence of plasmid-mediated AmpC β-lactamases among uropathogenic Escherichia coli isolates in southwestern Iran
- Nabi Jomehzadeh, Khadijeh Ahmadi, Zahra Rahmani
- Osong Public Health Res Perspect. 2021;12(6):390-395. Published online December 1, 2021
- DOI: https://doi.org/10.24171/j.phrp.2021.0272
- 4,935 View
- 90 Download
- 5 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
This study was undertaken to evaluate AmpC β-lactamase-producing Escherichia coli urine isolates and to characterize the frequency of plasmid-mediated AmpC (pAmpC)-encoding genes.
Methods
Antimicrobial susceptibility tests were performed using the disk diffusion technique. AmpC β-lactamase production was assessed with a phenotypic inhibitor-based method. The presence of 6 pAmpC-encoding cluster genes was detected by multiplex polymerase chain reaction (PCR).
Results
The proportion of antibiotic resistance of E. coli isolates ranged from 7.4% to 90.5%, and more than half (51.6%) of the total isolates were multidrug-resistant (MDR). Among the 95 E. coli isolates, 60 (63.2%) were found to be cefoxitin-resistant, but only 14 (14.7%) isolates were confirmed as AmpC β-lactamase-producers. In the PCR assay, pAmpC-encoding genes were found in 15 (15.8%) isolates, and blaDHA was the most prevalent type. However, blaFOX, blaMOX, and blaACC genes were not detected in the isolates.
Conclusion
Our findings contributed valuable information concerning antibiotic resistance, confirmatory phenotypic testing for AmpC production, and pAmpC β-lactamase gene content in E. coli isolates in southwestern Iran. The level of MDR recorded in AmpC-producing strains of this study was worrying; therefore, implementing strong infection control approaches to reduce the MDR burden is recommended. -
Citations
Citations to this article as recorded by- A review of the mechanisms that confer antibiotic resistance in pathotypes of E. coli
Sina Nasrollahian, Jay P. Graham, Mehrdad Halaji
Frontiers in Cellular and Infection Microbiology.2024;[Epub] CrossRef - Association Between Uropathogenic Escherichia coli Virulence Genes and Severity of Infection and Resistance to Antibiotics
Sofía Alejandra Fonseca-Martínez, Ruth Aralí Martínez-Vega, Ana Elvira Farfán-García, Clara Isabel González Rugeles, Libeth Yajaira Criado-Guerrero
Infection and Drug Resistance.2023; Volume 16: 3707. CrossRef - Extended-spectrum β-lactamases producing Enterobacteriaceae (ESBL-PE) prevalence in Nepal: A systematic review and meta-analysis
Christina Khadka, Manita Shyaula, Gopiram Syangtan, Shrijana Bista, Reshma Tuladhar, Anjana Singh, Dev Raj Joshi, Lok R. Pokhrel, Prabin Dawadi
Science of The Total Environment.2023; 901: 166164. CrossRef - Prevalence of Extended-Spectrum β-Lactamase-Resistant Genes in Escherichia coli Isolates from Central China during 2016–2019
Zui Wang, Qin Lu, Xiaohui Mao, Li Li, Junfeng Dou, Qigai He, Huabin Shao, Qingping Luo
Animals.2022; 12(22): 3191. CrossRef - Molecular detection and characterization of Shigella spp. harboring extended-spectrum β-lactamase genes in children with diarrhea in northwest Iran
Sahar Sabour, Amir Teimourpour, Jafar Mohammadshahi, Hadi Peeridogaheh, Roghayeh Teimourpour, Taher Azimi, Zahra Hosseinali
Molecular and Cellular Pediatrics.2022;[Epub] CrossRef - Plasmid-mediated AmpC β-Lactamase gene analysis in Klebsiella Pneumoniae clinical isolates
Nabi Jomehzadeh, Khadijeh Ahmadi, Hasti Shaabaninejad, Gholamali Eslami
Biomedical and Biotechnology Research Journal (BBR.2022; 6(4): 582. CrossRef
- A review of the mechanisms that confer antibiotic resistance in pathotypes of E. coli
- The laboratory test procedure to confirm rotavirus vaccine infection in severe complex immunodeficiency patients
- Su-Jin Chae, Seung-Rye Cho, Wooyoung Choi, Myung-Guk Han, Deog-Yong Lee
- Osong Public Health Res Perspect. 2021;12(4):269-273. Published online August 13, 2021
- DOI: https://doi.org/10.24171/j.phrp.2021.0079
- 4,573 View
- 85 Download
-
 Abstract
Abstract
 PDF
PDF - The rotavirus vaccine is a live vaccine, and there is a possibility of infection by the virus strain used in the vaccine. We investigated the process of determining whether an infection was caused by the vaccine strain in a severe complex immunodeficiency (SCID) patient with rotavirus infection. The patient was vaccinated with RotaTeq prior to being diagnosed with SCID. The testing process was conducted in the following order: confirming rotavirus infection, determining its genotype, and confirming the vaccine strain. Rotavirus infection was confirmed through enzyme immunoassay and VP6 gene detection. G1 and P[8] were identified by multiplex polymerase chain reaction for the genotype, and G3 was further identified using a single primer. By detecting the fingerprint gene (WC3) of RotaTeq, it was confirmed that the detected virus was the vaccine strain. Genotypes G1 and P[8] were identified, and the infection was suspected of having been caused by rotavirus G1P[8]. G1P[8] is the most commonly detected genotype worldwide and is not included in the recombinant strains used in vaccines. Therefore, the infection was confirmed to have been caused by the vaccine strain by analyzing the genetic relationship between VP4 and VP7. Rotavirus infection by the vaccine strain can be identified through genotyping and fingerprint gene detection. However, genetic linkage analysis will also help to identify vaccine strains.
- Detection of Novel Coronavirus on the Surface of Environmental Materials Contaminated by COVID-19 Patients in the Republic of Korea
- Sang-Eun Lee, Deog-Yong Lee, Wook-Gyo Lee, ByeongHak Kang, Yoon Suk Jang, Boyeong Ryu, SeungJae Lee, Hyunjung Bahk, Eungyu Lee
- Osong Public Health Res Perspect. 2020;11(3):128-132. Published online May 8, 2020
- DOI: https://doi.org/10.24171/j.phrp.2020.11.3.03
- 8,817 View
- 280 Download
- 45 Web of Science
- 22 Crossref
-
 Abstract
Abstract
 PDF
PDF This study aimed to determine the presence of SARS-CoV-2 on surfaces frequently touched by COVID-19 patients, and assess the scope of contamination and transmissibility in facilities where the outbreaks occurred. In the course of this epidemiological investigation, a total of 80 environmental specimens were collected from 6 hospitals (68 specimens) and 2 “mass facilities” (6 specimens from a rehabilitation center and 6 specimens from an apartment building complex). Specific reverse transcriptase-polymerase chain reaction targeting of RNA-dependent RNA polymerase, and envelope genes, were used to identify the presence of this novel coronavirus. The 68 specimens from 6 hospitals (A, B, C, D, E, and G), where prior disinfection/cleaning had been performed before environmental sampling, tested negative for SARS-CoV-2. However, 2 out of 12 specimens (16.7%) from 2 “mass facilities” (F and H), where prior disinfection/cleaning had not taken place, were positive for SARS-CoV-2 RNA polymerase, and envelope genes. These results suggest that prompt disinfection and cleaning of potentially contaminated surfaces is an effective infection control measure. By inactivating SARS-CoV-2 with disinfection/cleaning the infectivity and transmission of the virus is blocked. This investigation of environmental sampling may help in the understanding of risk assessment of the COVID-19 outbreak in “mass facilities” and provide guidance in using effective disinfectants on contaminated surfaces.
