Search
- Page Path
- HOME > Search
- Psychiatric adverse events associated with the COVID-19 vaccines approved in the Republic of Korea: a systematic review
- Seungeun Ryoo, Miyoung Choi, Nam-Kyong Choi, Hyoung-Shik Shin, Jun Hee Woo, Byung-Joo Park, Sanghoon Oh
- Received October 31, 2023 Accepted January 16, 2024 Published online March 28, 2024
- DOI: https://doi.org/10.24171/j.phrp.2023.0325 [Epub ahead of print]
- 214 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - This systematic review evaluated psychiatric adverse events (AEs) following vaccination against coronavirus disease 2019 (COVID-19). We included studies that reported or investigated psychiatric AEs in individuals who had received an approved COVID-19 vaccine in the Republic of Korea. Systematic electronic searches of Ovid-Medline, Embase, CENTRAL, and KoreaMed databases were conducted on March 22, 2023. Risk of bias was assessed using the Risk of Bias Assessment Tool for Non-randomized Studies 2.0. The study protocol was registered in the International Prospective Register of Systematic Reviews (CRD42023449422). Of the 301 articles initially selected, 7 were included in the final analysis. All studies reported on sleep disturbances, and 2 highlighted anxiety-related AEs. Sleep disorders like insomnia and narcolepsy were the most prevalent AEs, while depression was not reported. Our review suggests that these AEs may have been influenced by biological mechanisms as well as the broader psychosocial context of the COVID-19 pandemic. Although this study had limitations, such as a primary focus on the BNT162b2 vaccine and an observational study design, it offered a systematic, multi-vaccine analysis that fills a critical gap in the existing literature. This review underscores the need for continued surveillance of psychiatric AEs and guides future research to investigate underlying mechanisms, identify risk factors, and inform clinical management.
- Predictors of outcomes 3 to 12 months after traumatic brain injury: a systematic review and meta-analysis
- Younes Iderdar, Maryem Arraji, Nadia Al Wachami, Morad Guennouni, Karima Boumendil, Yassmine Mourajid, Noureddine Elkhoudri, Elmadani Saad, Mohamed Chahboune
