Search
- Page Path
- HOME > Search
- Time-series comparison of COVID-19 case fatality rates across 21 countries with adjustment for multiple covariates
- Yongmoon Kim, Bryan Inho Kim, Sangwoo Tak
- Osong Public Health Res Perspect. 2022;13(6):424-434. Published online November 28, 2022
- DOI: https://doi.org/10.24171/j.phrp.2022.0212
- 2,681 View
- 110 Download
- 1 Web of Science
- 1 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 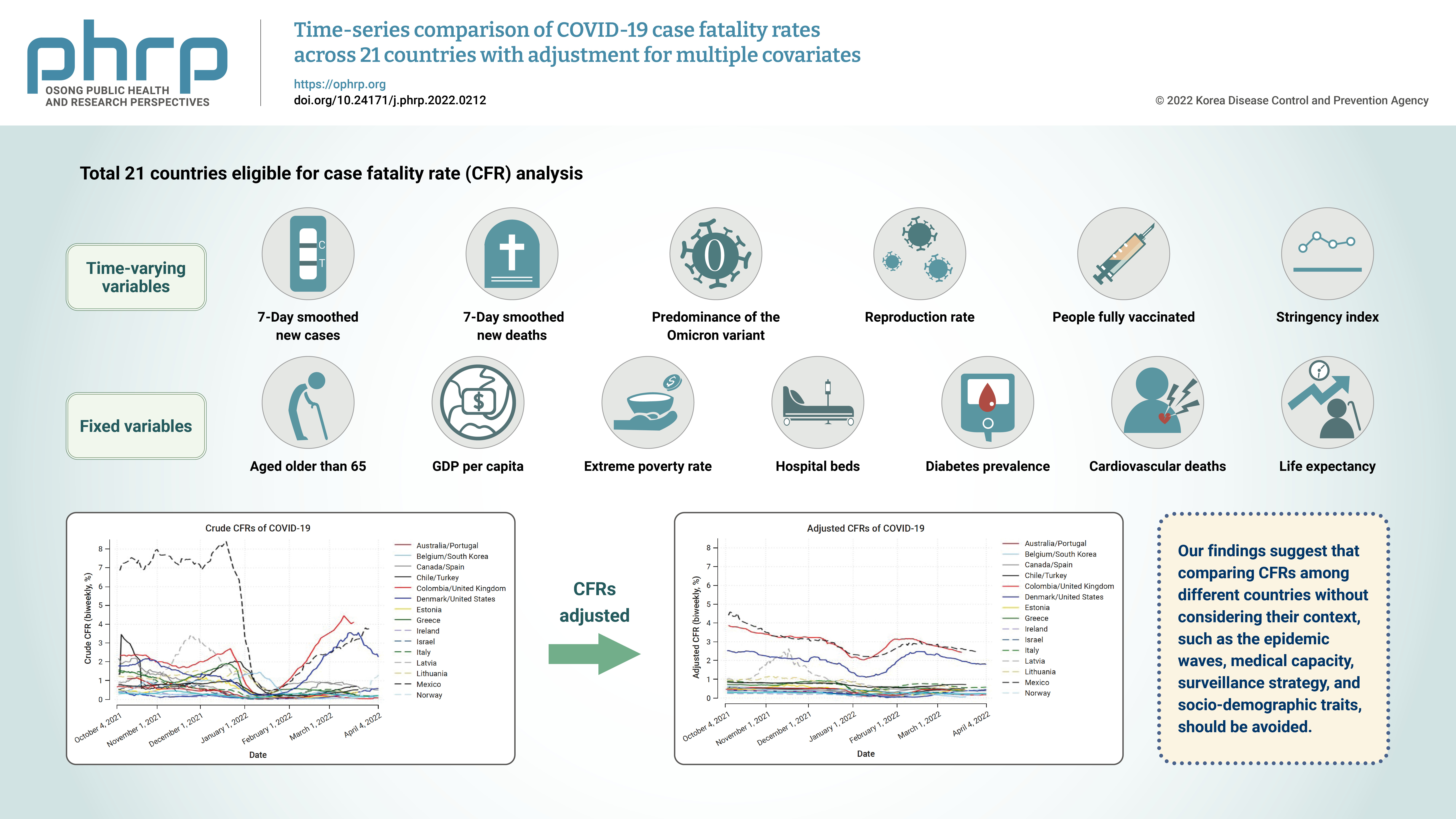
- Objectives
Although it is widely used as a measure for mortality, the case fatality rate (CFR) ofcoronavirus disease 2019 (COVID-19) can vary over time and fluctuate for many reasons otherthan viral characteristics. To compare the CFRs of different countries in equal measure, weestimated comparable CFRs after adjusting for multiple covariates and examined the mainfactors that contributed to variability in the CFRs among 21 countries.Methods: For statistical analysis, time-series cross-sectional data were collected from OurWorld in Data, CoVariants.org, and GISAID. Biweekly CFRs of COVID-19 were estimated bypooled generalized linear squares regression models for the panel data. Covariates includedthe predominant virus variant, reproduction rate, vaccination, national economic status,hospital beds, diabetes prevalence, and population share of individuals older than age 65. Intotal, 21 countries were eligible for analysis.Results: Adjustment for covariates reduced variation in the CFRs of COVID-19 across countriesand over time. Regression results showed that the dominant spread of the Omicron variant,reproduction rate, and vaccination were associated with lower country-level CFRs, whereasage, the extreme poverty rate, and diabetes prevalence were associated with higher countrylevel CFRs.Conclusion: A direct comparison of crude CFRs among countries may be fallacious, especiallyin a cross-sectional analysis. Our study presents an adjusted comparison of CFRs over timefor a more proper comparison. In addition, our findings suggest that comparing CFRs amongdifferent countries without considering their context, such as the epidemic phase, medicalcapacity, surveillance strategy, and socio-demographic traits, should be avoided. -
Citations
Citations to this article as recorded by- Comments on the article "Time-series comparison of COVID-19 case fatality rates across 21 countries with adjustment for multiple covariates"
Gaetano Perone
Osong Public Health and Research Perspectives.2023; 14(2): 146. CrossRef
- Comments on the article "Time-series comparison of COVID-19 case fatality rates across 21 countries with adjustment for multiple covariates"
- COVID-19 prediction models: a systematic literature review
- Sheikh Muzaffar Shakeel, Nithya Sathya Kumar, Pranita Pandurang Madalli, Rashmi Srinivasaiah, Devappa Renuka Swamy
- Osong Public Health Res Perspect. 2021;12(4):215-229. Published online August 13, 2021
- DOI: https://doi.org/10.24171/j.phrp.2021.0100
- 8,190 View
- 180 Download
- 15 Web of Science
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF - As the world grapples with the problem of the coronavirus disease 2019 (COVID-19) pandemic and its devastating effects, scientific groups are working towards solutions to mitigate the effects of the virus. This paper aimed to collate information on COVID-19 prediction models. A systematic literature review is reported, based on a manual search of 1,196 papers published from January to December 2020. Various databases such as Google Scholar, Web of Science, and Scopus were searched. The search strategy was formulated and refined in terms of subject