-
Citations
Citations to this article as recorded by- Assessing the impact of architectural and behavioral interventions for controlling indoor COVID-19 infection risk: An agent-based approach
Anxiao Zhang, Qi Zhen, Chi Zheng, Jing Li, Yue Zheng, Yiming Du, Qiong Huang, Qi Zhang
Journal of Building Engineering.2023; 74: 106807. CrossRef - Advancements in COVID-19 Testing: An In-depth Overview
Rajesh Kumar, Seetha Harilal, Abdullah G. Al-Sehemi, Mehboobali Pannipara, Githa Elizabeth Mathew, Bijo Mathew
Current Pharmaceutical Biotechnology.2023; 24(9): 1122. CrossRef - Coronavirus disease 2019 (COVID-19) research agenda for healthcare epidemiology
Lona Mody, Ibukunoluwa C. Akinboyo, Hilary M. Babcock, Werner E. Bischoff, Vincent Chi-Chung Cheng, Kathleen Chiotos, Kimberly C. Claeys, K. C. Coffey, Daniel J. Diekema, Curtis J. Donskey, Katherine D. Ellingson, Heather M. Gilmartin, Shruti K. Gohil, An
Infection Control & Hospital Epidemiology.2022; 43(2): 156. CrossRef - SARS-CoV-2 on Surfaces and HVAC Filters in Dormitory Rooms
Jin Pan, Seth A. Hawks, Aaron J. Prussin, Nisha K. Duggal, Linsey C. Marr
Environmental Science & Technology Letters.2022; 9(1): 71. CrossRef - COVID-19 Cluster Linked to Aerosol Transmission of SARS-CoV-2 via Floor Drains
Taewon Han, Heedo Park, Yungje Jeong, Jungmin Lee, Eungyeong Shon, Man-Seong Park, Minki Sung
The Journal of Infectious Diseases.2022; 225(9): 1554. CrossRef - Environmental Contamination with SARS-CoV-2 in Hospital COVID Department: Antigen Test, Real-Time RT-PCR and Virus Isolation
Urška Rozman, Lea Knez, Goran Novak, Jernej Golob, Anita Pulko, Mojca Cimerman, Matjaž Ocepek, Urška Kuhar, Sonja Šostar Turk
COVID.2022; 2(8): 1050. CrossRef - Using Environmental Sampling to Enable Zoonotic Pandemic Preparedness
Avirup Sanyal, Sanskriti Agarwal, Uma Ramakrishnan, Kritika M. Garg, Balaji Chattopadhyay
Journal of the Indian Institute of Science.2022; 102(2): 711. CrossRef - Anforderungen an die Hygiene bei der Reinigung und Desinfektion von Flächen
Bundesgesundheitsblatt - Gesundheitsforschung - Ge.2022; 65(10): 1074. CrossRef - SARS-CoV-2 pandemic: a review of molecular diagnostic tools including sample collection and commercial response with associated advantages and limitations
Harikrishnan Jayamohan, Christopher J. Lambert, Himanshu J. Sant, Alexander Jafek, Dhruv Patel, Haidong Feng, Michael Beeman, Tawsif Mahmood, Ugochukwu Nze, Bruce K. Gale
Analytical and Bioanalytical Chemistry.2021; 413(1): 49. CrossRef - Contamination of inert surfaces by SARS-CoV-2: Persistence, stability and infectivity. A review
Montse Marquès, José L. Domingo
Environmental Research.2021; 193: 110559. CrossRef - A Systematic Review of Surface Contamination, Stability, and Disinfection Data on SARS-CoV-2 (Through July 10, 2020)
Noah Bedrosian, Elizabeth Mitchell, Elsa Rohm, Miguel Rothe, Christine Kelly, Gabrielle String, Daniele Lantagne
Environmental Science & Technology.2021; 55(7): 4162. CrossRef - Transmission of Severe Acute Respiratory Syndrome Coronavirus 2 via Contaminated Surfaces: What Is to Be Done?
Craig S Conover
Clinical Infectious Diseases.2021; 72(11): 2062. CrossRef - Investigation of SARS CoV-2 virus in environmental surface
Abdollah Dargahi, Farhad Jeddi, Mehdi Vosoughi, Chiman Karami, Aidin Hadisi, S. Ahamad Mokhtari, Hasan Ghobadi, Morteza Alighadri, Somayeh Biparva Haghighi, Hadi Sadeghi
Environmental Research.2021; 195: 110765. CrossRef - Ist die Desinfektion öffentlicher Flächen zur Prävention von SARS-CoV-2 – infektionen sinnvoll?
Günter Kampf, Lutz Jatzwauk
Das Gesundheitswesen.2021; 83(03): 180. CrossRef - SARS-CoV-2 Detection Rates from Surface Samples Do Not Implicate Public Surfaces as Relevant Sources for Transmission
Günter Kampf, Stephanie Pfaender, Emanuel Goldman, Eike Steinmann
Hygiene.2021; 1(1): 24. CrossRef - The SARS-CoV-2 (COVID-19) pandemic in hospital: An insight into environmental surfaces contamination, disinfectants’ efficiency, and estimation of plastic waste production
Faezeh seif, Zahra Noorimotlagh, Seyyed Abbas Mirzaee, Mojtaba Kalantar, Barat Barati, Mahdi Emamian Fard, Nozar Kalantar Fard
Environmental Research.2021; 202: 111809. CrossRef - Prevalence of SARS-CoV-2 RNA on inanimate surfaces: a systematic review and meta-analysis
Simone Belluco, Marzia Mancin, Filippo Marzoli, Alessio Bortolami, Eva Mazzetto, Alessandra Pezzuto, Michela Favretti, Calogero Terregino, Francesco Bonfante, Roberto Piro
European Journal of Epidemiology.2021; 36(7): 685. CrossRef - Management following the first confirmed case of SARS-CoV-2 in a domestic cat associated with a massive outbreak in South Korea
Taewon Han, Boyeong Ryu, Suyeon Lee, Yugyeong Song, Yoongje Jeong, Ilhwan Kim, Jeongmin Kim, Eunjin Kim, Wonjun Lee, Hyunju Lee, Haekyoung Hwang
One Health.2021; 13: 100328. CrossRef - Non-Respiratory Droplet Transmission of COVID-19 in the Isolation Ward of a Secondary Hospital in Oman
Zayid K. Al Mayahi, Nawal Al Kindi, Nasser Al Shaqsi, Noaman Al Hattali, Azza Al Hattali, Khalid Salim, Mark Beatty
Infectious Diseases in Clinical Practice.2021; 29(6): e371. CrossRef - Effectiveness of antiviral metal and metal oxide thin-film coatings against human coronavirus 229E
Louis-Vincent Delumeau, Hatameh Asgarimoghaddam, Tamiru Alkie, Alexander James Bryan Jones, Samantha Lum, Kissan Mistry, Marc G. Aucoin, Stephanie DeWitte-Orr, Kevin P. Musselman
APL Materials.2021;[Epub] CrossRef - Rapid Review of SARS-CoV-1 and SARS-CoV-2 Viability, Susceptibility to Treatment, and the Disinfection and Reuse of PPE, Particularly Filtering Facepiece Respirators
José G. B. Derraik, William A. Anderson, Elizabeth A. Connelly, Yvonne C. Anderson
International Journal of Environmental Research an.2020; 17(17): 6117. CrossRef - Potential sources, modes of transmission and effectiveness of prevention measures against SARS-CoV-2
G. Kampf, Y. Brüggemann, H.E.J. Kaba, J. Steinmann, S. Pfaender, S. Scheithauer, E. Steinmann
Journal of Hospital Infection.2020; 106(4): 678. CrossRef
- Assessing the impact of architectural and behavioral interventions for controlling indoor COVID-19 infection risk: An agent-based approach
- Contact Transmission of COVID-19 in South Korea: Novel Investigation Techniques for Tracing Contacts
- Osong Public Health Res Perspect. 2020;11(1):60-63. Published online February 28, 2020
- DOI: https://doi.org/10.24171/j.phrp.2020.11.1.09
- 45,194 View
- 1,051 Download
- 120 Web of Science
- 115 Crossref
-
 Abstract
Abstract
 PDF
PDF In the epidemiological investigation of an infectious disease, investigating, classifying, tracking, and managing contacts by identifying the patient’s route are important for preventing further transmission of the disease. However, omissions and errors in previous activities can occur when the investigation is performed through only a proxy interview with the patient. To overcome these limitations, methods that can objectively verify the patient’s claims (medical facility records, Global Positioning System, card transactions, and closed-circuit television) were used for the recent ongoing coronavirus disease 2019 contact investigations in South Korea.