- Osong Public Health Res Perspect. 2024;15(1):3-17. Published online February 5, 2024
- DOI: https://doi.org/10.24171/j.phrp.2023.0288
- 840 View
- 56 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 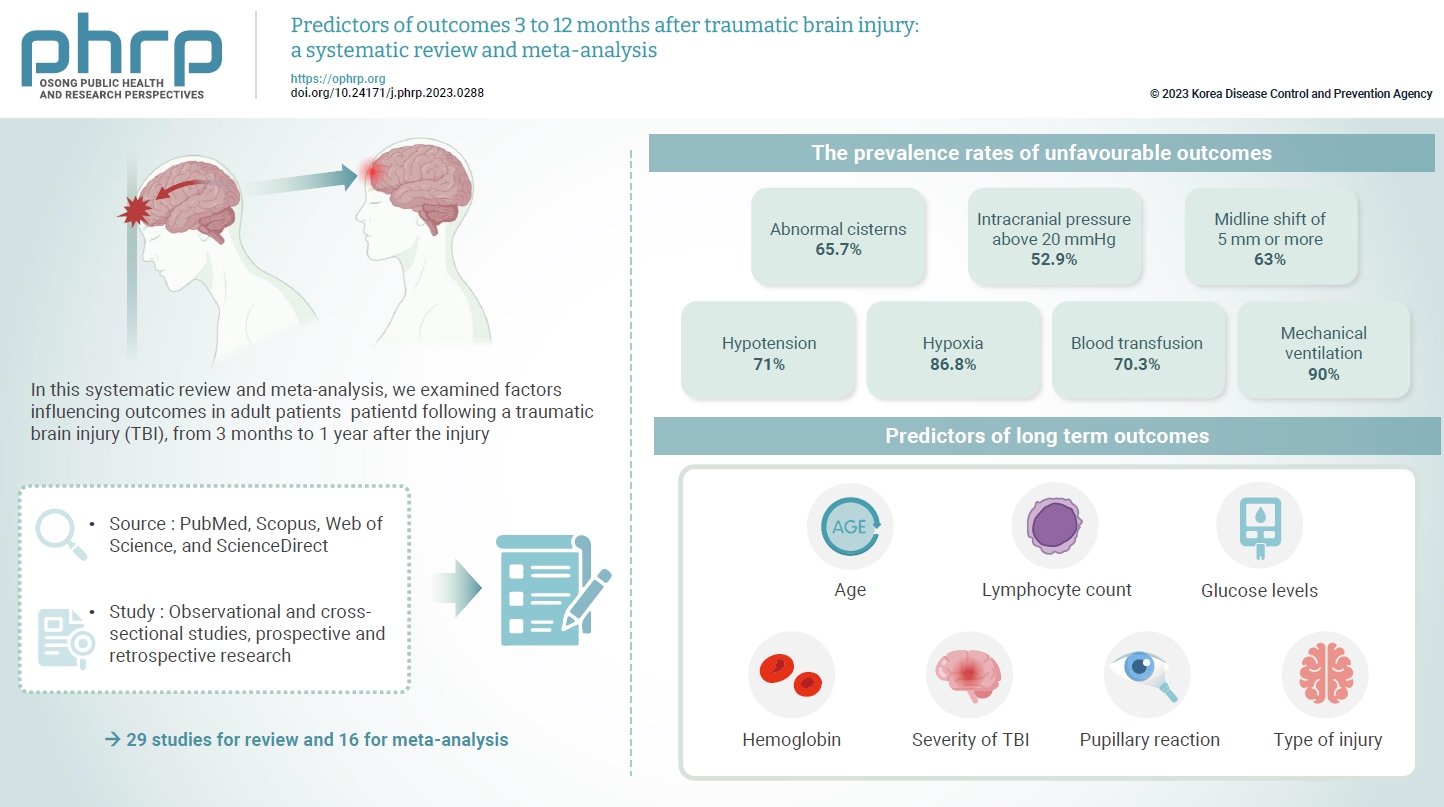
- The exact factors predicting outcomes following traumatic brain injury (TBI) remain elusive. In this systematic review and meta-analysis, we examined factors influencing outcomes in adult patients with TBI, from 3 months to 1 year after injury. A search of four electronic databases—PubMed, Scopus, Web of Science, and ScienceDirect—yielded 29 studies for review and 16 for meta-analysis, in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines. In patients with TBI of any severity, mean differences were observed in age (8.72 years; 95% confidence interval [CI], 4.77–12.66 years), lymphocyte count (−0.15 109/L; 95% CI, −0.18 to −0.11), glucose levels (1.20 mmol/L; 95% CI, 0.73–1.68), and haemoglobin levels (−0.91 g/dL; 95% CI, −1.49 to −0.33) between those with favourable and unfavourable outcomes. The prevalence rates of unfavourable outcomes were as follows: abnormal cisterns, 65.7%; intracranial pressure above 20 mmHg, 52.9%; midline shift of 5 mm or more, 63%; hypotension, 71%; hypoxia, 86.8%; blood transfusion, 70.3%; and mechanical ventilation, 90%. Several predictors were strongly associated with outcome. Specifically, age, lymphocyte count, glucose level, haemoglobin level, severity of TBI, pupillary reaction, and type of injury were identified as potential predictors of long-term outcomes.
- Behavioral interventions for smoking cessation among adolescents: a rapid review and meta-analysis for the Korea Preventive Services Task Force
- Younglee Choi, Cheol Min Lee, Belong Cho, Eon Sook Lee, Seung-Won Oh, Naae Lee, Jae Moon Yun
- Osong Public Health Res Perspect. 2021;12(3):177-186. Published online June 2, 2021
- DOI: https://doi.org/10.24171/j.phrp.2021.0018
- 9,316 View
- 161 Download
- 2 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Objectives
The aim of this study was to evaluate the effectiveness of behavioral smoking cessation interventions among adolescents.