keywords, geographical purview, and time period according to a predefined protocol. Visualizations were created to present the data trends according to different parameters. The results of this systematic literature review show that the study findings are critically relevant for both healthcare managers and prediction model developers. Healthcare managers can choose the best prediction model output for their organization or process management. Meanwhile, prediction model developers and managers can identify the lacunae in their models and improve their data-driven approaches.
-
Citations
Citations to this article as recorded by- The Telemedicine Demand Index and its Utility in Managing COVID-19 Case Surges
Martin Yong Kwong Lee, Kie Beng Goh, Deanna Xiuting Koh, Si Jack Chong, Raymond Swee Boon Chua
Telemedicine and e-Health.2024; 30(2): 545. CrossRef - Vaccination compartmental epidemiological models for the delta and omicron SARS-CoV-2 variants
J. Cuevas-Maraver, P.G. Kevrekidis, Q.Y. Chen, G.A. Kevrekidis, Y. Drossinos
Mathematical Biosciences.2024; 367: 109109. CrossRef - The reporting completeness and transparency of systematic reviews of prognostic prediction models for COVID-19 was poor: a methodological overview of systematic reviews
Persefoni Talimtzi, Antonios Ntolkeras, Georgios Kostopoulos, Konstantinos I. Bougioukas, Eirini Pagkalidou, Andreas Ouranidis, Athanasia Pataka, Anna-Bettina Haidich
Journal of Clinical Epidemiology.2024; 167: 111264. CrossRef - A comprehensive benchmark for COVID-19 predictive modeling using electronic health records in intensive care
Junyi Gao, Yinghao Zhu, Wenqing Wang, Zixiang Wang, Guiying Dong, Wen Tang, Hao Wang, Yasha Wang, Ewen M. Harrison, Liantao Ma
Patterns.2024; 5(4): 100951. CrossRef - A study of learning models for COVID-19 disease prediction
Sakshi Jain, Pradeep Kumar Roy
Journal of Ambient Intelligence and Humanized Comp.2024; 15(4): 2581. CrossRef - Is It Possible to Predict COVID-19? Stochastic System Dynamic Model of Infection Spread in Kazakhstan
Berik Koichubekov, Aliya Takuadina, Ilya Korshukov, Anar Turmukhambetova, Marina Sorokina
Healthcare.2023; 11(5): 752. CrossRef - Early triage echocardiography to predict outcomes in patients admitted with COVID‐19: a multicenter study
Daniel Peck, Andrea Beaton, Maria Carmo Nunes, Nicholas Ollberding, Allison Hays, Pranoti Hiremath, Federico Asch, Nitin Malik, Christopher Fung, Craig Sable, Bruno Nascimento
Echocardiography.2023; 40(5): 388. CrossRef - Static Seeding and Clustering of LSTM Embeddings to Learn From Loosely Time-Decoupled Events
Christian G. Manasseh, Razvan Veliche, Jared Bennett, Hamilton Scott Clouse
IEEE Access.2023; 11: 64219. CrossRef - Harnessing the power of AI: Advanced deep learning models optimization for accurate SARS-CoV-2 forecasting
Muhammad Usman Tariq, Shuhaida Binti Ismail, Muhammad Babar, Ashir Ahmad, Lin Wang
PLOS ONE.2023; 18(7): e0287755. CrossRef - Development and validation of COEWS (COVID-19 Early Warning Score) for hospitalized COVID-19 with laboratory features: A multicontinental retrospective study
Riku Klén, Ivan A Huespe, Felipe Aníbal Gregalio, Antonio Lalueza Lalueza Blanco, Miguel Pedrera Jimenez, Noelia Garcia Barrio, Pascual Ruben Valdez, Matias A Mirofsky, Bruno Boietti, Ricardo Gómez-Huelgas, José Manuel Casas-Rojo, Juan Miguel Antón-Santos
eLife.2023;[Epub] CrossRef - Dynamic transmission modeling of COVID-19 to support decision-making in Brazil: A scoping review in the pre-vaccine era
Gabriel Berg de Almeida, Lorena Mendes Simon, Ângela Maria Bagattini, Michelle Quarti Machado da Rosa, Marcelo Eduardo Borges, José Alexandre Felizola Diniz Filho, Ricardo de Souza Kuchenbecker, Roberto André Kraenkel, Cláudia Pio Ferreira, Suzi Alves Cam