-
Citations
Citations to this article as recorded by- Privacy risk in contact tracing systems
Janine L. Spears, Ali Padyab
Behaviour & Information Technology.2023; 42(2): 174. CrossRef - The role of data platforms in COVID-19 crisis: a smart city perspective
Laura-Diana Radu, Daniela Popescul
Aslib Journal of Information Management.2023; 75(6): 1033. CrossRef - Feasibility of digital contact tracing in low-income settings – pilot trial for a location-based DCT app
Eric Handmann, Sia Wata Camanor, Mosoka P. Fallah, Neima Candy, Davidetta Parker, André Gries, Thomas Grünewald
BMC Public Health.2023;[Epub] CrossRef - Incidence of rheumatic diseases during the COVID-19 pandemic in South Korea
Soo Min Ahn, Seongho Eun, Sunghwan Ji, Seokchan Hong, Chang-Keun Lee, Bin Yoo, Ji Seon Oh, Yong-Gil Kim
The Korean Journal of Internal Medicine.2023; 38(2): 248. CrossRef - SARS-CoV-2 molecular diagnostic point-of-care testing based on loop-mediated isothermal amplification: A prospective, single-center validation study
Sung Hun Moon, Sang-Chul Kim, Byung Woo Kim, Gwan-Jin Park, Hyun-Seok Chai, Young Min Kim, Hee Sung Kim, Hee Sue Park
Heliyon.2023; 9(3): e14564. CrossRef - Contact Tracing With District-Based Trajectories
Kiki Adhinugraha, Wenny Rahayu, Nasser Allheeib
International Journal of Data Warehousing and Mini.2023; 19(1): 1. CrossRef - La pandemia de COVID-19 en Brasil: epidemiología e impactos del negacionismo
Pedro Rodrigues Curi Hallal, Bruno Pereira Nunes
Revista de Estudios Brasileños.2023; 9(19): 15. CrossRef - Identification and comparison of pandemic-to-symptom networks of South Korea and the United States
Mijeong Park, Deachul Seo, Ji Geun Kim, Gayeon Lee, Larkin S. McReynolds, Lawrence Amsel, Hyunjung Yang, Young-Hoon Kim, Sanghoon Han, Soo Hyun Park, Juyoen Hur
Frontiers in Psychiatry.2023;[Epub] CrossRef - Detecting mpox infection in the early epidemic: an epidemiologic investigation of the third and fourth cases in Korea
Taeyoung Kim, Eonjoo Park, Jun Suk Eun, Eun-young Lee, Ji Won Mun, Yunsang Choi, Shinyoung Lee, Hansol Yeom, Eunkyoung Kim, Jongmu Kim, Jihyun Choi, Jinho Ha, Sookkyung Park
Epidemiology and Health.2023; 45: e2023040. CrossRef - COVID-19 conscience tracing: mapping the moral distances of coronavirus
David Shaw
Journal of Medical Ethics.2022; 48(8): 530. CrossRef - Bio-safety and bio-security: A major global concern for ongoing COVID-19 pandemic
Saud Ali Al Shehri, AM Al-Sulaiman, Sarfuddin Azmi, Sultan S. Alshehri
Saudi Journal of Biological Sciences.2022; 29(1): 132. CrossRef - Perceived sources of occupational burn-out and embitterment among front-line health workers for COVID-19 control in Gyeonggi province, South Korea: a qualitative study
Bee-Ah Kang, Sijoung Kwon, Myoungsoon You, Heeyoung Lee
Occupational and Environmental Medicine.2022; 79(4): 245. CrossRef - COVID-19 vaccine willingness and hesitancy among residents in Qatar: a quantitative analysis based on machine learning
Muhammad Hafizh, Yousif Badri, Sakib Mahmud, Amir Hafez, Pilsung Choe
Journal of Human Behavior in the Social Environmen.2022; 32(7): 899. CrossRef - A resposta da Coreia do Sul à pandemia de COVID-19: lições aprendidas e recomendações a gestores
Thais Regis Aranha Rossi, Catharina Leite Matos Soares, Gerluce Alves Silva, Jairnilson Silva Paim, Lígia Maria Vieira-da-Silva
Cadernos de Saúde Pública.2022;[Epub] CrossRef - Self-Injurious Behavior Rate in the Short-Term Period of the COVID-19 Pandemic in Korea
Se Jin Park, Soo Jung Rim, Minkyung Jo, Min Geu Lee, Gyurin Kim, Subin Park
Journal of Korean Medical Science.2022;[Epub] CrossRef - Cost-effectiveness of interventions for the prevention and control of COVID-19: Systematic review of 85 modelling studies
Lihui Zhou, Wenxin Yan, Shu Li, Hongxi Yang, Xinyu Zhang, Wenli Lu, Jue Liu, Yaogang Wang
Journal of Global Health.2022;[Epub] CrossRef - Artificial Intelligence and Internet of Things (AI-IoT) Technologies in Response to COVID-19 Pandemic: A Systematic Review
Junaid Iqbal Khan, Jebran Khan, Furqan Ali, Farman Ullah, Jamshid Bacha, Sungchang Lee
IEEE Access.2022; 10: 62613. CrossRef - An Experience of the Early Stage of COVID-19 Outbreak in Nursing Homes in Gyeonggi Province, Korea
Gawon Choi, Na-young Kim, Seon-young Lee, Hae Deun Noh, Heeyoung Lee
Korean Journal of Clinical Geriatrics.2022; 23(1): 27. CrossRef - Likely community transmission of COVID-19 infections between neighboring, persistent hotspots in Ontario, Canada
Eliseos J. Mucaki, Ben C. Shirley, Peter K. Rogan
F1000Research.2022; 10: 1312. CrossRef - Unwillingness to cooperate with COVID-19 contact tracing in Japan
M. Machida, H. Kikuchi, T. Kojima, I. Nakamura, R. Saito, T. Nakaya, T. Hanibuchi, T. Takamiya, Y. Odagiri, N. Fukushima, S. Amagasa, H. Watanabe, S. Inoue
Public Health.2022; 210: 34. CrossRef - The effectiveness of COVID-19 testing and contact tracing in a US city
Xutong Wang, Zhanwei Du, Emily James, Spencer J. Fox, Michael Lachmann, Lauren Ancel Meyers, Darlene Bhavnani
Proceedings of the National Academy of Sciences.2022;[Epub] CrossRef - Contact Tracing Strategies for COVID-19 Prevention and Containment: A Scoping Review
Bolanle Adefowoke Ojokoh, Benjamin Aribisala, Oluwafemi A. Sarumi, Arome Junior Gabriel, Olatunji Omisore, Abiola Ezekiel Taiwo, Tobore Igbe, Uchechukwu Madukaku Chukwuocha, Tunde Yusuf, Abimbola Afolayan, Olusola Babalola, Tolulope Adebayo, Olaitan Afola
Big Data and Cognitive Computing.2022; 6(4): 111. CrossRef - Epidemiology and Outcome of Out-of-Hospital Cardiac Arrests during the COVID-19 Pandemic in South Korea: A Systematic Review and Meta-Analyses
Jae Hwan Kim, Chiwon Ahn, Myeong Namgung
Yonsei Medical Journal.2022; 63(12): 1121. CrossRef - Perceived barriers to the process of COVID-19 control among frontline healthcare workers in South Korea: a qualitative study
Sijoung Kwon, Bee-Ah Kang, Myoungsoon You, Heeyoung Lee
BMJ Open.2022; 12(12): e063899. CrossRef - Response System for and Epidemiological Features of COVID-19 in Gyeongsangnam-do Province in South Korea
Yu Mi Wi, Su Jin Lim, Si-Ho Kim, Seungjin Lim, Su Jin Lee, Byung-Han Ryu, Sun In Hong, Oh-Hyun Cho, Kyunglan Moon, Kyung-Wook Hong, Sunjoo Kim, In-Gyu Bae
Clinical Infectious Diseases.2021; 72(4): 661. CrossRef - Impact of Public Health Interventions on Seasonal Influenza Activity During the COVID-19 Outbreak in Korea
Hyunju Lee, Heeyoung Lee, Kyoung-Ho Song, Eu Suk Kim, Jeong Su Park, Jongtak Jung, Soyeon Ahn, Eun Kyeong Jeong, Hyekyung Park, Hong Bin Kim
Clinical Infectious Diseases.2021; 73(1): e132. CrossRef - The utility of video technology and enhanced infection control in reducing COVID-19 disease burden in a custodial setting
Larissa H Unruh, Sadhana Dharmapuri, Kenneth Soyemi
American Journal of Infection Control.2021; 49(6): 852. CrossRef - Will the COVID-19 pandemic boost access to personal health care records? Smartphone data access to tackle the modern pandemic
Charles Edmund Breeze, Charlotte Murkin, Matt Lechner
BMJ Innovations.2021; 7(1): 243. CrossRef - Spatial variability in reproduction number and doubling time across two waves of the COVID-19 pandemic in South Korea, February to July, 2020
Eunha Shim, Amna Tariq, Gerardo Chowell
International Journal of Infectious Diseases.2021; 102: 1. CrossRef - The experience of contact tracing in Singapore in the control of COVID-19: highlighting the use of digital technology
Sean Han Sheng Lai, Camelia Qian Ying Tang, Asok Kurup, Gowreeson Thevendran
International Orthopaedics.2021; 45(1): 65. CrossRef - Structural Racism in the COVID-19 Pandemic: Moving Forward
Maya Sabatello, Mary Jackson Scroggins, Greta Goto, Alicia Santiago, Alma McCormick, Kimberly Jacoby Morris, Christina R. Daulton, Carla L. Easter, Gwen Darien
The American Journal of Bioethics.2021; 21(3): 56. CrossRef - Privacy concerns can explain unwillingness to download and use contact tracing apps when COVID-19 concerns are high
Eugene Y. Chan, Najam U. Saqib
Computers in Human Behavior.2021; 119: 106718. CrossRef - Reduction in mobility and COVID-19 transmission
Pierre Nouvellet, Sangeeta Bhatia, Anne Cori, Kylie E. C. Ainslie, Marc Baguelin, Samir Bhatt, Adhiratha Boonyasiri, Nicholas F. Brazeau, Lorenzo Cattarino, Laura V. Cooper, Helen Coupland, Zulma M. Cucunuba, Gina Cuomo-Dannenburg, Amy Dighe, Bimandra A.