Methods
MEDLINE, CENTRAL, Embase, CINAHL, KoreaMed, and KMbase were searched from inception to June 2020. Systematic reviews (SRs) or meta-analyses of randomized controlled trials (RCTs) were initially searched to perform a rapid SR. After selecting the final SR, RCTs after the publication year of the selected SR were searched. The primary outcome was smoking status after at least 6 months of follow-up, and the secondary outcome was smoking status at 4 weeks. Two reviewers independently assessed the selected studies’ quality using the Cochrane risk of bias tool. The meta-analysis utilized a Mantel-Haenszel fixed-effect model reporting the relative risk (RR) and 95% confidence interval (CI). The subgroup analysis utilized Cochrane’s Q.
Results
Thirty-two RCTs (11,637 participants) from a single SR were meta-analyzed. After 6 months of follow-up, the intervention group had significantly higher abstinence rates (RR, 1.30; 95% CI, 1.20−1.41; I2=26.46%). At 4 weeks of follow-up, the intervention group also had significantly higher abstinence rates (RR, 1.92; 95% CI, 1.49–2.47; I2=0.00%). The subgroup analysis indicated a significant difference in the abstinence rate according to the study setting and the period between intervention completion and follow-up.
Conclusion
This review showed that adolescent behavioral smoking cessation intervention programs significantly increased abstinence rates compared to the usual care. -
Citations
Citations to this article as recorded by- Effectiveness of Healthcare Interventions on Smoking Cessation in Adolescents in Low- and Middle-Income Countries: A Narrative Review
Janhvi Thakur, Sonali G Choudhari
Cureus.2024;[Epub] CrossRef - Non-pharmacological interventions for smoking cessation: analysis of systematic reviews and meta-analyses
Tao Nian, Kangle Guo, Wendi Liu, Xinxin Deng, Xiaoye Hu, Meng Xu, Fenfen E, Ziyi Wang, Guihang Song, Kehu Yang, Xiuxia Li, Wenru Shang
BMC Medicine.2023;[Epub] CrossRef - Behavioral Interventions for Smoking Cessation in Adolescents: Korea Preventive Services Task Force Guidance
Younglee Choi, Cheol Min Lee, Jae Moon Yun, Eon Sook Lee, Seung-Won Oh, Naae Lee, Belong Cho
Journal of the Korean Society for Research on Nico.2021; 12(1): 1. CrossRef - Tobacco Control Policy in Period of Epidemic “COVID 19”
Eon Sook Lee
Journal of the Korean Society for Research on Nico.2021; 12(1): 34. CrossRef
- Effectiveness of Healthcare Interventions on Smoking Cessation in Adolescents in Low- and Middle-Income Countries: A Narrative Review
- COVID-19 Patients: A Systematic Review and Meta-Analysis of Laboratory Findings, Comorbidities, and Clinical Outcomes Comparing Medical Staff versus the General Population
- Mina Ebrahimi, Amal Saki Malehi, Fakher Rahim
- Osong Public Health Res Perspect. 2020;11(5):269-279. Published online October 22, 2020
- DOI: https://doi.org/10.24171/j.phrp.2020.11.5.02
- 8,379 View
- 124 Download
- 11 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material This review compared coronavirus disease 2019 (COVID-19) laboratory findings, comorbidities, and clinical outcomes in patients from the general population versus medical staff to aid diagnosis of COVID-19 in a more timely, efficient, and accurate way. Electronic databases were searched up to 23rd March, 2020. The initial search yielded 6,527 studies. Following screening, 24 studies were included [18 studies (11,564 cases) of confirmed COVID-19 cases in the general public, and 6 studies (394 cases) in medical staff] in this review. Significant differences were observed in white blood cell counts (
