Search
- Page Path
- HOME > Search
- Developing a national surveillance system for stroke and acute myocardial infarction using claims data in the Republic of Korea: a retrospective study
- Tae Jung Kim, Hak Seung Lee, Seong-Eun Kim, Jinju Park, Jun Yup Kim, Jiyoon Lee, Ji Eun Song, Jin-Hyuk Hong, Joongyub Lee, Joong-Hwa Chung, Hyeon Chang Kim, Dong-Ho Shin, Hae-Young Lee, Bum Joon Kim, Woo-Keun Seo, Jong-Moo Park, Soo Joo Lee, Keun-Hwa Jung, Sun U. Kwon, Yun-Chul Hong, Hyo-Soo Kim, Hyun-Jae Kang, Juneyoung Lee, Hee-Joon Bae
- Osong Public Health Res Perspect. 2024;15(1):18-32. Published online January 31, 2024
- DOI: https://doi.org/10.24171/j.phrp.2023.0248
- 855 View
- 54 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 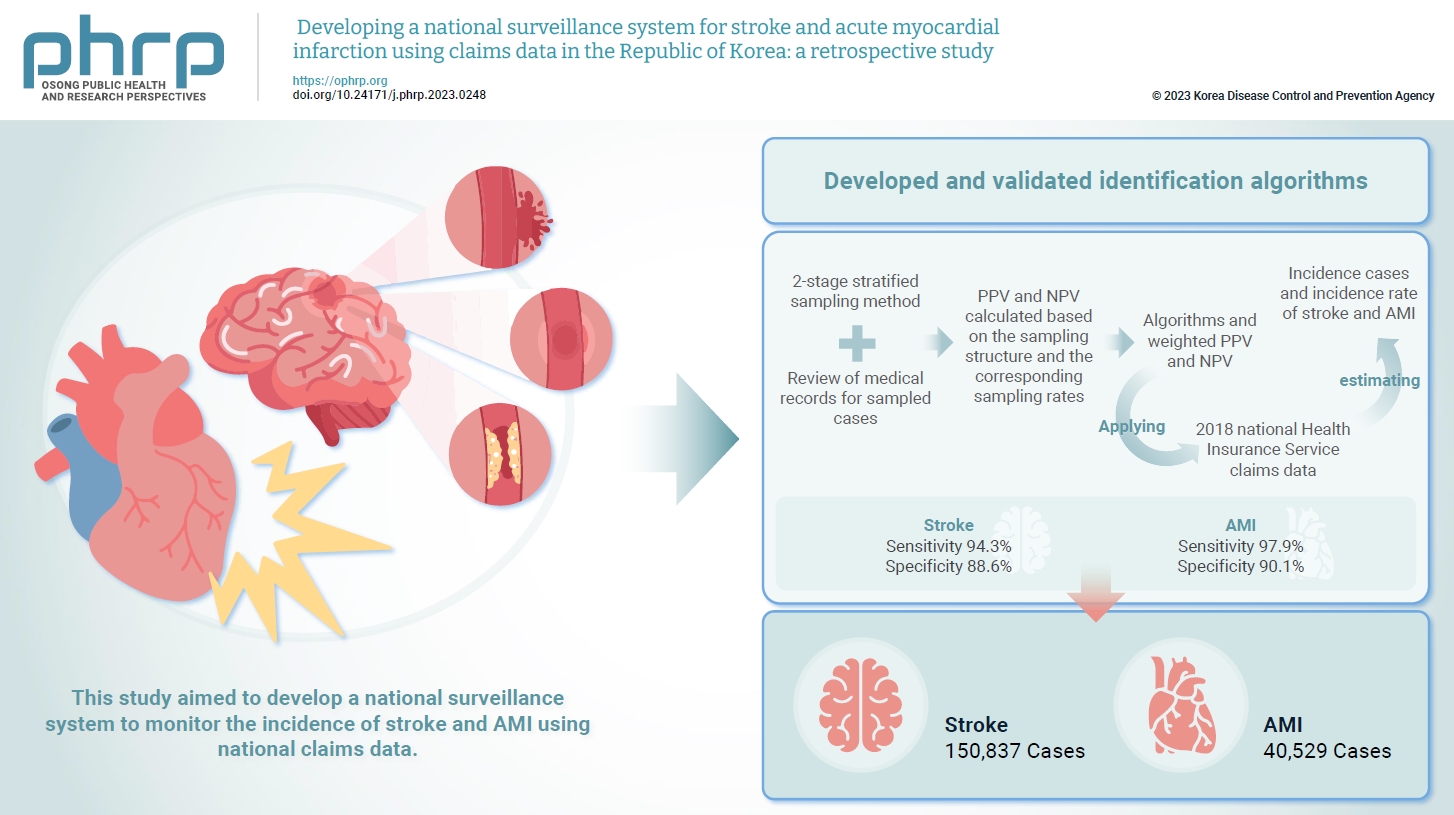
- Objectives
Limited information is available concerning the epidemiology of stroke and acute myocardial infarction (AMI) in the Republic of Korea. This study aimed to develop a national surveillance system to monitor the incidence of stroke and AMI using national claims data. Methods: We developed and validated identification algorithms for stroke and AMI using claims data. This validation involved a 2-stage stratified sampling method with a review of medical records for sampled cases. The weighted positive predictive value (PPV) and negative predictive value (NPV) were calculated based on the sampling structure and the corresponding sampling rates. Incident cases and the incidence rates of stroke and AMI in the Republic of Korea were estimated by applying the algorithms and weighted PPV and NPV to the 2018 National Health Insurance Service claims data. Results: In total, 2,200 cases (1,086 stroke cases and 1,114 AMI cases) were sampled from the 2018 claims database. The sensitivity and specificity of the algorithms were 94.3% and 88.6% for stroke and 97.9% and 90.1% for AMI, respectively. The estimated number of cases, including recurrent events, was 150,837 for stroke and 40,529 for AMI in 2018. The age- and sex-standardized incidence rate for stroke and AMI was 180.2 and 46.1 cases per 100,000 person-years, respectively, in 2018. Conclusion: This study demonstrates the feasibility of developing a national surveillance system based on claims data and identification algorithms for stroke and AMI to monitor their incidence rates.