Nature Communications.2021;[Epub] CrossRef - State of the Art in Adoption of Contact Tracing Apps and Recommendations Regarding Privacy Protection and Public Health: Systematic Review
Katarzyna Kolasa, Francesca Mazzi, Ewa Leszczuk-Czubkowska, Zsombor Zrubka, Márta Péntek
JMIR mHealth and uHealth.2021; 9(6): e23250. CrossRef - Genomic investigation of the coronavirus disease-2019 outbreak in the Republic of Korea
Jeong-Min Kim, Sung Yong Park, Daesang Lee, Jun-Sub Kim, Youngjoon Park, Jin Gwack, Mi Young Kim, Dong Hyun Song, Seong Tae Jeong, Yoon-Seok Chung, Cheon Kwon Yoo, Ha Youn Lee, Myung-Guk Han
Scientific Reports.2021;[Epub] CrossRef - Test, Trace, and Put on the Blockchain?: A Viewpoint Evaluating the Use of Decentralized Systems for Algorithmic Contact Tracing to Combat a Global Pandemic
Moritz Platt, Anton Hasselgren, Juan Manuel Román-Belmonte, Marcela Tuler de Oliveira, Hortensia De la Corte-Rodríguez, Sílvia Delgado Olabarriaga, E Carlos Rodríguez-Merchán, Tim Ken Mackey
JMIR Public Health and Surveillance.2021; 7(4): e26460. CrossRef - Decrease in hospital admissions for respiratory diseases during the COVID-19 pandemic: a nationwide claims study
Kyungmin Huh, Young-Eun Kim, Wonjun Ji, Dong Wook Kim, Eun-Joo Lee, Jong-Hun Kim, Ji-Man Kang, Jaehun Jung
Thorax.2021; 76(9): 939. CrossRef - A simple model for the total number of SARS-CoV-2 infections on a national level
N. Blanco, K. A. Stafford, M. C. Lavoie, A. Brandenburg, M. W. Górna, M. Merski
Epidemiology and Infection.2021;[Epub] CrossRef - Malaysia’s Health Systems Response to COVID-19
Zen Yang Ang, Kit Yee Cheah, Md. Sharif Shakirah, Weng Hong Fun, Jailani Anis-Syakira, Yuke-Lin Kong, Sondi Sararaks
International Journal of Environmental Research an.2021; 18(21): 11109. CrossRef - Managing Pandemics with Health Informatics: Successes and Challenges
Mujeeb A. Basit, Christoph U. Lehmann, Richard J. Medford
Yearbook of Medical Informatics.2021; 30(01): 017. CrossRef - When robots contribute to eradicate the COVID-19 spread in a context of containment
Naila Aziza Houacine, Habiba Drias
Progress in Artificial Intelligence.2021; 10(4): 391. CrossRef - Best Practice Guidance for Digital Contact Tracing Apps: A Cross-disciplinary Review of the Literature
James O'Connell, Manzar Abbas, Sarah Beecham, Jim Buckley, Muslim Chochlov, Brian Fitzgerald, Liam Glynn, Kevin Johnson, John Laffey, Bairbre McNicholas, Bashar Nuseibeh, Michael O'Callaghan, Ian O'Keeffe, Abdul Razzaq, Kaavya Rekanar, Ita Richardson, And
JMIR mHealth and uHealth.2021; 9(6): e27753. CrossRef - Implementing Public Health Strategies—The Need for Educational Initiatives: A Systematic Review
Amir Khorram-Manesh, Maxim A. Dulebenets, Krzysztof Goniewicz
International Journal of Environmental Research an.2021; 18(11): 5888. CrossRef - Lessons from non-pharmaceutical interventions on the first wave of COVID-19 in the Asia Pacific region
Dongil Ahn
Journal of Global Health Science.2021;[Epub] CrossRef - Modeling the early temporal dynamics of viral load in respiratory tract specimens of COVID-19 patients in Incheon, the Republic of Korea
Ah-Young Lim, Hae-Kwan Cheong, Yoon Ju Oh, Jae Kap Lee, Jae Bum So, Hyun Jin Kim, Boram Han, Sung Won Park, Yongsun Jang, Chang Yong Yoon, Yun Ok Park, Jong-Hun Kim, Jin Yong Kim
International Journal of Infectious Diseases.2021; 108: 428. CrossRef - Contact Tracing Apps: Lessons Learned on Privacy, Autonomy, and the Need for Detailed and Thoughtful Implementation
Katie Hogan, Briana Macedo, Venkata Macha, Arko Barman, Xiaoqian Jiang
JMIR Medical Informatics.2021; 9(7): e27449. CrossRef - Using Mobile Phone Data to Estimate the Relationship between Population Flow and Influenza Infection Pathways
Qiushi Chen, Michiko Tsubaki, Yasuhiro Minami, Kazutoshi Fujibayashi, Tetsuro Yumoto, Junzo Kamei, Yuka Yamada, Hidenori Kominato, Hideki Oono, Toshio Naito
International Journal of Environmental Research an.2021; 18(14): 7439. CrossRef - Effective COVID-19 Control: A Comparative Analysis of the Stringency and Timeliness of Government Responses in Asia
Shu Chen, Lei Guo, Taghred Alghaith, Di Dong, Mohammed Alluhidan, Mariam M. Hamza, Christopher H. Herbst, Xinqi Zhang, Gabrielle Charis Alano Tagtag, Yi Zhang, Nahar Alazemi, Rana Saber, Reem Alsukait, Shenglan Tang
International Journal of Environmental Research an.2021; 18(16): 8686. CrossRef - Analysis of the factors affecting the adoption and compliance of the NHS COVID-19 mobile application: a national cross-sectional survey in England
Marcus Panchal, Sukhpreet Singh, Esther Rodriguez-Villegas
BMJ Open.2021; 11(8): e053395. CrossRef - Management of the COVID-19 Pandemic in the Republic of Korea from the Perspective of Governance and Public-Private Partnership
Woojin Kim, Tae Yong Jung, Susann Roth, Woochong Um, Changsoo Kim
Yonsei Medical Journal.2021; 62(9): 777. CrossRef - Pilot Evaluations of Two Bluetooth Contact Tracing Approaches on a University Campus: Mixed Methods Study
Tyler Shelby, Tyler Caruthers, Oren Y Kanner, Rebecca Schneider, Dana Lipnickas, Lauretta E Grau, Rajit Manohar, Linda Niccolai
JMIR Formative Research.2021; 5(10): e31086. CrossRef - Efficient Contact Tracing for pandemics using blockchain
Nida Bari, Usman Qamar, Ayesha Khalid
Informatics in Medicine Unlocked.2021; 26: 100742. CrossRef - Policy Review and Modeling Analysis of Mitigation Measures for Coronavirus Disease Epidemic Control, Health System, and Disease Burden, South Korea
Hae-Young Kim, In-Hwan Oh, Jacob Lee, Jeong-Yeon Seon, Woo-Hwi Jeon, Jae Seok Park, Sung-Il Nam, Niket Thakkar, Prashanth Selvaraj, Jessica McGillen, Daniel Klein, Scott Braithwaite, Anna Bershteyn, Seung Heon Lee
Emerging Infectious Diseases.2021;[Epub] CrossRef - Experiences and Lessons Learned from COVID-19 Pandemic Management in South Korea and the V4 Countries
Gergő Túri, Attila Virág
Tropical Medicine and Infectious Disease.2021; 6(4): 201. CrossRef - Likely community transmission of COVID-19 infections between neighboring, persistent hotspots in Ontario, Canada
Eliseos J. Mucaki, Ben C. Shirley, Peter K. Rogan
F1000Research.2021; 10: 1312. CrossRef - Cost-Effectiveness of Interventions for the Prevention and Control of COVID-19: A Systematic Review and Meta-Analysis
Lihui Zhou, Wenxin Yan, Shu Li, Hongxi Yang, Xinyu Zhang, Wenli Lu, Jue Liu, Yaogang WANG
SSRN Electronic Journal .2021;[Epub] CrossRef - Effectiveness for the Response to COVID-19: The MERS Outbreak Containment Procedures
Hae-Wol Cho
Osong Public Health and Research Perspectives.2020; 11(1): 1. CrossRef - COVID-19, Australia: Epidemiology Report 5: Reporting week ending 19:00 AEDT 29 February 2020
Olivia Williams
Communicable Diseases Intelligence.2020;[Epub] CrossRef - The global community needs to swiftly ramp up the response to contain COVID-19
Dale Fisher, Annelies Wilder-Smith
The Lancet.2020; 395(10230): 1109. CrossRef - Experts’ request to the Spanish Government: move Spain towards complete lockdown
Oriol Mitjà, Àlex Arenas, Xavier Rodó, Aurelio Tobias, Joe Brew, José M Benlloch
The Lancet.2020; 395(10231): 1193. CrossRef - Maximizing the Calm before the Storm: Tiered Surgical Response Plan for Novel Coronavirus (COVID-19)
Samuel Wade Ross, Cynthia W. Lauer, William S. Miles, John M. Green, Britton A Christmas, Addison K. May, Brent D. Matthews
Journal of the American College of Surgeons.2020; 230(6): 1080. CrossRef - Coronavirus Disease-19: Summary of 2,370 Contact Investigations of the First 30 Cases in the Republic of Korea
Osong Public Health and Research Perspectives.2020; 11(2): 81. CrossRef - Only strict quarantine measures can curb the coronavirus disease (COVID-19) outbreak in Italy, 2020
Henrik Sjödin, Annelies Wilder-Smith, Sarah Osman, Zia Farooq, Joacim Rocklöv
Eurosurveillance.2020;[Epub] CrossRef - Governance, technology and citizen behavior in pandemic: Lessons from COVID-19 in East Asia
Rajib Shaw, Yong-kyun Kim, Jinling Hua
Progress in Disaster Science.2020; 6: 100090. CrossRef - Sub-National Allocation of COVID-19 Tests: An Efficiency Criterion with an Application to Italian Regions
Christelle Baunez, Mickael Degoulet, Stephane Luchini, Patrick Pintus, Miriam Teschl
SSRN Electronic Journal .2020;[Epub] CrossRef - The COVID-19 pandemic: a moment for exposure science
Nicole C. Deziel, Joseph G. Allen, Paul T. J. Scheepers, Jonathan I. Levy
Journal of Exposure Science & Environmental Epidem.2020; 30(4): 591. CrossRef - National Response to COVID-19 in the Republic of Korea and Lessons Learned for Other Countries
Juhwan Oh, Jong-Koo Lee, Dan Schwarz, Hannah L. Ratcliffe, Jeffrey F. Markuns, Lisa R. Hirschhorn
Health Systems & Reform.2020;[Epub] CrossRef - Containing COVID-19 Among 627,386 Persons in Contact With the Diamond Princess Cruise Ship Passengers Who Disembarked in Taiwan: Big Data Analytics
Chi-Mai Chen, Hong-Wei Jyan, Shih-Chieh Chien, Hsiao-Hsuan Jen, Chen-Yang Hsu, Po-Chang Lee, Chun-Fu Lee, Yi-Ting Yang, Meng-Yu Chen, Li-Sheng Chen, Hsiu-Hsi Chen, Chang-Chuan Chan
Journal of Medical Internet Research.2020; 22(5): e19540. CrossRef - COVID-19 and MERS Infections in Healthcare Workers in Korea
Seong-Kyu Kang
Safety and Health at Work.2020; 11(2): 125. CrossRef - How we should respond to the Coronavirus SARS-CoV-2 outbreak: A German perspective
F. Jung, V. Krieger, F.T. Hufert, J.-H. Küpper
Clinical Hemorheology and Microcirculation.2020; 74(4): 363. CrossRef - WHAT HAS THE COVID-19 PANDEMIC TAUGHT US ABOUT ADOPTING PREVENTIVE MEASURES?