p < 0.001), lymphocyte counts (p < 0.001), platelet counts (p = 0.04), procalcitonin levels (p < 0.001), lactate dehydrogenase levels (p < 0.001), and creatinine levels (p = 0.03) when comparing infected medical staff with the general public. The mortality rate was higher in the general population than in medical staff (8% versus 2%). This review showed that during the early stages of COVID-19, laboratory findings alone may not be significant predictors of infection and may just accompany increasing C-reactive protein levels, erythrocyte sedimentation rates, and lactate dehydrogenase levels. In the symptomatic stage, the lymphocyte and platelet counts tended to decrease. Elevated D-dimer fibrin degradation product was associated with poor prognosis.-
Citations
Citations to this article as recorded by- microRNA-185 Inhibits SARS-CoV-2 Infection through the Modulation of the Host’s Lipid Microenvironment
Nadine Ahmed, Magen E. Francis, Noreen Ahmed, Alyson A. Kelvin, John Paul Pezacki
Viruses.2023; 15(9): 1921. CrossRef - Protective action of natural and induced immunization against the occurrence of delta or alpha variants of SARS-CoV-2 infection: a test-negative case-control study
Giovanni Corrao, Matteo Franchi, Federico Rea, Danilo Cereda, Antonio Barone, Catia Rosanna Borriello, Petra Giulia Della Valle, Michele Ercolanoni, Ida Fortino, Jose Jara, Olivia Leoni, Francesco Mazziotta, Elisabetta Pierini, Giuseppe Preziosi, Marcello
BMC Medicine.2022;[Epub] CrossRef - Balancing Benefits and Harms of COVID-19 Vaccines: Lessons from the Ongoing Mass Vaccination Campaign in Lombardy, Italy
Giovanni Corrao, Federico Rea, Matteo Franchi, Danilo Cereda, Antonio Barone, Catia Rosanna Borriello, Giulia Petra Della Valle, Michele Ercolanoni, Jose Jara, Giuseppe Preziosi, Manuel Maffeo, Francesco Mazziotta, Elisabetta Pierini, Francesco Lecis, Pie
Vaccines.2022; 10(4): 623. CrossRef - Vulnerability Predictors of Post-Vaccine SARS-CoV-2 Infection and Disease—Empirical Evidence from a Large Population-Based Italian Platform
Giovanni Corrao, Matteo Franchi, Danilo Cereda, Francesco Bortolan, Olivia Leoni, Catia Rosanna Borriello, Petra Giulia Della Valle, Marcello Tirani, Giovanni Pavesi, Antonio Barone, Michele Ercolanoni, Jose Jara, Massimo Galli, Guido Bertolaso
Vaccines.2022; 10(6): 845. CrossRef - Factors associated with severe or fatal clinical manifestations of SARS‐CoV‐2 infection after receiving the third dose of vaccine
Giovanni Corrao, Matteo Franchi, Danilo Cereda, Francesco Bortolan, Olivia Leoni, Jose Jara, Giuseppina Valenti, Giovanni Pavesi
Journal of Internal Medicine.2022; 292(5): 829. CrossRef - Role of multiresolution vulnerability indices in COVID-19 spread in India: a Bayesian model-based analysis
Rupam Bhattacharyya, Anik Burman, Kalpana Singh, Sayantan Banerjee, Subha Maity, Arnab Auddy, Sarit Kumar Rout, Supriya Lahoti, Rajmohan Panda, Veerabhadran Baladandayuthapani
BMJ Open.2022; 12(11): e056292. CrossRef - A novel multi-omics-based highly accurate prediction of symptoms, comorbid conditions, and possible long-term complications of COVID-19