- Predictors of health-related quality of life in Koreans with cardiovascular disease
- Jung-Hye Lim
- Osong Public Health Res Perspect. 2022;13(1):62-70. Published online February 22, 2022
- DOI: https://doi.org/10.24171/j.phrp.2021.0286
- 3,941 View
- 86 Download
- 1 Web of Science
- 1 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 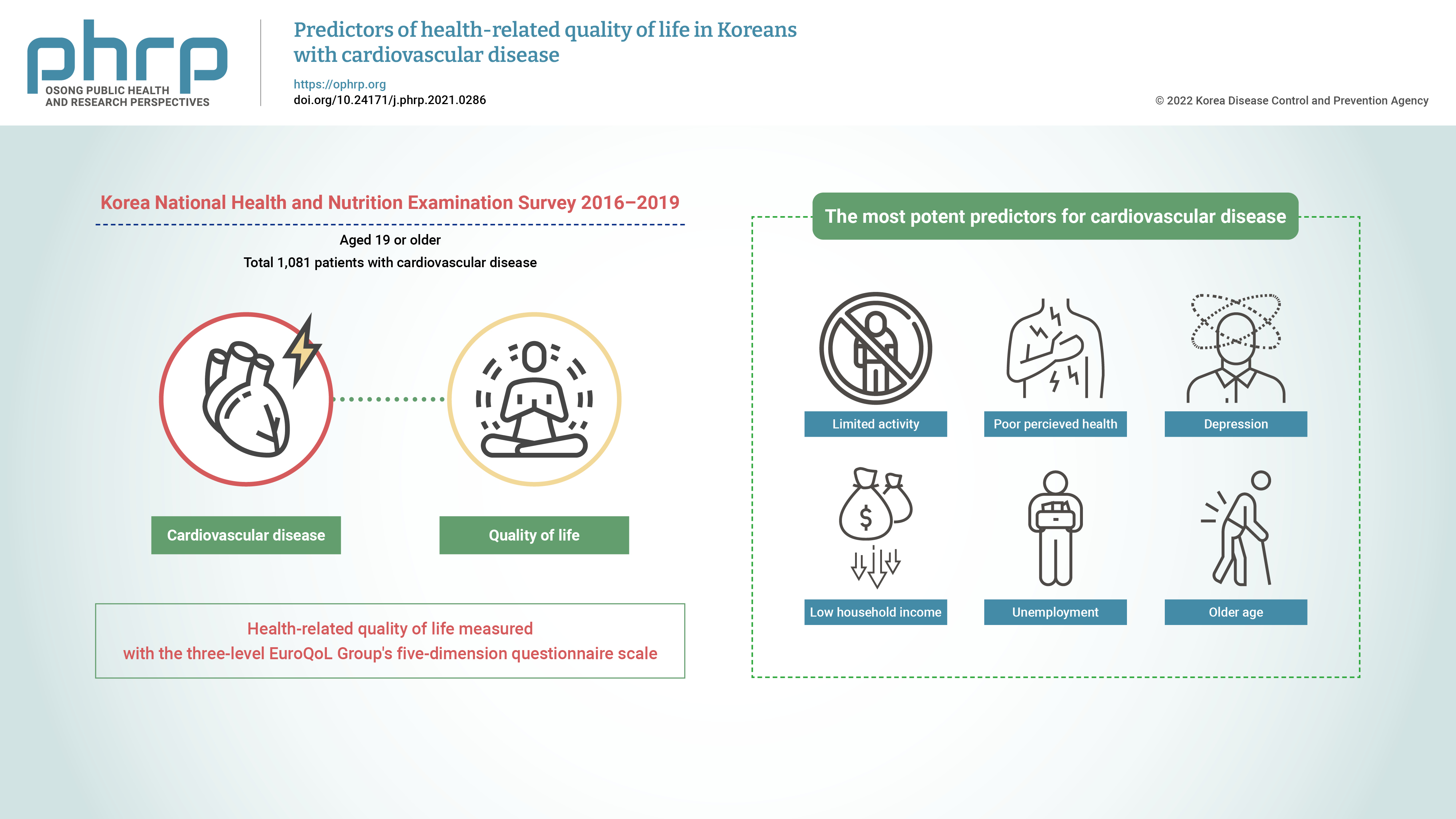
- Objectives
This study aimed to identify the predictors of health-related quality of life (HRQoL) in Korean adults with cardiovascular disease (CVD). Methods: This was a cross-sectional study with a stratified multistage probability sampling design. Data from the 2016 to 2019 Korea National Health and Nutrition Examination Survey (n=32,379) were used. Among the participants aged 19 years or older (n=25,995), 1,081 patients with CVD were extracted after excluding those with missing data and those who had cancer. The participants’ HRQoL was measured using the three-level EuroQoL Group’s five-dimension questionnaire (EQ-5D) scale. Data were analyzed using the t-test, one-way analysis of variance, and general linear regression for complex samples. Results: The most potent predictors of HRQoL in Korean adults with CVD were limited activity (β =−0.103, p <0.001), poor perceived health (β =−0.089, p <0.001), depression (β =−0.065, p<0.01), low household income (β=−0.033, p<0.05), unemployment (β=−0.023, p<0.05), and older age (β=−0.002, p<0.01), which explained 37.2% of the variance. Conclusion: Comprehensive interventions that address both physical and mental factors and social systems that provide financial help need to be implemented to improve the HRQoL of Korean adults with CVD. -
Citations
Citations to this article as recorded by- Factors associated with health-related quality of life in patients with coronary heart disease
Febio Gutama, Melisa Intan Barliana, Irma Melyani Puspitasari
Pharmacia.2022; 69(3): 771. CrossRef
- Factors associated with health-related quality of life in patients with coronary heart disease
- Effects of activities of daily living-based dual-task training on upper extremity function, cognitive function, and quality of life in stroke patients
- Hee-Su An, Deok-Ju Kim
- Osong Public Health Res Perspect. 2021;12(5):304-313. Published online September 13, 2021
- DOI: https://doi.org/10.24171/j.phrp.2021.0177
- 10,776 View
- 306 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Objectives
The aim of this study was to investigate the effect of daily living dual-task training focused on improving attention and executive function of the upper extremities, cognitive function, and quality of life in stroke patients.
Methods