Adriana Cristina de Oliveira, Thabata Coaglio Lucas, Robert Aldo Iquiapaza
Texto & Contexto - Enfermagem.2020;[Epub] CrossRef - COVID-19: when should quarantine be enforced?
Chris T Bauch, Madhur Anand
The Lancet Infectious Diseases.2020; 20(9): 994. CrossRef - COVID-19–We urgently need to start developing an exit strategy
Eskild Petersen, Sean Wasserman, Shui-Shan Lee, Unyeong Go, Allison H. Holmes, Seif Al-Abri, Susan McLellan, Lucille Blumberg, Paul Tambyah
International Journal of Infectious Diseases.2020; 96: 233. CrossRef - COVID-19: the virus in the control of culture?
Lincoln Lopes Ferreira, Antonio Carlos P. Chagas, Wanderley M. Bernardo
Revista da Associação Médica Brasileira.2020; 66(3): 242. CrossRef - Evaluating How Smartphone Contact Tracing Technology Can Reduce the Spread of Infectious Diseases: The Case of COVID-19
Enrique Hernandez-Orallo, Pietro Manzoni, Carlos Tavares Calafate, Juan-Carlos Cano
IEEE Access.2020; 8: 99083. CrossRef - Development and Utilization of a Rapid and Accurate Epidemic Investigation Support System for COVID-19
Young Joon Park, Sang Yun Cho, Jin Lee, Ikjin Lee, Won-Ho Park, Seungmyeong Jeong, Seongyun Kim, Seokjun Lee, Jaeho Kim, Ok Park
Osong Public Health and Research Perspectives.2020; 11(3): 118. CrossRef - How could we improve the national projects in health and demography after coronavirus pandemic?
N. A. Avxentyev, V. S. Nazarov, N. N. Sisigina
Voprosy Ekonomiki.2020; (6): 22. CrossRef - Public Health Emergency and Crisis Management: Case Study of SARS-CoV-2 Outbreak
Hemin Choi, Wonhyuk Cho, Min-Hyu Kim, Joon-Young Hur
International Journal of Environmental Research an.2020; 17(11): 3984. CrossRef - COVID-19 data sources: evaluation of map applications and analysis of behavior changes in Europe’s population
Vít Pászto, Jaroslav Burian, Karel Macků
Geografie.2020; 125(2): 171. CrossRef - The impact of COVID-19 and strategies for mitigation and suppression in low- and middle-income countries
Patrick G. T. Walker, Charles Whittaker, Oliver J. Watson, Marc Baguelin, Peter Winskill, Arran Hamlet, Bimandra A. Djafaara, Zulma Cucunubá, Daniela Olivera Mesa, Will Green, Hayley Thompson, Shevanthi Nayagam, Kylie E. C. Ainslie, Sangeeta Bhatia, Samir
Science.2020; 369(6502): 413. CrossRef - Public health initiatives from hospitalized patients with COVID-19, China
Chenkai Zhao, Yueqin Xu, Xu Zhang, Yaping Zhong, Li Long, Wenzhi Zhan, Tingting Xu, Chen Zhan, Yuehan Chen, Jinghai Zhu, Wei Xiao, Miao He
Journal of Infection and Public Health.2020; 13(9): 1229. CrossRef - COVID-19 in South Korea
Jun Yong Choi
Postgraduate Medical Journal.2020; 96(1137): 399. CrossRef - COVID-19 Pandemic and Burden of Non-Communicable Diseases: An Ecological Study on Data of 185 Countries
M. Reza Azarpazhooh, Negar Morovatdar, Abolfazl Avan, Thanh G Phan, Afshin A. Divani, Nawaf Yassi, Saverio Stranges, Brian Silver, José Biller, Masoud Tokazebani Belasi, Sepideh Kazemi Neya, Bita Khorram, Asher Frydman, Yongchai Nilanont, Elisa Onorati, M
Journal of Stroke and Cerebrovascular Diseases.2020; 29(9): 105089. CrossRef - Effect of Underlying Comorbidities on the Infection and Severity of COVID-19 in Korea: a Nationwide Case-Control Study
Wonjun Ji, Kyungmin Huh, Minsun Kang, Jinwook Hong, Gi Hwan Bae, Rugyeom Lee, Yewon Na, Hyoseon Choi, Seon Yeong Gong, Yoon-Hyeong Choi, Kwang-Pil Ko, Jeong-Soo Im, Jaehun Jung
Journal of Korean Medical Science.2020;[Epub] CrossRef - Innovative countermeasures can maintain cancer care continuity during the coronavirus disease-2019 pandemic in Korea
Soohyeon Lee, Ah-reum Lim, Min Ja Kim, Yoon Ji Choi, Ju Won Kim, Kyong Hwa Park, Sang Won Shin, Yeul Hong Kim
European Journal of Cancer.2020; 136: 69. CrossRef - Role of Chest CT in Resource-Driven Healthcare Systems
Natalie L. Demirjian, Brandon K. K. Fields, Ali Gholamrezanezhad
American Journal of Roentgenology.2020; 215(3): W36. CrossRef - Contact Tracing during Coronavirus Disease Outbreak, South Korea, 2020
Young Joon Park, Young June Choe, Ok Park, Shin Young Park, Young-Man Kim, Jieun Kim, Sanghui Kweon, Yeonhee Woo, Jin Gwack, Seong Sun Kim, Jin Lee, Junghee Hyun, Boyeong Ryu, Yoon Suk Jang, Hwami Kim, Seung Hwan Shin, Seonju Yi, Sangeun Lee, Hee Kyoung K
Emerging Infectious Diseases.2020; 26(10): 2465. CrossRef - Health policy and leadership models during the COVID-19 pandemic: A review
Maria Nicola, Catrin Sohrabi, Ginimol Mathew, Ahmed Kerwan, Ahmed Al-Jabir, Michelle Griffin, Maliha Agha, Riaz Agha
International Journal of Surgery.2020; 81: 122. CrossRef - Lessons From South Korea’s Covid-19 Policy Response
Jongeun You
The American Review of Public Administration.2020; 50(6-7): 801. CrossRef - Nationwide Results of COVID-19 Contact Tracing in South Korea: Individual Participant Data From an Epidemiological Survey
Seung Won Lee, Woon Tak Yuh, Jee Myung Yang, Yoon-Sik Cho, In Kyung Yoo, Hyun Yong Koh, Dominic Marshall, Donghwan Oh, Eun Kyo Ha, Man Yong Han, Dong Keon Yon
JMIR Medical Informatics.2020; 8(8): e20992. CrossRef - The COVID-19 pandemic: critical issues and perspectives for infectious disease prevention in Africa
Ayodele Oluwaseun Ajayi
Infection Ecology & Epidemiology.2020;[Epub] CrossRef - COVID-19
Osakpolor Ogbebor, Zaw Min, Tariq Cheema, Nitin Bhanot
Critical Care Nursing Quarterly.2020; 43(4): 343. CrossRef Awareness of Health Professionals on COVID-19 and Factors Affecting It Before and During Index Case in North Shoa Zone, Ethiopia, 2020
Ayele Abebe, Abinet Mekuria, Awraris Balchut
Infection and Drug Resistance.2020; Volume 13: 2979. CrossRef- COVID-19: Weighing the Endeavors of Nations, with Time to Event Analysis
Shine Stephen, Alwin Issac, Jaison Jacob, VR Vijay, Rakesh Vadakkethil Radhakrishnan, Nadiya Krishnan
Osong Public Health and Research Perspectives.2020; 11(4): 149. CrossRef - Coronavirus Disease 2019 (COVID-19) diagnostic technologies: A country-based retrospective analysis of screening and containment procedures during the first wave of the pandemic
Brandon K.K. Fields, Natalie L. Demirjian, Ali Gholamrezanezhad
Clinical Imaging.2020; 67: 219. CrossRef - Journey to the East: COVID-19 Lessons From the East
Samuel S. Y. Wang
Asia Pacific Journal of Public Health.2020; 32(8): 513. CrossRef - COVID-19 healthcare demand and mortality in Sweden in response to non-pharmaceutical mitigation and suppression scenarios
Henrik Sjödin, Anders F Johansson, Åke Brännström, Zia Farooq, Hedi Katre Kriit, Annelies Wilder-Smith, Christofer Åström, Johan Thunberg, Mårten Söderquist, Joacim Rocklöv
International Journal of Epidemiology.2020; 49(5): 1443. CrossRef - Lessons learnt from easing COVID-19 restrictions: an analysis of countries and regions in Asia Pacific and Europe
Emeline Han, Melisa Mei Jin Tan, Eva Turk, Devi Sridhar, Gabriel M Leung, Kenji Shibuya, Nima Asgari, Juhwan Oh, Alberto L García-Basteiro, Johanna Hanefeld, Alex R Cook, Li Yang Hsu, Yik Ying Teo, David Heymann, Helen Clark, Martin McKee, Helena Legido-Q
The Lancet.2020; 396(10261): 1525. CrossRef - Natural outbreaks and bioterrorism: How to deal with the two sides of the same coin?