Debmalya Barh, Sandeep Tiwari, Bruno Silva Andrade, Marianna E. Weener, Aristóteles Góes-Neto, Vasco Azevedo, Preetam Ghosh, Kenneth Blum, Nirmal Kumar Ganguly
Molecular Omics.2021; 17(2): 317. CrossRef - Clinical and laboratory factors associated with coronavirus disease 2019 (Covid‐19): A systematic review and meta‐analysis
Le Huu Nhat Minh, Ali Ahmed‐Fouad Abozaid, Nam Xuan Ha, Loc Le Quang, Abdelrahman Gamil Gad, Ranjit Tiwari, Tran Nhat‐Le, Dinh Kim Quyen, Balqees AL‐Manaseer, Nguyen Dang Kien, Nguyen Lam Vuong, Ahmad Helmy Zayan, Le Huu Hanh Nhi, Kadek Agus Surya Dila, J
Reviews in Medical Virology.2021;[Epub] CrossRef - Epidemiologic and Clinic Characteristics of the First Wave of the COVID-19 Pandemic in Hospitalized Patients from Galați County
Mihaela-Camelia Vasile, Anca-Adriana Arbune, Gabriela Lupasteanu, Constantin-Marinel Vlase, George-Cosmin Popovici, Manuela Arbune
Journal of Clinical Medicine.2021; 10(18): 4210. CrossRef - Human Amniotic Fluid for the Treatment of Hospitalized, Symptomatic, and Laboratory-verified SARS-CoV-2 Patients
Mojgan Barati, Fakher Rahim
The Open Biology Journal.2021; 9(1): 36. CrossRef - Stratification of the risk of developing severe or lethal Covid-19 using a new score from a large Italian population: a population-based cohort study
Giovanni Corrao, Federico Rea, Flavia Carle, Salvatore Scondotto, Alessandra Allotta, Vito Lepore, Antonio D'Ettorre, Cinzia Tanzarella, Patrizia Vittori, Sabrina Abena, Marica Iommi, Liana Spazzafumo, Michele Ercolanoni, Roberto Blaco, Simona Carbone, Cr
BMJ Open.2021; 11(11): e053281. CrossRef
- microRNA-185 Inhibits SARS-CoV-2 Infection through the Modulation of the Host’s Lipid Microenvironment
- Epidemiological and Clinical Features of People with Malta Fever in Iran: A Systematic Review and Meta-Analysis
- Mahmood Moosazadeh, Roja Nikaeen, Ghasem Abedi, Motahareh Kheradmand, Saeid Safiri
- Osong Public Health Res Perspect. 2016;7(3):157-167. Published online June 30, 2016
- DOI: https://doi.org/10.1016/j.phrp.2016.04.009
- 3,327 View
- 21 Download
- 17 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
Numerous studies have reported the epidemiological and clinical features of Malta fever incidence in Iran. Review and synthesis of the related literature through meta-analysis can provide an appropriate measurement for aforementioned indices. Therefore, the present study aimed to determine the epidemiological and clinical features of people with Malta fever in Iran.
Methods
The required documents were obtained through searching national and international databases. In each study, standard deviation of the indices was calculated using binomial distribution formulas. Finally, the heterogeneity index was determined between studies using Cochran (Q) and I2 tests.
Results
Combining the results of 47 articles in the meta-analysis indicated that 57.6% (55.02–60.1%) and 42.3% (49.8–44.9%) of the patients were male and female, respectively. Most of the patients lived in rural areas; 68.4% (63.6–73.2%) compared to 31.4% (26.7–36.3%). In addition, 20.8% (17.4–24.2%) of the patients were ranchers and farmers, 16.9% (14.5–19.4%) were students, and 31.6% (27–36.2%) were housewives. Of the patients studies, 50.5% (35.6–65.2%) experienced contact with animals and 57.1% (46.4–67.9%) used unpasteurized dairy products. Fever, joint pain, and sweating were detected among 65.7% (53.7–77.8%) and 55.3% (44.4–66.2%), respectively.