We included 30 stroke patients who were hospitalized between July 2020 and October 2020. They were divided into experimental and control groups through randomization. The experimental group performed 20 minutes of dual-task training and received 10 minutes of conventional occupational therapy, while the control group performed 20 minutes of single-task training and received 10 minutes of conventional occupational therapy. Both groups underwent their respective rehabilitation for 30 minutes per session, 5 times per week for 5 weeks.
Results
Both groups showed significant improvements in upper extremity function, cognitive function, and quality of life; the experimental group showed higher results for all items. A significant between-group difference was observed in the magnitude of the changes.
Conclusion
In stroke patients, dual-task training that combined attention and executive function with daily living activities was found to be meaningful, as it encouraged active participation and motivation. This study is expected to be used as a foundation for future interventions for stroke patients. -
Citations
Citations to this article as recorded by- Intervention and assessment of executive dysfunction in patients with stroke: A scoping review
Katsuya Sakai, Yuichiro Hosoi, Junpei Tanabe, Kathleen Bennett
PLOS ONE.2024; 19(2): e0298000. CrossRef - Occupation-based interventions to improve occupational performance and participation in the hospital setting: a systematic review
Gemma Wall, Stephen Isbel, Louise Gustafsson, Claire Pearce
Disability and Rehabilitation.2023; : 1. CrossRef - The effect of five activities daily living on improving cognitive function in ischemic stroke patients
Frana Andrianur, Dwi Prihatin Era, Arifin Hidayat, Ismansyah Ismansyah, Diah Setiani
Healthcare in Low-resource Settings.2023;[Epub] CrossRef - Effect of Upper Limb Motor Rehabilitation on Cognition in Parkinson’s Disease: An Observational Study
Valentina Varalta, Elisa Evangelista, Anna Righetti, Giovanni Morone, Stefano Tamburin, Alessandro Picelli, Cristina Fonte, Michele Tinazzi, Ilaria Antonella Di Vico, Andreas Waldner, Mirko Filippetti, Nicola Smania
Brain Sciences.2022; 12(12): 1684. CrossRef
- Intervention and assessment of executive dysfunction in patients with stroke: A scoping review
- The Effects of the Korean Medicine Health Care Program on Stroke-Related Factors and Self-Care Enhancement
- Kyoung-Oh Chang, Jung-Hye Lim
- Osong Public Health Res Perspect. 2019;10(5):307-314. Published online October 31, 2019
- DOI: https://doi.org/10.24171/j.phrp.2019.10.5.07
- 4,925 View
- 180 Download
-
 Abstract
Abstract
 PDF
PDF Objectives This study was performed to examine the effects of the Korean medicine healthcare program on stroke-related factors and self-care enhancement.