PLOS Global Public Health.2023; 3(12): e0002679. CrossRef - Predictive Models for Forecasting Public Health Scenarios: Practical Experiences Applied during the First Wave of the COVID-19 Pandemic
Jose M. Martin-Moreno, Antoni Alegre-Martinez, Victor Martin-Gorgojo, Jose Luis Alfonso-Sanchez, Ferran Torres, Vicente Pallares-Carratala
International Journal of Environmental Research an.2022; 19(9): 5546. CrossRef - Artificial intelligence and clinical deterioration
James Malycha, Stephen Bacchi, Oliver Redfern
Current Opinion in Critical Care.2022; 28(3): 315. CrossRef
- The Telemedicine Demand Index and its Utility in Managing COVID-19 Case Surges
- Factors Associated with Cesarean Section in Tehran, Iran using Multilevel Logistic Regression Model
- Payam Amini, Maryam Mohammadi, Reza Omani-Samani, Amir Almasi-Hashiani, Saman Maroufizadeh
- Osong Public Health Res Perspect. 2018;9(2):86-92. Published online April 30, 2018
- DOI: https://doi.org/10.24171/j.phrp.2018.9.2.08
- 5,514 View
- 61 Download
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF Objectives Over the past few decades, the prevalence of cesarean sections (CS) have risen dramatically worldwide, particularly in Iran. The aim of this study was to determine the prevalence of CS in Tehran, and to examine the associated risk factors.
Methods A cross-sectional study of 4,308 pregnant women with singleton live-births in Tehran, Iran, between July 6–21, 2015 was performed. Multilevel logistic regression analysis was performed using demographic and obstetrical variables at the first level, and hospitals as a variable at the second level.
Results The incidence of CS was 72.0%. Multivariate analysis showed a significant relationship between CS and the mother’s age, socioeconomic status, body mass index, parity, type of pregnancy, preeclampsia, infant height, and baby’s head circumference. The intra-class correlation using the second level variable, the hospital was 0.292, indicating approximately 29.2% of the total variation in the response variable accounted for by the hospital.
Conclusion The incidence of CS was substantially higher than other countries. Therefore, educational and psychological interventions are necessary to reduce CS rates amongst pregnant Iranian women.
-
Citations
Citations to this article as recorded by- Determinants of cesarean mode of childbirth among Rwandan women of childbearing age: Evidence from the 2019–2020 Rwanda Demographic and Health Survey (RDHS)
Nsereko Etienne, Uwase Aline, Mpinganzima Ornella, Usanzineza Henriette, Niyitegeka Jean Pierre, Turabayo Jean Léonard, Mwiseneza Marie Josee, Mugeni Girimpundu Candide, Moreland Patricia
Public Health Challenges.2024;[Epub] CrossRef - Virtual Reality, Fear of Pain and Labor Pain Intensity: A Randomized Controlled Trial
Halimeh Mohammadi, Javad Rasti, Elham Ebrahimi
Anesthesiology and Pain Medicine.2023;[Epub] CrossRef - The double burden of maternal overweight and short stature and the likelihood of cesarean deliveries in South Asia: An analysis of national datasets from Bangladesh, India, Maldives, Nepal, and Pakistan
Mosiur Rahman, Syed Emdadul Haque, Md. Jahirul Islam, Nguyen Huu Chau, Izzeldin Fadl Adam, Md. Nuruzzaman Haque
Birth.2022; 49(4): 661. CrossRef - Geospatial analysis of cesarean section in Iran (2016–2020): exploring clustered patterns and measuring spatial interactions of available health services
Alireza Mohammadi, Elahe Pishgar, Zahra Salari, Behzad Kiani