Conclusion
The present study revealed that the frequency of male patients with brucellosis was considerably more than that of female patients. The number of patients with Malta fever in rural areas was significantly more than in urban areas. High-risk behavior, unprotected contact with animals, and using unpasteurized dairy products were among the most significant factors affecting Malta fever incidence in Iran. Fever, joint pain, and sweating were detected among most of the patients with Malta fever. -
Citations
Citations to this article as recorded by- A study of rural populations’ knowledge, attitude, and practice about brucellosis: a descriptive, cross-sectional, multicenter study
Zahra Montaseri, Zahra Mohebi, Rahil Masoumi, Azizallah Dehghan, Mostafa Bijani
BMC Research Notes.2024;[Epub] CrossRef - Diagnostic significance of hematological parameters in brucellosis
Mehmet Çelik, Mehmet Reşat Ceylan, Deniz Altındağ, Nevin Güler Dinçer, Sevil Alkan
Journal of Clinical Medicine of Kazakhstan.2023; 20(1): 50. CrossRef - Presence of Brucella spp. in Milk and Dairy Products: A Comprehensive Review and Its Perspectives
Md. Sadequl Islam, Md. Ariful Islam, Md. Moshiur Rahman, Khaleda Islam, Md. Mominul Islam, Md. Murtuza Kamal, Md. Nazrul Islam, Gianfranco Picone
Journal of Food Quality.2023; 2023: 1. CrossRef - Predicting of Bacteremia in Patients with Brucellosis Using Machine Learning Methods
Mehmet ÇELİK, Mehmet Reşat CEYLAN, Deniz ALTINDAĞ, Sait Can YÜCEBAŞ, Nevin GÜLER DİNCER, Sevil ALKAN
Journal of Contemporary Medicine.2023; 13(3): 459. CrossRef - Toponyms in dermatology
Heera Ramesh, Sachin Somashekar
Indian Journal of Dermatology.2022; 67(3): 279. CrossRef - Brucella pleurisy: An extremely rare complication of brucellosis
Ahmad Alikhani, Hamideh Abbaspour Kasgari, Haadi Majidi, Zahra Nekoukar
Clinical Case Reports.2022;[Epub] CrossRef - Design and validation of brucellosis prevention questionnaire focused on animal vaccination
Farhad Bahadori, Fazlollah Ghofranipour, Saeideh Ghaffarifar, Reza Ziaei
BMC Public Health.2021;[Epub] CrossRef - Forecasting the monthly incidence rate of brucellosis in west of Iran using time series and data mining from 2010 to 2019
Hadi Bagheri, Leili Tapak, Manoochehr Karami, Zahra Hosseinkhani, Hamidreza Najari, Safdar Karimi, Zahra Cheraghi, Esteban Tlelo-Cuautle
PLOS ONE.2020; 15(5): e0232910. CrossRef - Epidemiologically characteristics of human brucellosis and antimicrobial susceptibility pattern of Brucella melitensis in Hinggan League of the Inner Mongolia Autonomous Region, China
Hai-Tao Yuan, Cheng-Ling Wang, Li-Na Liu, Dan Wang, Dan Li, Zhen-Jun Li, Zhi-Guo Liu
Infectious Diseases of Poverty.2020;[Epub] CrossRef - Brucellosis: Evaluation of Two Hundred and Ten Cases with Different Clinical Features
Esma Eroglu, Bahar Kandemir
Annals of the Academy of Medicine, Singapore.2020; 49(7): 462. CrossRef - A comparison of three data mining time series models in prediction of monthly brucellosis surveillance data
Nasrin Shirmohammadi‐Khorram, Leili Tapak, Omid Hamidi, Zohreh Maryanaji
Zoonoses and Public Health.2019; 66(7): 759. CrossRef - Human brucellosis caused by raw dairy products: A review on the occurrence, major risk factors and prevention
Maryam Dadar, Youcef Shahali, Adrian M. Whatmore
International Journal of Food Microbiology.2019; 292: 39. CrossRef - Epidemiological, Clinical and Paraclinical Evaluation of Recorded Cases with Brucellosis in Kermanshah Province Health Center 2012 - 2016
Hossein Hatami, Ali Ramezankhani, Farahnaz Shekarchi
Journal of Kermanshah University of Medical Scienc.2019;[Epub] CrossRef - Epidemiological, risk factors, clinical, and laboratory features of brucellosis in the Southwest of Iran within 2009–2015
Mahmood Nabavi, Hossein Hatami, Hedayatollah Jamaliarand
International Journal of Preventive Medicine.2019; 10(1): 108. CrossRef - Meta-Analysis of the Changes of Peripheral Blood T Cell Subsets in Patients with Brucellosis