Methods This study was a quasi-experimental, pretest-posttest nonequivalent control group design study (
N = 58 participants), with 28 in the treatment group (Korean medicine health care program) and 30 in the control group (no intervention). The program was conducted twice a week for 2 hours, for a total of 12 weeks.Results There were statistically significant differences in systolic (
p = 0.005) and diastolic blood pressure (p = 0.006), cholesterol (p < 0.001), blood glucose (p < 0.001), self-esteem (p = 0.001), self-efficacy (p < 0.001), health perception (p < 0.001), and the health behavior (p < 0.001) between the experimental group and the control group.Conclusion Thus, the Korean medicine healthcare program was effective in managing stroke-related factors and enhancing self-care, and should be actively used to develop community health promotion strategies to prevent strokes and prepare long-term measures.
- The Effect of a Complex Intervention Program for Unilateral Neglect in Patients with Acute-Phase Stroke: A Randomized Controlled Trial
- Hyun-Se Choi, Deok-Ju Kim, Yeong-Ae Yang
- Osong Public Health Res Perspect. 2019;10(5):265-273. Published online October 31, 2019
- DOI: https://doi.org/10.24171/j.phrp.2019.10.5.02
- 6,078 View
- 248 Download
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Objectives The purpose of this study was to examine the combined effects of Prism Adaptation (PA) plus functional electrical stimulation (FES) on stroke patients with unilateral neglect, and suggest a new intervention method for acute-phase stroke patients.
Methods There were 30 patients included in this study from April to October 2016 that had unilateral neglect whilst hospitalized following a stroke (diagnosed by a professional). The participants, who were patients receiving occupational therapy, understood the purpose of the study and agreed to participate. The patients were randomly divided into 3 groups: PA plus FES group (Group A), PA group (Group B), and FES group (Group C). Treatments lasted for 50 minutes per day, 5 times per week, for 3 weeks in total. Reevaluation was conducted after 3 weeks of intervention.
Results All 3 groups showed unilateral neglect reduction after the intervention, but PA plus FES (complex intervention method) was more effective than PA or FES alone [effect size: Motor-free Visual Perception Test (0.80), Albert test (0.98), CBS (0.92)].
Conclusion The results of this study support further studies to examine complex intervention for the treatment of unilateral neglect.
-
Citations
Citations to this article as recorded by- Inclusion of People With Aphasia in Stroke Trials: A Systematic Search and Review
Ciara Shiggins, Brooke Ryan, Farhana Dewan, Julie Bernhardt, Robyn O'Halloran, Emma Power, Richard I. Lindley, Gordon McGurk, Miranda L. Rose
Archives of Physical Medicine and Rehabilitation.2024; 105(3): 580. CrossRef - Prism adaptation combined with eye movement training for unilateral spatial neglect after stroke: Study protocol for a single-blind prospective, randomized controlled trial
Yu-xuan Yang, Ling-ling Wang, Juan Du, Yao-min Luo, Yu-lei Xie, Bo Zhang, Han Zhang
Frontiers in Neurology.2023;[Epub] CrossRef - No short-term treatment effect of prism adaptation for spatial neglect: An inclusive meta-analysis
Orsolya Székely, Antonia F. Ten Brink, Alexandra G. Mitchell, Janet H. Bultitude, Robert D. McIntosh
Neuropsychologia.2023; 189: 108566. CrossRef - A Complex Intervention Integrating Prism Adaptation and Neck Vibration for Unilateral Neglect in Patients of Chronic Stroke: A Randomised Controlled Trial
Hyun-Se Choi, Bo-Min Lee
International Journal of Environmental Research an.2022; 19(20): 13479. CrossRef - Non-pharmacological interventions for spatial neglect or inattention following stroke and other non-progressive brain injury
Verity Longley, Christine Hazelton, Calvin Heal, Alex Pollock, Kate Woodward-Nutt, Claire Mitchell, Gorana Pobric, Andy Vail, Audrey Bowen
Cochrane Database of Systematic Reviews.2021;[Epub] CrossRef
- Inclusion of People With Aphasia in Stroke Trials: A Systematic Search and Review
- Dual Task Training Effects on Upper Extremity Functions and Performance of Daily Activities of Chronic Stroke Patients
- JuHyung Park
- Osong Public Health Res Perspect. 2019;10(1):2-5. Published online February 28, 2019
- DOI: https://doi.org/10.24171/j.phrp.2019.10.1.02
- 4,981 View
- 109 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Objectives The purpose of this research was to study the influences of dual task training on upper extremity function and performance of daily activities of chronic stroke patients.
Methods Dual task training was performed on 21 patients who had suffered a chronic stroke with hemiplegia. The dual task training was performed for 30 minutes per session, for 5 days a week, for 3 weeks. There were 5 evaluations carried out over 3 weeks before and after the intervention. Changes in upper extremity function were measured by using the Box and block test. Changes in the performance of daily activities were measured using the Korea-Modified Barthel Index.