BMC Pregnancy and Childbirth.2022;[Epub] CrossRef - Factors associated with cesarean delivery in Bangladesh: A multilevel modeling
Md. Akhtarul Islam, Mst. Tanmin Nahar, Md. Ashfikur Rahman, Sutapa Dey Barna, S.M. Farhad Ibn Anik
Sexual & Reproductive Healthcare.2022; 34: 100792. CrossRef - The Birth Satisfaction Scale-Revised Indicator (BSS-RI): a validation study in Iranian mothers
Reza Omani-Samani, Caroline J. Hollins Martin, Colin R. Martin, Saman Maroufizadeh, Azadeh Ghaheri, Behnaz Navid
The Journal of Maternal-Fetal & Neonatal Medicine.2021; 34(11): 1827. CrossRef - The effect of familiarization with preoperative care on anxiety and vital signs in the patient’s cesarean section: A randomized controlled trial
Mehrnush Mostafayi, Behzad Imani, Shirdel Zandi, Faeze Jongi
European Journal of Midwifery.2021; 5(June): 1. CrossRef - Dynamic prediction of liver cirrhosis risk in chronic hepatitis B patients using longitudinal clinical data
Ying Wang, Xiang-Yong Li, Li-Li Wu, Xiao-Yan Zheng, Yu Deng, Meng-Jie Li, Xu You, Yu-Tian Chong, Yuan-Tao Hao
European Journal of Gastroenterology & Hepatology.2020; 32(1): 120. CrossRef - Factors Contributing to Iranian Pregnant Women’s Tendency to Choice Cesarean Section
Soraya Nouraei Motlagh, Zahra Asadi-piri, Razyeh Bajoulvand, Fatemeh Seyed Mohseni, Katayoun Bakhtiar, Mehdi Birjandi, Maryam Mansouri
Medical - Surgical Nursing Journal.2020;[Epub] CrossRef - Trends and correlates of cesarean section rates over two decades in Nepal
Aliza K. C. Bhandari, Bibha Dhungel, Mahbubur Rahman
BMC Pregnancy and Childbirth.2020;[Epub] CrossRef - Symptoms of Discomfort and Problems Associated with Mode of Delivery During the Puerperium: An Observational Study
Martínez-Galiano, Delgado-Rodríguez, Rodríguez-Almagro, Hernández-Martínez
International Journal of Environmental Research an.2019; 16(22): 4564. CrossRef
- Determinants of cesarean mode of childbirth among Rwandan women of childbearing age: Evidence from the 2019–2020 Rwanda Demographic and Health Survey (RDHS)
- Are There Spatial and Temporal Correlations in the Incidence Distribution of Scrub Typhus in Korea?
- Maengseok Noh, Youngjo Lee, Chaeshin Chu, Jin Gwack, Seung-Ki Youn, Sun Huh
- Osong Public Health Res Perspect. 2013;4(1):39-44. Published online February 28, 2013
- DOI: https://doi.org/10.1016/j.phrp.2013.01.002
- 3,554 View
- 21 Download
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
A hierarchical generalized linear model (HGLM) was applied to estimate the transmission pattern of scrub typhus from 2001 to 2011 in the Republic of Korea, based on spatial and temporal correlation.
Methods
Based on the descriptive statistics of scrub typhus incidence from 2001 to 2011 reported to the Korean Centers for Disease Control and Prevention, the spatial and temporal correlations were estimated by HGLM. Incidences according to age, sex, and year were also estimated by the best-fit model out of nine HGLMs. A disease map was drawn to view the annual regional spread of the disease.
Results
The total number of scrub typhus cases reported from 2001 to 2011 was 51,136: male, 18,628 (36.4%); female, 32,508 (63.6%). The best-fit model selected was a combination of the spatial model (Markov random-field model) and temporal model (first order autoregressive model) of scrub typhus transmission. The peak incidence was 28.80 per 100,000 persons in early October and the peak incidence was 40.17 per 100,000 persons in those aged 63.3 years old by the best-fit HGLM. The disease map showed the spread of disease from the southern central area to a nationwide area, excepting Gangwon-do (province), Gyeongsangbuk-do (province), and Seoul.