Lionel Koch, Anne-Aurelie Lopes, Avelina Maiguy, Sophie Guillier, Laurent Guillier, Jean-Nicolas Tournier, Fabrice Biot
Journal of Global Health.2020;[Epub] CrossRef - Retour d’expérience sur Covisan : un dispositif médicosocial pour casser les chaînes de transmission de la Covid-19
J. Pernet, H. de Bonnières, C. Breton, V. Hirsch, J.S. Molitor, D. Boutolleau, R. Piarroux, P. Hausfater
Annales françaises de médecine d’urgence.2020; 10(4-5): 306. CrossRef - Retour d’expérience sur la réorganisation d’un service d’urgence de centre hospitalo-universitaire en réponse à l’épidémie de Covid-19
M. Drogrey, J. Pernet, P. Hausfater
Annales françaises de médecine d’urgence.2020; 10(4-5): 233. CrossRef - Evaluating the Effectiveness of COVID-19 Bluetooth-Based Smartphone Contact Tracing Applications
Enrique Hernández-Orallo, Carlos T. Calafate, Juan-Carlos Cano, Pietro Manzoni
Applied Sciences.2020; 10(20): 7113. CrossRef - COVID-19 testing and infection surveillance: Is a combined digital contact-tracing and mass-testing solution feasible in the United States?
Devin Skoll, Jennifer C. Miller, Leslie A. Saxon
Cardiovascular Digital Health Journal.2020; 1(3): 149. CrossRef - Delay-adjusted age- and sex-specific case fatality rates for COVID-19 in South Korea: Evolution in the estimated risk of mortality throughout the epidemic
A.T. Newall, R.N.F. Leong, A. Nazareno, D.J. Muscatello, J.G. Wood, W.J. Kim
International Journal of Infectious Diseases.2020; 101: 306. CrossRef - Heralding the Digitalization of Life in Post-Pandemic East Asian Societies
Calvin Wai-Loon Ho, Karel Caals, Haihong Zhang
Journal of Bioethical Inquiry.2020; 17(4): 657. CrossRef Intensive Care Unit Capacity and Its Associated Risk Factors During the COVID-19 Surge in the Republic of Korea: Analysis Using Nationwide Health Claims Data
Seung Heon Lee, So-Youn Park, Jeong-Yeon Seon, Woo-Hwi Jeon, Sung Il Nam, Jong-Hak Park, Jae Seok Park, Hae-Young Kim, Niket Thakkar, Prashanth Selvaraj, Anna Bershteyn, In-Hwan Oh
Risk Management and Healthcare Policy.2020; Volume 13: 2571. CrossRef- The Facts, Fallacies and Uncertainties about Coronavirus Disease 2019 (COVID-19)
Tow Keang Lim
Annals of the Academy of Medicine, Singapore.2020; 49(6): 343. CrossRef - Digital contact tracing technologies in epidemics: a rapid review
Andrew Anglemyer, Theresa HM Moore, Lisa Parker, Timothy Chambers, Alice Grady, Kellia Chiu, Matthew Parry, Magdalena Wilczynska, Ella Flemyng, Lisa Bero
Cochrane Database of Systematic Reviews.2020;[Epub] CrossRef - Initial estimates of COVID-19 infections in hospital workers in the United States during the first wave of pandemic
Junaid A. Razzak, Junaid A. Bhatti, Muhammad Ramzan Tahir, Omrana Pasha-Razzak, Oathokwa Nkomazana
PLOS ONE.2020; 15(12): e0242589. CrossRef - Effective Control of COVID-19 in South Korea: Cross-Sectional Study of Epidemiological Data
Gwang Hun Jeong, Hyo Jeong Lee, Jinhee Lee, Jun Young Lee, Keum Hwa Lee, Young Joo Han, Sojung Yoon, Seohyun Ryu, Da Kyung Kim, Myung Bae Park, Jae Won Yang, Maria Effenberger, Michael Eisenhut, Sung Hwi Hong, Andreas Kronbichler, Ramy Abou Ghayda, Jae Il
Journal of Medical Internet Research.2020; 22(12): e22103. CrossRef - Evidence of Long-Distance Droplet Transmission of SARS-CoV-2 by Direct Air Flow in a Restaurant in Korea
Keun-Sang Kwon, Jung-Im Park, Young Joon Park, Don-Myung Jung, Ki-Wahn Ryu, Ju-Hyung Lee
Journal of Korean Medical Science.2020;[Epub] CrossRef - Why many countries failed at COVID contact-tracing — but some got it right
Dyani Lewis
Nature.2020; 588(7838): 384. CrossRef - The Serial Interval of COVID-19 in Korea: 1,567 Pairs of Symptomatic Cases from Contact Tracing
Kwan Hong, Sujin Yum, Jeehyun Kim, Byung Chul Chun
Journal of Korean Medical Science.2020;[Epub] CrossRef - A Public Platform for Virtual IoT-Based Monitoring and Tracking of COVID-19
Younchan Jung, Ronnel Agulto
Electronics.2020; 10(1): 12. CrossRef - The feasibility of organ transplantation during the COVID-19 outbreak: experiences from South Korea
Juhan Lee, Eun Jin Kim, Kyong Ihn, Jae Geun Lee, Dong Jin Joo, Myoung Soo Kim, Soon Il Kim, Yu Seun Kim, Kyu Ha Huh
Korean Journal of Transplantation.2020; 34(4): 257. CrossRef
- Privacy risk in contact tracing systems
- Estimation of the Size of Dengue and Zika Infection Among Korean Travelers to Southeast Asia and Latin America, 2016–2017
- Chaeshin Chu, Een Suk Shin
- Osong Public Health Res Perspect. 2019;10(6):394-398. Published online December 31, 2019
- DOI: https://doi.org/10.24171/j.phrp.2019.10.6.10
- 4,183 View
- 61 Download
-
 Abstract
Abstract
 PDF
PDF Objectives To estimate the number and risk of imported infections resulting from people visiting Asian and Latin American countries.
Methods The dataset of visitors to 5 Asian countries with dengue were analyzed for 2016 and 2017, and in the Philippines, Thailand and Vietnam, imported cases of zika virus infection were also reported. For zika virus, a single imported case was reported from Brazil in 2016, and 2 imported cases reported from the Maldives in 2017. To understand the transmissibility in 5 Southeast Asian countries, the estimate of the force of infection, i.e., the hazard of infection per year and the average duration of travel has been extracted. Outbound travel numbers were retrieved from the World Tourism Organization, including business travelers.
Results The incidence of imported dengue in 2016 was estimated at 7.46, 15.00, 2.14, 4.73 and 2.40 per 100,000 travelers visiting Philippines, Indonesia, Thailand, Malaysia and Vietnam, respectively. Similarly, 2.55, 1.65, 1.53, 1.86 and 1.70 per 100,000 travelers in 2017, respectively. It was estimated that there were 60.1 infections (range: from 16.8 to 150.7 infections) with zika virus in Brazil, 2016, and 345.6 infections (range: from 85.4 to 425.5 infections) with zika virus in the Maldives, 2017.
Conclusion This study emphasizes that dengue and zika virus infections are mild in their nature, and a substantial number of infections may go undetected. An appropriate risk assessment of zika virus infection must use the estimated total size of infections.