Results The mean upper limb function score of the chronic stroke patients increased significantly from 21.88 ± 19.99 before the intervention, to 26.22 ± 15.65 after the intervention (
p < 0.05), and the mean daily activities score increased significantly from 65.82 ± 12.04, to 67.29 ± 12.90 (p < 0.05).Conclusion Dual task training effectively improved upper extremity function, and the performance of daily activities in chronic stroke patients.
-
Citations
Citations to this article as recorded by- How does a motor or cognitive dual-task affect our sense of upper limb proprioception?
Amanda L. Ager, Ann M. Cools, Dorien Borms, Jean-Sébastien Roy, Renato S. Melo
PLOS ONE.2024; 19(3): e0299856. CrossRef - The Relationship Between Dual-Task Performance and Functional Independence in Stroke Patients
Pınar OBA, Musa POLAT
Turkish Journal of Science and Health.2022;[Epub] CrossRef - İnme Hastalarında Çift Yönlü Görev Aktivitesinin Etkinliği
Derya Tuba BAL, Tuba KOCA, Ejder BERK, Burhan Fatih KOÇYİĞİT, Vedat NACİTARHAN
Kahramanmaraş Sütçü İmam Üniversitesi Tıp Fakültes.2020; 15(3): 60. CrossRef
- How does a motor or cognitive dual-task affect our sense of upper limb proprioception?
- The Effects of Task-Oriented Circuit Training Using Rehabilitation Tools on the Upper-Extremity Functions and Daily Activities of Patients with Acute Stroke: A Randomized Controlled Pilot Trial
- Jong-Hoon Moon, Kyoung-Young Park, Hee-Jin Kim, Chang-Ho Na
- Osong Public Health Res Perspect. 2018;9(5):225-230. Published online October 31, 2018
- DOI: https://doi.org/10.24171/j.phrp.2018.9.5.03
- 5,982 View
- 141 Download
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF Objectives The purpose of this study was to investigate the effect of task-oriented circuit training (TOCT) using the rehabilitation tools for upper extremity function upon the daily life of patients with acute stroke.
Methods Eighteen patients with acute stroke were randomly allocated into either the experimental group or the control group. The experimental group performed the TOCT program using rehabilitation tools, whilst the control group had neuro-developmental treatment. Both groups received 30 minutes of treatment per session, 5~6 times per week, for 4 weeks. The assessments conducted were the Fugl-Meyer assessment, motor activity log and stroke impact scale to compare the upper extremity function and activities of daily living.
Results The results showed a significant improvement in the TOCT group compared with the neuro-developmental treatment group in the amount of motor activity use and high stroke impact score, indicating recovery (
p < 0.05).Conclusion The TOCT program using rehabilitation tools could have a positive impact on acute stroke patients use of their upper extremity.
-
Citations
Citations to this article as recorded by- What is Task-Oriented Training? A Scoping Review
Erin Halford, Samantha Jakubiszak, Kassidy Krug, Amanda Umphress
Student Journal of Occupational Therapy.2024; : 1. CrossRef - Dosages of Swallowing Exercises Prescribed in Stroke Rehabilitation: A Medical Record Audit
Jacinda Choy, Fereshteh Pourkazemi, Caitlin Anderson, Hans Bogaardt
Dysphagia.2023; 38(2): 686. CrossRef - Bobath therapy is inferior to task-specific training and not superior to other interventions in improving arm activity and arm strength outcomes after stroke: a systematic review
Simone Dorsch, Cameron Carling, Zheng Cao, Emma Fanayan, Petra L Graham, Annie McCluskey, Karl Schurr, Katharine Scrivener, Sarah Tyson
Journal of Physiotherapy.2023; 69(1): 15. CrossRef - Adaptation and clinical application of assistive device chair for bedside sitting in acute stroke phase: two case reports
Priscila Salge Mauad Rodrigues, Marcos Massao Shimano, Edimar de Oliveira, Fábio Masao Kawamura, Ana Flávia Silveira, Gustavo José Luvizutto, Luciane Aparecida Pacucci Sande de Souza
Disability and Rehabilitation: Assistive Technolog.2023; : 1. CrossRef - Development and Implementation of a New Model of Care for Patients With Stroke, Acute Hospital Rehabilitation Intensive SErvices
Nicole Langton-Frost, Stephanie Orient, Jessica Adeyemo, Mona N. Bahouth, Kelly Daley, Bingqing Ye, Annette Lavezza, April Pruski
American Journal of Physical Medicine & Rehabilita.2023; 102(2S): S13. CrossRef - Standardized circuit class group training versus individualized goal-directed group training to improve upper limb function in stroke survivors during in-patient rehabilitation: a pragmatic trial
S.G Rozevink, C.M Beerepoot, C.K van der Sluis, J.M Hijmans
Disability and Rehabilitation.2023; : 1. CrossRef - Effects of the different intensities of task-oriented training on the upper extremity motor function and self-care ability of stroke survivors: study protocol for a multiarm parallel-group randomised controlled trial in a tertiary hospital in China
Shengfeng Liu, Kai Zhang, Xuecha Li, Chunxiang Li, Mengsi Peng
BMJ Open.2023; 13(12): e074106. CrossRef - Revisiting dose and intensity of training: Opportunities to enhance recovery following stroke
Kalita Donnellan-Fernandez, Andrew Ioakim, Brenton Hordacre
Journal of Stroke and Cerebrovascular Diseases.2022; 31(11): 106789. CrossRef - Effect of Task Oriented Training on Spasticity in Post Stroke Individuals
Tanavi S. Patel, Suraj Kanase
Journal of Ecophysiology and Occupational Health.2021; 21(3): 90. CrossRef
- What is Task-Oriented Training? A Scoping Review
- Assessment of Weight Shift Direction in Chronic Stroke Patients
- So Hyun Park
- Osong Public Health Res Perspect. 2018;9(3):118-121. Published online June 30, 2018
- DOI: https://doi.org/10.24171/j.phrp.2018.9.3.06
- 4,090 View
- 40 Download
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Background In patients who have suffered a stroke, the measurement of center of pressure excursion in all directions including oblique direction, anterior-medial, anterior-lateral, posterior-medial, and posterior-lateral side is important for determining balance instability but no research has been reported.