Conclusion
In the transmission of scrub typhus in Korea, there was a correlation to the incidence of adjacent areas, as well as that of the previous year. According to the disease map, we are unlikely to see any decrease in the incidence in the near future, unless ongoing aggressive measures to prevent the exposure to the vector, chigger mites, in rural areas, are put into place. -
Citations
Citations to this article as recorded by- Prevalence of chigger mites and Orientia tsutsugamushi strains in northern regions of Gangwon-do, Korea
Soojin Kim, In Yong Lee, Sezim Monoldorova, Jiro Kim, Jang Hoon Seo, Tai-Soon Yong, Bo Young Jeon
Parasites, Hosts and Diseases.2023; 61(3): 263. CrossRef - Urine Metabolite of Mice with Orientia tsutsugamushi Infection
Sangho Choi, Do-Hwan Ahn, Min-Gyu Yoo, Hye-Ja Lee, Seong Beom Cho, Hee-Bin Park, Sung Soon Kim, Hyuk Chu
The American Journal of Tropical Medicine and Hygi.2023; 108(2): 296. CrossRef - Spatiotemporal dynamics and environmental determinants of scrub typhus in Anhui Province, China, 2010–2020
Xianyu Wei, Junyu He, Wenwu Yin, Ricardo J. Soares Magalhaes, Yanding Wang, Yuanyong Xu, Liang Wen, Yehuan Sun, Wenyi Zhang, Hailong Sun
Scientific Reports.2023;[Epub] CrossRef - Epidemiological characteristics of cases with scrub typhus and their correlation with chigger mite occurrence (2019–2021): A focus on case occupation and activity locations
Se‐Jin Jeong, Jin‐Hwan Jeon, Kyung won Hwang
Entomological Research.2023; 53(7): 247. CrossRef - Epidemiological characteristics and spatiotemporal patterns of scrub typhus in Yunnan Province from 2006 to 2017
Pei-Ying Peng, Lei Xu, Gu-Xian Wang, Wen-Yuan He, Ting-Liang Yan, Xian-Guo Guo
Scientific Reports.2022;[Epub] CrossRef - Clinical and Laboratory Predictors associated with Complicated Scrub Typhus
Mi-Hee Kim, Si-Hyun Kim, Jung-Hyun Choi, Seong-Heon Wie
Infection & Chemotherapy.2019; 51(2): 161. CrossRef - Awareness and Work-Related Factors Associated with Scrub Typhus: A Case-Control Study from South Korea
Dong-Seob Kim, Dilaram Acharya, Kwan Lee, Seok-Ju Yoo, Ji-Hyuk Park, Hyun-Sul Lim
International Journal of Environmental Research an.2018; 15(6): 1143. CrossRef - Estimating the burden of scrub typhus: A systematic review
Ana Bonell, Yoel Lubell, Paul N. Newton, John A. Crump, Daniel H. Paris, Janet Foley
PLOS Neglected Tropical Diseases.2017; 11(9): e0005838. CrossRef - Spatiotemporal Dynamics of Scrub Typhus Transmission in Mainland China, 2006-2014
Yi-Cheng Wu, Quan Qian, Ricardo J. Soares Magalhaes, Zhi-Hai Han, Wen-Biao Hu, Ubydul Haque, Thomas A. Weppelmann, Yong Wang, Yun-Xi Liu, Xin-Lou Li, Hai-Long Sun, Yan-Song Sun, Archie C. A. Clements, Shen-Long Li, Wen-Yi Zhang, Mathieu Picardeau
PLOS Neglected Tropical Diseases.2016; 10(8): e0004875. CrossRef - Larval Chigger Mites Collected from Small Mammals in 3 Provinces, Korea
In-Yong Lee, Hyeon-Je Song, Yeon-Joo Choi, Sun-Hye Shin, Min-Kyung Choi, So-Hyun Kwon, E-Hyun Shin, Chan Park, Heung-Chul Kim, Terry A. Klein, Kyung-Hee Park, Won-Jong Jang
The Korean Journal of Parasitology.2014; 52(2): 225. CrossRef
- Prevalence of chigger mites and Orientia tsutsugamushi strains in northern regions of Gangwon-do, Korea
- Spatial and Temporal Distribution of
Plasmodium vivax Malaria in Korea Estimated with a Hierarchical Generalized Linear Model - Maengseok Noh, Youngjo Lee, Seungyoung Oh, Chaeshin Chu, Jin Gwack, Seung-Ki Youn, Shin Hyeong Cho, Won Ja Lee, Sun Huh
- Osong Public Health Res Perspect. 2012;3(4):192-198. Published online December 31, 2012
- DOI: https://doi.org/10.1016/j.phrp.2012.11.003
- 3,345 View
- 19 Download
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
The spatial and temporal correlations were estimated to determine Plasmodium vivax malarial transmission pattern in Korea from 2001–2011 with the hierarchical generalized linear model.
Methods
Malaria cases reported to the Korea Centers for Disease Control and Prevention from 2001 to 2011 were analyzed with descriptive statistics and the incidence was estimated according to age, sex, and year by the hierarchical generalized linear model. Spatial and temporal correlation was estimated and the best model was selected from nine models. Results were presented as diseases map according to age and sex.
Results
The incidence according to age was highest in the 20–25-year-old group (244.52 infections/100,000). Mean ages of infected males and females were 31.0 years and 45.3 years with incidences 7.8 infections/100,000 and 7.1 infections/100,000 after estimation. The mean month for infection was mid-July with incidence 10.4 infections/100,000. The best-fit model showed that there was a spatial and temporal correlation in the malarial transmission. Incidence was very low or negligible in areas distant from the demilitarized zone between Republic of Korea and Democratic People’s Republic of Korea (North Korea) if the 20–29-year-old male group was omitted in the diseases map.