- Relationships between Virulence Factors and Antimicrobial Resistance among
Escherichia coli Isolated from Urinary Tract Infections and Commensal Isolates in Tehran, Iran - Mohammad Reza Asadi Karam, Mehri Habibi, Saeid Bouzari
- Osong Public Health Res Perspect. 2018;9(5):217-224. Published online October 31, 2018
- DOI: https://doi.org/10.24171/j.phrp.2018.9.5.02
- 6,705 View
- 130 Download
- 30 Crossref
-
 Abstract
Abstract
 PDF
PDF Objectives Uropathogenic
Escherichia coli (UPEC) are the major cause of urinary tract infections (UTIs). Here, we determined whether sensitivity to antibiotics was related to the prevalence of iron scavenging genes, or to biofilm and hemolysis formation.Methods A total of 110 UPEC and 30
E coli isolates were collected from the urine of UTI patients and feces of healthy individuals without UTI, respectively. The presence of iron receptor genes and phenotypic properties were evaluated by polymerase chain reaction and phenotypic methods, respectively. Susceptibility to routine antibiotics was evaluated using the disc diffusion method.Results The prevalence of iron scavenging genes ranged from 21.8% (
ireA ) to 84.5% (chuA ) in the UPEC. Resistance to ceftazidime and cefotaxime was significantly correlated with the presence offyuA andiutA iron genes. Biofilm production was significantly associated with the prevalence offyuA andhma iron genes. A higher degree of antibiotic resistance was exhibited by isolates that produced biofilms than by their non-biofilm producing counterparts.Conclusion Our study clearly indicates that biofilm production is associated with antibiotic resistance, and that iron receptors and hemolysin production also contribute to reduced antibiotic sensitivity. These results further our understanding of the role that these virulence factors play during UPEC pathogenesis, which in turn may be valuable for the development of novel treatment strategies against UTIs.
-
Citations
Citations to this article as recorded by- Correlation between antimicrobial resistance, biofilm formation, and virulence determinants in uropathogenic Escherichia coli from Egyptian hospital
Sara A. Alshaikh, Tarek El-banna, Fatma Sonbol, Mahmoud H. Farghali
Annals of Clinical Microbiology and Antimicrobials.2024;[Epub] CrossRef - Multidrug resistance in pathogenic Escherichia coli isolates from urinary tract infections in dogs, Spain
Ana Abad-Fau, Eloisa Sevilla, Ainara Oro, Inmaculada Martín-Burriel, Bernardino Moreno, Mariano Morales, Rosa Bolea
Frontiers in Veterinary Science.2024;[Epub] CrossRef - Resistant Escherichia coli isolated from wild mammals from two rescue and rehabilitation centers in Costa Rica: characterization and public health relevance
Rita Fernandes, Raquel Abreu, Isa Serrano, Roger Such, Encarnación Garcia-Vila, Sandy Quirós, Eva Cunha, Luís Tavares, Manuela Oliveira
Scientific Reports.2024;[Epub] CrossRef -
Progress toward a vaccine for extraintestinal pathogenic
E. coli
(ExPEC) II: efficacy of a toxin-autotransporter dual antigen approach
Yikun Xing, Justin R. Clark, James D. Chang, Jacob J. Zulk, Dylan M. Chirman, Felipe-Andres Piedra, Ellen E. Vaughan, Haroldo J. Hernandez Santos, Kathryn A. Patras, Anthony W. Maresso, Kimberly A. Kline
Infection and Immunity.2024;[Epub] CrossRef - Uropathogenic Escherichia coli (UPEC)-Associated Urinary Tract Infections: The Molecular Basis for Challenges to Effective Treatment
Shane Whelan, Brigid Lucey, Karen Finn
Microorganisms.2023; 11(9): 2169. CrossRef - Susceptibility and Virulence of Enterobacteriaceae Isolated from Urinary Tract Infections in Benin
Funkè F. Assouma, Haziz Sina, Tomabu Adjobimey, Agossou Damien Pacôme Noumavo, Akim Socohou, Bawa Boya, Ange D. Dossou, Lauriane Akpovo, Basile Boni Saka Konmy, Jacques F. Mavoungou, Adolphe Adjanohoun, Lamine Baba-Moussa
Microorganisms.2023; 11(1): 213. CrossRef - Association Between Uropathogenic Escherichia coli Virulence Genes and Severity of Infection and Resistance to Antibiotics
Sofía Alejandra Fonseca-Martínez, Ruth Aralí Martínez-Vega, Ana Elvira Farfán-García, Clara Isabel González Rugeles, Libeth Yajaira Criado-Guerrero
Infection and Drug Resistance.2023; Volume 16: 3707. CrossRef - Incidence of biofilms among the multidrug resistant E. coli, isolated from urinary tract infections in the Nilgiris district, South India
A. P. Cardiliya, M. J. N. Chandrasekar, M. J. Nanjan
Brazilian Journal of Microbiology.2023; 54(3): 1809. CrossRef - Correlation of biofilm formation, virulence factors, and phylogenetic groups among Escherichia coli strains causing urinary tract infection: A global systematic review and meta-analysis
HosseinKarballaei Mirzahosseini, Farhad Najmeddin, Atabak Najafi, Arezoo Ahmadi, Hamidreza Sharifnia, Azad Khaledi, Mojtaba Mojtahedzadeh
Journal of Research in Medical Sciences.2023; 28(1): 66. CrossRef - Diabetic Foot Osteomyelitis Caused by Co-Infection with Methicillin-Resistant Staphylococcus aureus and Multidrug-Resistant Extended-Spectrum ß-Lactamase-Producing Escherichia coli: A Case Report
Shiori Kitaya, Chieko Miura, Ayano Suzuki, Yoshimichi Imai, Koichi Tokuda, Hajime Kanamori
Applied Microbiology.2023; 3(3): 1046. CrossRef - Fluoroquinolone resistance determinants in carbapenem-resistant Escherichia coli isolated from urine clinical samples in Thailand
Parichart Boueroy, Peechanika Chopjitt, Rujirat Hatrongjit, Masatomo Morita, Yo Sugawara, Yukihiro Akeda, Tetsuya Iida, Shigeyuki Hamada, Anusak Kerdsin
PeerJ.2023; 11: e16401. CrossRef - Characterization of virulence determinants and phylogenetic background of multiple and extensively drug resistant Escherichia coli isolated from different clinical sources in Egypt
Rana El-baz, Heba Shehta Said, Eman Salama Abdelmegeed, Rasha Barwa
Applied Microbiology and Biotechnology.2022; 106(3): 1279. CrossRef - A global systematic review and meta-analysis on correlation between biofilm producers and non-biofilm producers with antibiotic resistance in Uropathogenic Escherichia coli
Mitra Garousi, Sina Monazami Tabar, Hosein Mirazi, Parnia Asgari, Paniz Sabeghi, Astireh Salehi, Azad Khaledi, Mohammad Ghenaat Pisheh Sanani, Hossein Karballaei Mirzahosseini
Microbial Pathogenesis.2022; 164: 105412. CrossRef - Virulence factors, antimicrobial resistance and the relationship between these characteristics in uropathogenic Escherichia coli
Farzaneh Firoozeh, Mohammad Zibaei, Farzad Badmasti, Azad Khaledi
Gene Reports.2022; 27: 101622. CrossRef - Association between Virulence Factors and Antimicrobial Resistance of Klebsiella pneumoniae Clinical Isolates from North Kerala
Ramya Kumaran, R.V. Geetha, Sabitha Baby
Journal of Pure and Applied Microbiology.2022; 16(2): 867. CrossRef - Characterization of virulence factors and antibiotic resistance pattern of uropathogenic Escherichia coli strains in a tertiary care center
Naveen Kumar M, Sevitha Bhat, Archana Bhat K, Vishwas Saralaya, Shalini Shenoy Mulki
F1000Research.2022; 11: 1163. CrossRef - Antibiotic Resistance, Biofilm Formation and Sub-Inhibitory Hydrogen Peroxide Stimulation in Uropathogenic Escherichia coli
Prabin Dawadi, Santosh Khanal, Tista Prasai Joshi, Sudeep KC, Reshma Tuladhar, Bijaya Laxmi Maharjan, Anjani Darai, Dev Raj Joshi
Microbiology Insights.2022; 15: 117863612211352. CrossRef - Characterization of virulence factors and antibiotic resistance pattern of uropathogenic Escherichia coli strains in a tertiary care center
Naveen Kumar M, Sevitha Bhat, Archana Bhat K, Vishwas Saralaya, Shalini Shenoy Mulki
F1000Research.2022; 11: 1163. CrossRef - Insects, Rodents, and Pets as Reservoirs, Vectors, and Sentinels of Antimicrobial Resistance
Willis Gwenzi, Nhamo Chaukura, Norah Muisa-Zikali, Charles Teta, Tendai Musvuugwa, Piotr Rzymski, Akebe Luther King Abia
Antibiotics.2021; 10(1): 68. CrossRef - Virulence genes and phylogenetic groups of uropathogenic Escherichia coli isolates from patients with urinary tract infection and uninfected control subjects: a case-control study
Seyedeh Elham Rezatofighi, Mahsa Mirzarazi, Mansour Salehi
BMC Infectious Diseases.2021;[Epub] CrossRef - Virulence characterization and clonal analysis of uropathogenic Escherichia coli metallo-beta-lactamase-producing isolates
Fatemeh Zangane Matin, Seyedeh Elham Rezatofighi, Mohammad Roayaei Ardakani, Mohammad Reza Akhoond, Fahimeh Mahmoodi
Annals of Clinical Microbiology and Antimicrobials.2021;[Epub] CrossRef - Antimicrobial Susceptibility and Detection of Virulence-Associated Genes in Escherichia coli Strains Isolated from Commercial Broilers