Objectives This study investigated weight shift in all directions to determine balance instability in stroke patients, including the oblique direction, using the multi-directional functional reach test.
Methods Eleven subjects participated. Multi-directional functional reach test consisted of moving the unaffected arm as far as possible in 8 directions. The directions were as follows; anterior, middle of anterior and lateral in unaffected side, lateral in unaffected side, and middle of the posterior and lateral in unaffected side, posterior, middle of posterior and lateral in affected side, lateral in affected side, middle of anterior and lateral in affected side.
Results Movement was the lowest in the affected posterior-lateral side, followed by affected posterior, affected anterior-lateral, non-affected posterior lateral, affected lateral, non-affected lateral, non-affected anterior-lateral and anterior side (
p < 0.05).Conclusion Center of pressure excursion of the affected posterior-lateral side was the most challenging for stroke patients and their reach was lowest from posterior, to lateral, and anterior directions, whilst patients could move less on the affected side compared with the non-affected side.
-
Citations
Citations to this article as recorded by- Immediate effects of circular trunk movements on reach distance and centre of pressure distance during a multidirectional seated reach task in participants with post-stroke hemiparesis: a non-randomised controlled trial
Ryohei Nabeya, Hiromi Fujii, Toshiaki Sato
International Journal of Therapy and Rehabilitatio.2024; 31(1): 1. CrossRef - Effects of galvanic vestibular stimulation on postural righting reactions in hemiplegia
Akari Horikawa, Kazu Amimoto, Shota Horikawa, Ken Hiramoto, Masaki Nishio, Jun Yoshino, Yumi Ikeda
Neuroscience Letters.2024; 827: 137735. CrossRef - Oblique direction reach test: evaluating psychometric properties in stroke population
Rinita Mascarenhas, Akshatha Nayak, Abraham M. Joshua, Shyam K. Krishnan, Vani Lakshmi R. Iyer, Jaya Shanker Tedla, Ravi Shankar Reddy
PeerJ.2023; 11: e16562. CrossRef - Effects of the different intensities of task-oriented training on the upper extremity motor function and self-care ability of stroke survivors: study protocol for a multiarm parallel-group randomised controlled trial in a tertiary hospital in China
Shengfeng Liu, Kai Zhang, Xuecha Li, Chunxiang Li, Mengsi Peng
BMJ Open.2023; 13(12): e074106. CrossRef - Efficacy of sitting balance training with delayed visual feedback among patients with stroke: a randomized crossover clinical trial
Kota Sawa, Kazu Amimoto, Abdul Chalik Meidian, Keisuke Ishigami, Takuya Miyamoto, Chika Setoyama, Rikuya Suzuki, Miko Tamura, Mitsusuke Miyagami
Journal of Physical Therapy Science.2022; 34(8): 540. CrossRef - Evaluation of the Effect of SPIDER System Therapy on Weight Shifting Symmetry in Chronic Stroke Patients—A Randomized Controlled Trial
Paulina Magdalena Ostrowska, Rafał Studnicki, Marcin Rykaczewski, Dawid Spychała, Rita Hansdorfer-Korzon
International Journal of Environmental Research an.2022; 19(23): 16214. CrossRef - Normative reference values for functional, lateral, and oblique direction reach tests in Saudi children aged six to 15 years old and psychometric properties of the oblique direction reach test
JS Tedla, DR Sangadala, K Gular, RS Reddy, MS Alshahrani, I Ahmad, M Abohashrh
Nigerian Journal of Clinical Practice.2021; 24(4): 576. CrossRef
- Immediate effects of circular trunk movements on reach distance and centre of pressure distance during a multidirectional seated reach task in participants with post-stroke hemiparesis: a non-randomised controlled trial
- Therapeutic Intervention for Visuo-Spatial Neglect after Stroke: A Meta-Analysis of Randomized Controlled Trials
- Jae-Sung Kwon
- Osong Public Health Res Perspect. 2018;9(2):59-65. Published online April 30, 2018
- DOI: https://doi.org/10.24171/j.phrp.2018.9.2.04
- 6,020 View
- 73 Download
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Objectives The aims of this meta-analysis were to examine intervention methods of qualitatively, well-designed studies from the past 10 years for treating visuo-spatial neglect (VSN) in patients who had suffered a stroke, and to evaluate the combined effects of intervention.