Conclusion
Malarial transmission in a region in Korea was influenced by the incidence in adjacent regions in recent years. Since malaria in Korea mainly originates from mosquitoes from North Korea, there will be continuous decrease if there is no further outbreak in North Korea. -
Citations
Citations to this article as recorded by- Source separation in municipal solid waste management: Practical means to its success in Asian cities
Premakumara Jagath Dickella Gamaralalage, Sadhan Kumar Ghosh, Kazunobu Onogawa
Waste Management & Research: The Journal for a Sus.2022; 40(3): 360. CrossRef - Spatial connectivity in mosquito-borne disease models: a systematic review of methods and assumptions
Sophie A. Lee, Christopher I. Jarvis, W. John Edmunds, Theodoros Economou, Rachel Lowe
Journal of The Royal Society Interface.2021; 18(178): 20210096. CrossRef - Effects of climate change on Plasmodium vivax malaria transmission dynamics: A mathematical modeling approach
Jung Eun Kim, Yongin Choi, Chang Hyeong Lee
Applied Mathematics and Computation.2019; 347: 616. CrossRef - Spatially Filtered Multilevel Analysis on Spatial Determinants for Malaria Occurrence in Korea
Sehyeong Kim, Youngho Kim
International Journal of Environmental Research an.2019; 16(7): 1250. CrossRef - Is it necessary to take anthelmintics every year in Korea?
Sun Huh
Journal of the Korean Medical Association.2018; 61(3): 198. CrossRef - Research on Factors Influencing Municipal Household Solid Waste Separate Collection: Bayesian Belief Networks
Zhujie Chu, Wenna Wang, Bairong Wang, Jun Zhuang
Sustainability.2016; 8(2): 152. CrossRef - Chemotherapeutic drugs for common parasitic diseases in Korea
Sun Huh
Journal of the Korean Medical Association.2013; 56(6): 513. CrossRef - Are There Spatial and Temporal Correlations in the Incidence Distribution of Scrub Typhus in Korea?
Maengseok Noh, Youngjo Lee, Chaeshin Chu, Jin Gwack, Seung-Ki Youn, Sun Huh
Osong Public Health and Research Perspectives.2013; 4(1): 39. CrossRef - Years of Epidemics (2009–2011): Pandemic Influenza and Foot-and-Mouth Disease Epidemic in Korea
Hae-Wol Cho, Chaeshin Chu
Osong Public Health and Research Perspectives.2013; 4(3): 125. CrossRef - A New Statistical Approach to Analyze Plasmodium vivax Malaria Endemic in Korea
Hae-Wol Cho, Chaeshin Chu
Osong Public Health and Research Perspectives.2012; 3(4): 191. CrossRef
- Source separation in municipal solid waste management: Practical means to its success in Asian cities
- Incubation Period of Ebola Hemorrhagic Virus Subtype Zaire
- Martin Eichner, Scott F. Dowell, Nina Firese
- Osong Public Health Res Perspect. 2011;2(1):3-7. Published online June 30, 2011
- DOI: https://doi.org/10.1016/j.phrp.2011.04.001
- 4,106 View
- 15 Download
- 46 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
Ebola hemorrhagic fever has killed over 1300 people, mostly in equatorial Africa. There is still uncertainty about the natural reservoir of the virus and about some of the factors involved in disease transmission. Until now, a maximum incubation period of 21 days has been assumed.
Methods
We analyzed data collected during the Ebola outbreak (subtype Zaire) in Kikwit, Democratic Republic of the Congo, in 1995 using maximum likelihood inference and assuming a log-normally distributed incubation period.
Results
The mean incubation period was estimated to be 12.7 days (standard deviation 4.31 days), indicating that about 4.1% of patients may have incubation periods longer than 21 days.
Conclusion
If the risk of new cases is to be reduced to 1% then 25 days should be used when investigating the source of an outbreak, when determining the duration of surveillance for contacts, and when declaring the end of an outbreak. -
Citations
Citations to this article as recorded by- Prevention and post-exposure management of occupational exposure to Ebola virus
Michael A Moso, Chuan K Lim, Eloise Williams, Caroline Marshall, James McCarthy, Deborah A Williamson
The Lancet Infectious Diseases.2024; 24(2): e93. CrossRef - Systems immunology of transcriptional responses to viral infection identifies conserved antiviral pathways across macaques and humans
Kalani Ratnasiri, Hong Zheng, Jiaying Toh, Zhiyuan Yao, Veronica Duran, Michele Donato, Mario Roederer, Megha Kamath, John-Paul M. Todd, Matthew Gagne, Kathryn E. Foulds, Joseph R. Francica, Kizzmekia S. Corbett, Daniel C. Douek, Robert A. Seder, Shirit E
Cell Reports.2024; 43(2): 113706. CrossRef - Isothermal nucleic acid amplification technology for rapid detection of virus
Zhenting Wei, Xiaowen Wang, Huhu Feng, Fanpu Ji, Dan Bai, Xiaoping Dong, Wei Huang
Critical Reviews in Biotechnology.2023; 43(3): 415. CrossRef - Predicting the combined effects of case isolation, safe funeral practices, and contact tracing during Ebola virus disease outbreaks
Aliou Bouba, Kristina Barbara Helle, Kristan Alexander Schneider, Jan Rychtář
PLOS ONE.2023; 18(1): e0276351. CrossRef - Stability analysis of an SIR epidemic model with homestead-isolation on the susceptible and infectious, immunity, relapse and general incidence rate
Amine Bernoussi
International Journal of Biomathematics.2023;[Epub] CrossRef - Path analysis method in an epidemic model and stability analysis
Yong Zhou, Yiming Ding, Minrui Guo
Frontiers in Physics.2023;[Epub] CrossRef - Tradeoff between speed and reproductive number in pathogen evolution
Andreas Eilersen, Bjarke Frost Nielsen, Kim Sneppen
Physical Review Research.2023;[Epub] CrossRef - A Reinforcement Learning Based Decision Support Tool for Epidemic Control: Validation Study for COVID-19
Mohamed-Amine Chadi, Hajar Mousannif
Applied Artificial Intelligence.2022;[Epub] CrossRef - Spatially-heterogeneous embedded stochastic SEIR models for the 2014–2016 Ebola outbreak in West Africa
Kaitlyn Martinez, Grant Brown, Stephen Pankavich
Spatial and Spatio-temporal Epidemiology.2022; 41: 100505. CrossRef - Staff Scheduling During a Pandemic: The Case of Radiation Therapy Department
Hossein Abouee Mehrizi, Arian Aminoleslami, Johnson Darko, Ernest Osei, Houra Mahmoudzadeh
SSRN Electronic Journal .2022;[Epub] CrossRef - Review of Ebola virus disease in children – how far have we come?