Tímea Kocúreková, Lívia Karahutová, Dobroslava Bujňáková
Antibiotics.2021; 10(11): 1303. CrossRef - Evaluation of Biofilm Formation and Virulence Genes and Association with Antibiotic Resistance Patterns of Uropathogenic Escherichia coli Strains in Southwestern Iran
Mostafa Boroumand, Asghar Sharifi, Mohammad Amin Ghatei, Mohsen Sadrinasab
Jundishapur Journal of Microbiology.2021;[Epub] CrossRef - Differences of virulence factors, and antimicrobial susceptibility according to phylogenetic group in uropathogenic Escherichia coli strains isolated from Korean patients
Miri Hyun, Ji Yeon Lee, Hyun ah Kim
Annals of Clinical Microbiology and Antimicrobials.2021;[Epub] CrossRef - Changes in Bacterial Spectrum and Resistance Patterns Over Time in the Urine of Patients with Neurogenic Lower Urinary Tract Dysfunction Due to Spinal Cord Injury
Jürgen Pannek, Carmen Kurmann, Jörg Krebs, Valentin Habermacher, Jens Wöllner
Urologia Internationalis.2021; 105(5-6): 483. CrossRef - A systematic review and meta-analysis of antibiotic resistance patterns, and the correlation between biofilm formation with virulence factors in uropathogenic E. coli isolated from urinary tract infections
Fei Zhao, Huanxin Yang, Dezhong Bi, Azad Khaledi, Mingqi Qiao
Microbial Pathogenesis.2020; 144: 104196. CrossRef - A survey for phylogenetic relationship; presence of virulence genes and antibiotic resistance patterns of avian pathogenic and uropathogenic Escherichia coli isolated from poultry and humans in Yazd, Iran
Mansoureh Bakhshi, Hengameh Zandi, Mehdi Fatahi Bafghi, Akram Astani, Vahid Reza Ranjbar, Mahmood Vakili
Gene Reports.2020; 20: 100725. CrossRef - Biofilm formation, antimicrobial susceptibility and virulence genes of Uropathogenic Escherichia coli isolated from clinical isolates in Uganda
Paul Katongole, Fatuma Nalubega, Najjuka Christine Florence, Benon Asiimwe, Irene Andia
BMC Infectious Diseases.2020;[Epub] CrossRef - Relationship between Virulence and Resistance among Gram-Negative Bacteria
Virginio Cepas, Sara M. Soto
Antibiotics.2020; 9(10): 719. CrossRef - Virulence factors of uropathogenic Escherichia coli (UPEC) and correlation with antimicrobial resistance
Chhaya Shah, Ratna Baral, Bijay Bartaula, Lok Bahadur Shrestha
BMC Microbiology.2019;[Epub] CrossRef
- Correlation between antimicrobial resistance, biofilm formation, and virulence determinants in uropathogenic Escherichia coli from Egyptian hospital
- Epidemiological Study on
Candida Species in Patients with Cancer in the Intensive Care Unit - Young-ju Choi, Byeongyeo Lee, Sun-A Park
- Osong Public Health Res Perspect. 2017;8(6):384-388. Published online December 31, 2017
- DOI: https://doi.org/10.24171/j.phrp.2017.8.6.05
- 3,642 View
- 23 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Objectives Although cancer survival rates have increased, serious infection complications can arise in cancer patients.
Candida can occur in various tissues and has significant effects on the prognosis of patients with cancer. Thus, we conducted an epidemiological study onCandida infections in patients with cancer admitted to the intensive care unit.Methods A retrospective study was conducted in adult patients with cancer admitted to the intensive care unit between January 1, 2013, and December 31, 2015.
Candida infection status and predictive factors for mortality were examined in 634 patients.Results The predictive factors for mortality included the use of steroids, use of a central venous catheter or mechanical ventilator, and identification of
Candida in the blood. Patients who stayed in the surgical and intensive care unit for more than 7 days had a lower risk of death than that in those with shorter days.Conclusion The present study shows that invasive procedures, bloodstream infections, and the use of steroids increase the risk of mortality in
Candida -infected patients with cancer. To improve the quality of life and reduce mortality, further studies are needed on the factors affecting the risk of mortality associated withCandida infection.-
Citations
Citations to this article as recorded by- Ionic Liquids with Anti-Candida and Anticancer Dual Activity as Potential N-Myristoyltransferase Inhibitors
Larysa Metelytsia, Maria Trush, Ivan Semenyuta, Sergiy Rogalsky, Oleksandr Kobzar, Larisa Kalashnikova, Volodymyr Blagodatny, Diana Hodyna
Current Bioactive Compounds.2020; 16(7): 1036. CrossRef
- Ionic Liquids with Anti-Candida and Anticancer Dual Activity as Potential N-Myristoyltransferase Inhibitors
- Foodborne Infectious Diseases Mediated by Inappropriate Infection Control in Food Service Businesses and Relevant Countermeasures in Korea
- Jong Myong Park, Young-Hyun You, Hyun-Min Cho, Ji Won Hong, Sa-Youl Ghim
- Osong Public Health Res Perspect. 2017;8(3):159-168. Published online June 30, 2017
- DOI: https://doi.org/10.24171/j.phrp.2017.8.3.02
- 4,963 View
- 37 Download
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF Objectives The objective of this review is to propose an appropriate course of action for improving the guidelines followed by food handlers for control of infection. For this purpose, previous epidemiological reports related to acute gastroenteritis in food service businesses mediated by food handlers were intensively analyzed.
Methods Relevant studies were identified in international databases. We selected eligible papers reporting foodborne infectious disease outbreaks. Among primary literature collection, the abstract of each article was investigated to find cases that absolutely identified a causative factor to be food handlers’ inappropriate infection control and the taxon of causative microbial agents by epidemiological methodologies. Information about the sites (type of food business) where the outbreaks occurred was investigated.
Results A wide variety of causative microbial agents has been investigated, using several epidemiological methods. These agents have shown diverse propagation pathways based on their own molecular pathogenesis, physiology, taxonomy, and etiology.
Conclusion Depending on etiology, transmission, propagation, and microbiological traits, we can predict the transmission characteristics of pathogens in food preparation areas. The infected food workers have a somewhat different ecological place in infection epidemiology as compared to the general population. However, the current Korean Food Safety Act cannot propose detailed guidelines. Therefore, different methodologies have to be made available to prevent further infections.
-
Citations
Citations to this article as recorded by- Pilot study for the development of a screening questionnaire to detect sarcopenic obesity
D. J. Bissonnette, B. N. Burk, M. Hadley, P. Knoblich
International Journal of Obesity.2022; 46(7): 1328. CrossRef - Worker Protection Scenarios for General Analytical Testing Facility under Several Infection Propagation Risks: Scoping Review, Epidemiological Model and ISO 31000
Jong-Myong Park, Joong-Hee Cho, Nam-Soo Jun, Ki-In Bang, Ji-Won Hong
International Journal of Environmental Research an.2022; 19(19): 12001. CrossRef - Assessment of potential factors that support the endemicity of cholera in Nigeria from food handlers, health workers and the environment
Olufemi Samuel Amoo, Oluwatoyin Awoderu, Jacob Yisau, David Oladele, Aghata Nkiru David, Toyosi Raheem, Mabel Uwandu, Moses Bamidele , Toun Wuraola Fesobi, Adeshina AbdusSalam, Samuel Nduaga, Chinedum Taahie Oparaugo, Morakinyo Ajayi, Francisc
Microbiologia Medica.2021;[Epub] CrossRef - The Korean food franchise industry: Diverse development and conceptual definitions of a food safety managing body
Jong Myong Park, Jong Mun Kim, Ah Reum Lee, Hyun Min Cho, Ji Won Hong, Sa‐Youl Ghim
Journal of Food Safety.2019;[Epub] CrossRef - Microbial risks in food franchise: A step forward in establishing ideal cleaning and disinfection practices in SSOPs
Jong Myong Park, Ah Reum Lee, Ji Won Hong, Sa‐Youl Ghim
Journal of Food Safety.2019;[Epub] CrossRef - New procedures for food handlers under infectious gastrointestinal disease: To control emerging microbial problems
Jong Myong Park, Hyun Min Cho, Jong Mun Kim, Sa‐Youl Ghim
Journal of Food Safety.2018;[Epub] CrossRef
- Pilot study for the development of a screening questionnaire to detect sarcopenic obesity



 First
First Prev
Prev