Methods Studies published between 2008 and 2017 on the theme of VSN were collected from PubMed, CINAHL, and MEDLINE, representative academic databases and search engines. The PEDro scale was used for evaluating the quality of methodology. The sample size, mean, and standard deviation of identified studies were used for meta-analysis.
Results Eight studies were selected for analysis. The PEDro scores of the selected studies were ≥ 7, with 237 subjects analyzed. The results of intervention were classified into “mental function” and “activity and participation” based on the International Classification of Functioning, Disability and Health. The analyzed effect sizes for combined outcomes, mental function and, activity and participation, were 0.728 (medium effect size), 0.850 (large effect size), and 0.536 (medium effect size), respectively.
Conclusion Intervention methods for treating VSN had a short-term effect on cognitive function (visual perception). In particular, non-invasive brain stimulation therapy showed a large effect size for VSN treatment.
-
Citations
Citations to this article as recorded by- Non-pharmacological interventions for spatial neglect or inattention following stroke and other non-progressive brain injury
Verity Longley, Christine Hazelton, Calvin Heal, Alex Pollock, Kate Woodward-Nutt, Claire Mitchell, Gorana Pobric, Andy Vail, Audrey Bowen
Cochrane Database of Systematic Reviews.2021;[Epub] CrossRef - Neural Mechanisms of Spatial Attention Deficits in Trauma
Stefanie R. Russman Block, Daniel H. Weissman, Chandra Sripada, Mike Angstadt, Elizabeth R. Duval, Anthony P. King, Israel Liberzon
Biological Psychiatry: Cognitive Neuroscience and .2020; 5(10): 991. CrossRef - Updated Approach to Stroke Rehabilitation
Leroy R. Lindsay, Diane A. Thompson, Michael W. O’Dell
Medical Clinics of North America.2020; 104(2): 199. CrossRef - Implementing a Rehabilitation Protocol for Spatial Neglect Assessment and Treatment in an Acute Care Hospital
Kimberly Hreha, Peii Chen, Jennifer LaRosa, Christopher Santos, Cindy Gocon, A.M. Barrett
Journal of Acute Care Physical Therapy.2020; 11(2): 59. CrossRef - Alertness Training Improves Spatial Bias and Functional Ability in Spatial Neglect
Thomas Van Vleet, Paolo Bonato, Eric Fabara, Sawsan Dabit, Sarah‐Jane Kim, Christopher Chiu, Antonio Luigi Bisogno, Michael Merzenich, Maurizio Corbetta, Joseph DeGutis
Annals of Neurology.2020; 88(4): 747. CrossRef
- Non-pharmacological interventions for spatial neglect or inattention following stroke and other non-progressive brain injury
- Determinants of the Length of Stay in Stroke Patients
- Sang Mi Kim, Sung Wan Hwang, Eun-Hwan Oh, Jung-Kyu Kang
- Osong Public Health Res Perspect. 2013;4(6):329-341. Published online December 31, 2013
- DOI: https://doi.org/10.1016/j.phrp.2013.10.008
- 3,173 View
- 13 Download
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
The study objective was to identify the factors that influence the length of stay (LOS) in hospital for stroke patients and to provide data for managing hospital costs by managing the LOS.
Methods
This study used data from the Discharge Injury Survey of the Korea Centers for Disease Control and Prevention, which included 17,364 cases from 2005 to 2008.
Result
The LOS for stroke, cerebral infarction, intracerebral hemorrhage, and subarachnoid hemorrhage was 18.6, 15.0, 28.9, and 25.3 days, respectively. Patients who underwent surgery had longer LOS. When patients were divided based on whether they had surgery, there was a 2.4-time difference in the LOS for patients with subarachnoid hemorrhage, 2.0-time difference for patients with cerebral infarction, and 1.4-time difference for patients with intracerebral hemorrhage. The emergency route of admission and other diagnosis increased LOS, whereas hypertension and diabetic mellitus reduced LOS.