Devika Dixit, Kasereka Masumbuko Claude, Lindsey Kjaldgaard, Michael T. Hawkes
Paediatrics and International Child Health.2021; 41(1): 12. CrossRef - Multi-population stochastic modeling of Ebola in Sierra Leone: Investigation of spatial heterogeneity
Rachid Muleia, Marc Aerts, Christel Faes, Maria Vittoria Barbarossa
PLOS ONE.2021; 16(5): e0250765. CrossRef - Detecting Pathogen Exposure During the Non-symptomatic Incubation Period Using Physiological Data: Proof of Concept in Non-human Primates
Shakti Davis, Lauren Milechin, Tejash Patel, Mark Hernandez, Greg Ciccarelli, Siddharth Samsi, Lisa Hensley, Arthur Goff, John Trefry, Sara Johnston, Bret Purcell, Catherine Cabrera, Jack Fleischman, Albert Reuther, Kajal Claypool, Franco Rossi, Anna Honk
Frontiers in Physiology.2021;[Epub] CrossRef - Advances and insights in the diagnosis of viral infections
Julija Dronina, Urte Samukaite-Bubniene, Arunas Ramanavicius
Journal of Nanobiotechnology.2021;[Epub] CrossRef - Treatment of Ebola-related critical illness
Peter Kiiza, S. Mullin, K. Teo, N. K. J. Adhikari, R. A. Fowler
Intensive Care Medicine.2020; 46(2): 285. CrossRef - AAV Vectored Immunoprophylaxis for Filovirus Infections
Amira D. Rghei, Laura P. van Lieshout, Lisa A. Santry, Matthew M. Guilleman, Sylvia P. Thomas, Leonardo Susta, Khalil Karimi, Byram W. Bridle, Sarah K. Wootton
Tropical Medicine and Infectious Disease.2020; 5(4): 169. CrossRef - Vaccination strategies to control Ebola epidemics in the context of variable household inaccessibility levels
Gerardo Chowell, Amna Tariq, Maria Kiskowski, Benjamin Althouse
PLOS Neglected Tropical Diseases.2019; 13(11): e0007814. CrossRef - Application of the CDC EbolaResponse Modeling tool to disease predictions
Robert H. Gaffey, Cécile Viboud
Epidemics.2018; 22: 22. CrossRef - A mathematical model with isolation for the dynamics of Ebola virus
Amira Rachah
Journal of Physics: Conference Series.2018; 1132: 012058. CrossRef - Multiscale model for pedestrian and infection dynamics during air travel
Sirish Namilae, Pierrot Derjany, Anuj Mubayi, Mathew Scotch, Ashok Srinivasan
Physical Review E.2017;[Epub] CrossRef - Modeling ebola virus disease transmissions with reservoir in a complex virus life ecology
Tsanou Berge, Samuel Bowong, Jean Lubuma, Martin Luther Mann Manyombe
Mathematical Biosciences and Engineering.2017; 15(1): 21. CrossRef - Application of a quantitative entry assessment model to compare the relative risk of incursion of zoonotic bat-borne viruses into European Union Member States
Verity Horigan, Paul Gale, Rowena D. Kosmider, Christopher Minnis, Emma L. Snary, Andrew C. Breed, Robin R.L. Simons
Microbial Risk Analysis.2017; 7: 8. CrossRef - Multigroup deterministic and stochasticSEIRIepidemic models with nonlinear incidence rates and distributed delays: A stability analysis
Hong Zhang, Juan Xia, Paul Georgescu
Mathematical Methods in the Applied Sciences.2017; 40(18): 6254. CrossRef - Modeling spatial invasion of Ebola in West Africa
Jeremy P. D’Silva, Marisa C. Eisenberg
Journal of Theoretical Biology.2017; 428: 65. CrossRef - The potential impact of a prophylactic vaccine for Ebola in Sierra Leone
Erin N. Bodine, Connor Cook, Mikayla Shorten
Mathematical Biosciences and Engineering.2017; 15(2): 337. CrossRef - Ebola virus – from neglected threat to global emergency state
Daniela Alexandra de Meneses Rocha Aguiar Pacheco, Acácio Agostinho Gonçalves Rodrigues, Carmen Maria Lisboa da Silva
Revista da Associação Médica Brasileira.2016; 62(5): 458. CrossRef - Neglected filoviruses
Robin Burk, Laura Bollinger, Joshua C. Johnson, Jiro Wada, Sheli R. Radoshitzky, Gustavo Palacios, Sina Bavari, Peter B. Jahrling, Jens H. Kuhn, Urs Greber
FEMS Microbiology Reviews.2016; 40(4): 494. CrossRef - Treatment–donation-stockpile dynamics in ebola convalescent blood transfusion therapy
Xi Huo, Xiaodan Sun, Kunquan Lan, Jianhong Wu
Journal of Theoretical Biology.2016; 392: 53. CrossRef - Ebola virus disease in nonendemic countries
Samson Sai-Yin Wong, Sally Cheuk-Ying Wong
Journal of the Formosan Medical Association.2015; 114(5): 384. CrossRef - Ebola Hemorrhagic Fever
Maryam Keshtkar Jahromi, Batool Sharifi Mood
International Journal of Infection.2015;[Epub] CrossRef - Tactics and Strategies for Managing Ebola Outbreaks and the Salience of Immunization
Wayne M. Getz, Jean-Paul Gonzalez, Richard Salter, James Bangura, Colin Carlson, Moinya Coomber, Eric Dougherty, David Kargbo, Nathan D. Wolfe, Nadia Wauquier
Computational and Mathematical Methods in Medicine.2015; 2015: 1. CrossRef - What is Ebola?
R. A. Stein
International Journal of Clinical Practice.2015; 69(1): 49. CrossRef - Ebola virus disease outbreak in Nigeria: Transmission dynamics and rapid control
C.L. Althaus, N. Low, E.O. Musa, F. Shuaib, S. Gsteiger
Epidemics.2015; 11: 80. CrossRef - A review of epidemiological parameters from Ebola outbreaks to inform early public health decision-making
Maria D. Van Kerkhove, Ana I. Bento, Harriet L. Mills, Neil M. Ferguson, Christl A. Donnelly
Scientific Data.2015;[Epub] CrossRef - Modeling Post-death Transmission of Ebola: Challenges for Inference and Opportunities for Control
Joshua S. Weitz, Jonathan Dushoff
Scientific Reports.2015;[Epub] CrossRef - Transmission Models of Historical Ebola Outbreaks
John M. Drake, Iurii Bakach, Matthew R. Just, Suzanne M. O’Regan, Manoj Gambhir, Isaac Chun-Hai Fung
Emerging Infectious Diseases.2015; 21(8): 1447. CrossRef - Theoretical perspectives on the infectiousness of Ebola virus disease
Hiroshi Nishiura, Gerardo Chowell
Theoretical Biology and Medical Modelling.2015;[Epub] CrossRef - Effect of Ebola Progression on Transmission and Control in Liberia
Dan Yamin, Shai Gertler, Martial L. Ndeffo-Mbah, Laura A. Skrip, Mosoka Fallah, Tolbert G. Nyenswah, Frederick L. Altice, Alison P. Galvani
Annals of Internal Medicine.2015; 162(1): 11. CrossRef - Transmission dynamics and control of Ebola virus disease (EVD): a review
Gerardo Chowell, Hiroshi Nishiura
BMC Medicine.2014;[Epub] CrossRef - Analysis of Ebolavirus with Decision Tree and Apriori algorithm
Eunby Go, Seungmin Lee, Taeseon Yoon
International Journal of Machine Learning and Comp.2014; 4(6): 543. CrossRef - Calculation of incubation period and serial interval from multiple outbreaks of Marburg virus disease
Boris I Pavlin
BMC Research Notes.2014; 7(1): 906. CrossRef - Outbreaks of Ebola virus disease in Africa: the beginnings of a tragic saga
Jean-Philippe Chippaux
Journal of Venomous Animals and Toxins including T.2014; 20(1): 44. CrossRef - Association between temperature, humidity and ebolavirus disease outbreaks in Africa, 1976 to 2014
S Ng, B J Cowling
Eurosurveillance.2014;[Epub] CrossRef - Early transmission dynamics of Ebola virus disease (EVD), West Africa, March to August 2014
H Nishiura, G Chowell
Eurosurveillance.2014;[Epub] CrossRef - Transmission dynamics and control of Ebola virus disease outbreak in Nigeria, July to September 2014
F O Fasina, A Shittu, D Lazarus, O Tomori, L Simonsen, C Viboud, G Chowell
Eurosurveillance.2014;[Epub] CrossRef - The Road Less Traveled
Chaeshin Chu
Osong Public Health and Research Perspectives.2011; 2(1): 1. CrossRef
- Prevention and post-exposure management of occupational exposure to Ebola virus



 First
First Prev
Prev