Conclusion
In the present rapidly changing hospital environments, hospitals approach an efficient policy for LOS, to maintain their revenues and quality of assessment. If LOS is used as the indicator of treatment expenses, there is a need to tackle factors that influence the LOS of stroke patients for each disease group who are divided based on whether surgery is performed or not for the proper management of the LOS. -
Citations
Citations to this article as recorded by- Teleneurocritical Care for Patients with Large Vessel Occlusive Ischemic Stroke Treated by Thrombectomy
Nick M. Murray, Scott Marshall, Robert Hoesch, Kyle Hobbs, Shawn Smith, Dean Roller, Katherine Thomas, Kevin Meier, Adrian Puttgen
Neurocritical Care.2023; 38(3): 650. CrossRef - Association Between Race and Length of Stay Among Stroke Patients: The National US Emergency Departments Data Set
Karan Patel, Kamil Taneja, Jared Wolfe, Joseph V. Campellone, Mudassir Farooqui, Santiago Ortega‐Gutierrez, James E. Siegler
Stroke: Vascular and Interventional Neurology.2023;[Epub] CrossRef - Can HRV Predict Prolonged Hospitalization and Favorable or Unfavorable Short-Term Outcome in Patients with Acute Ischemic Stroke?
Joanna Aftyka, Jacek Staszewski, Aleksander Dębiec, Aleksandra Pogoda-Wesołowska, Jan Żebrowski
Life.2023; 13(4): 856. CrossRef - Does the Implementation of a National Health Insurance Program Result in Rationing Care for Ischemic Stroke Management? Analysis of the Indonesian National Health Insurance Program
Lisda Amalia
Risk Management and Healthcare Policy.2023; Volume 16: 455. CrossRef - Teleneurocritical care is associated with equivalent billable charges to in-person neurocritical care for patients with acute stroke
Nick M. Murray, Katherine Thomas, Dean Roller, Scott Marshall, Julie Martinez, Robert Hoesch, Kyle Hobbs, Shawn Smith, Kevin Meier, Adrian Puttgen
Journal of Telemedicine and Telecare.2023; : 1357633X2311661. CrossRef - Systematic Review of Resource Use and Costs in the Hospital Management of Intracerebral Hemorrhage
Steven Mulackal Thomas, Yarin Reindorp, Brandon R. Christophe, Edward Sander Connolly
World Neurosurgery.2022; 164: 41. CrossRef - Relationship between time of referral for physiotherapy and length of stay after stroke in a Nigerian tertiary hospital: a retrospective study
A. Aderonmu Joseph, O. Obembe Adebimpe
Bulletin of Faculty of Physical Therapy.2022;[Epub] CrossRef - Predicting length of stay in patients admitted to stroke rehabilitation with severe and moderate levels of functional impairments
Alejandro García-Rudolph, Blanca Cegarra, Eloy Opisso, Josep María Tormos, Montserrat Bernabeu, Joan Saurí
Medicine.2020; 99(43): e22423. CrossRef - Propensity score matching analysis on inpatient period differences of hemorrhagic stroke survivors depending on medical insurance coverage
Sang-Mi Kim, Young Kim, Seong-A Lee
Physical Therapy Rehabilitation Science.2019; 8(2): 67. CrossRef - Does service heterogeneity have an impact on acute hospital length of stay in stroke? A UK-based multicentre prospective cohort study
Michelle Tørnes, David McLernon, Max Bachmann, Stanley Musgrave, Elizabeth A Warburton, John F Potter, Phyo Kyaw Myint
BMJ Open.2019; 9(4): e024506. CrossRef - Can differences in length of stay between Dutch university hospitals and other hospitals be explained by patient characteristics? A cross-sectional study
Janine Ghielen, Sezgin Cihangir, Karin Hekkert, Ine Borghans, Rudolf Bertijn Kool
BMJ Open.2019; 9(2): e021851. CrossRef - The Factors Associated with the Fatal Outcome of Stroke
Andjela Milojevic Samanovic, Dragan Milovanovic, Vladimir Gajic, Aleksandar Raskovic, Dragan Milojevic
Serbian Journal of Experimental and Clinical Resea.2019;[Epub] CrossRef - Evaluating the Duration of Hospitalization and Its Related Factors Among Stroke Patients
Maedeh Majidi Shad, Alia Saberi, Maryam Shakiba, Shademan Rezamasouleh
Caspian Journal of Neurological Sciences.2018; 4(15): 169. CrossRef - Racial differences in recurrent ischemic stroke risk and recurrent stroke case fatality
Karen C. Albright, Lei Huang, Justin Blackburn, George Howard, Michael Mullen, Vera Bittner, Paul Muntner, Virginia Howard
Neurology.2018;[Epub] CrossRef - Clinical Characteristics of Sleep-Disordered Breathing in Subacute Phase of Stroke
Hyunkyu Jeon, Min Kyun Sohn, Minsoo Jeon, Sungju Jee
Annals of Rehabilitation Medicine.2017; 41(4): 556. CrossRef - Subarachnoid Hemorrhage Patients Admitted to Intensive Care in Australia and New Zealand: A Multicenter Cohort Analysis of In-Hospital Mortality Over 15 Years
Andrew A. Udy, Chelsey Vladic, Edward Robert Saxby, Jeremy Cohen, Anthony Delaney, Oliver Flower, Matthew Anstey, Rinaldo Bellomo, David James Cooper, David V. Pilcher
Critical Care Medicine.2017; 45(2): e138. CrossRef
- Teleneurocritical Care for Patients with Large Vessel Occlusive Ischemic Stroke Treated by Thrombectomy



 First
First Prev
Prev