Rongjiong Zheng, Songsong Xie, Shaniya Niyazi, Xiaobo Lu, Lihua Sun, Yan Zhou, Yuexin Zhang, Kai Wang
Journal of Immunology Research.2018; 2018: 1. CrossRef - A Systematic Review and Meta-Analysis of Epidemiology and Clinical Manifestations of Human Brucellosis in China
Rongjiong Zheng, Songsong Xie, Xiaobo Lu, Lihua Sun, Yan Zhou, Yuexin Zhang, Kai Wang
BioMed Research International.2018; 2018: 1. CrossRef - The clinical features of 590 patients with brucellosis in Xinjiang, China with the emphasis on the treatment of complications
Bin Jia, Fengbo Zhang, Ying Lu, Wenbao Zhang, Jun Li, Yuexin Zhang, Jianbing Ding, Mazin Barry
PLOS Neglected Tropical Diseases.2017; 11(5): e0005577. CrossRef
- A study of rural populations’ knowledge, attitude, and practice about brucellosis: a descriptive, cross-sectional, multicenter study
- Exposure to Dichlorodiphenyltrichloroethane and the Risk of Breast Cancer: A Systematic Review and Meta-analysis
- Jae-Hong Park, Eun Shil Cha, Yousun Ko, Myung-Sil Hwang, Jin-Hwan Hong, Won Jin Lee
- Osong Public Health Res Perspect. 2014;5(2):77-84. Published online April 30, 2014
- DOI: https://doi.org/10.1016/j.phrp.2014.02.001
- 3,253 View
- 25 Download
- 23 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
This study extended and updated a meta-analysis of the association between exposure to dichlorodiphenyltrichloroethane (DDT) and the risk of breast cancer.
Methods
We reviewed the published literature on exposure to DDE and breast cancer risk to update a meta-analysis from 2004. The total of 35 studies included 16 hospital-based case–control studies, 11 population-based case–control studies, and 10 nested case–control studies identified through keyword searches in the PubMed and EMBASE databases.
Results
The summary odds ratio (OR) for the identified studies was 1.03 (95% confidence interval 0.95–1.12) and the overall heterogeneity in the OR was observed (I2 = 40.9; p = 0.006). Subgroup meta-analyses indicated no significant association between exposure to DDE and breast cancer risk by the type of design, study years, biological specimen, and geographical region of the study, except from population-based case–control studies with estimated DDE levels in serum published in 1990s.
Conclusion
Existing studies do not support the view that DDE increases the risk of breast cancer in humans. However, further studies incorporating more detailed information on DDT exposure and other potential risk factors for breast cancer are needed. -
Citations
Citations to this article as recorded by- Validation and green profile assessment of a binary solvent liquid phase microextraction method for the determination of chlorbenside and fenobucarb in lake and wastewater samples by GC–MS
Dotse Selali Chormey
Environmental Science and Pollution Research.2023; 30(15): 44697. CrossRef - Putative interactions between transthyretin and endosulfan II and its relevance in breast cancer
Saurabh Sharma, Lakshay Malhotra, Paromita Mukherjee, Navneet Kaur, Thammineni Krishanlata, Chittur V. Srikanth, Vandana Mishra, Basu Dev Banerjee, Abdul Samath Ethayathulla, Radhey Shyam Sharma
International Journal of Biological Macromolecules.2023; 235: 123670. CrossRef - Exposure to Organochlorine Pesticides and Female Breast Cancer Risk According to Molecular Receptors Expression: a Systematic Review and Meta-analysis of Epidemiological Evidence
Rodrigo Ugalde-Resano, Brenda Gamboa-Loira, Ángel Mérida-Ortega, Alma Rincón-Rubio, Gisela Flores-Collado, Maricela Piña-Pozas, Lizbeth López-Carrillo
Current Environmental Health Reports.2023; 10(4): 442. CrossRef - Mosquito control exposures and breast cancer risk: analysis of 1071 cases and 2096 controls from the Ghana Breast Health Study
Naomie Olivos, Jim E. Banta, Rhonda Spencer-Hwang, Daniel Ansong, Laura E. Beane Freeman, Joe-Nat Clegg-Lamptey, Beatrice Wiafe-Addai, Lawrence Edusei, Ernest Adjei, Nicholas Titiloye, Florence Dedey, Francis Aitpillah, Joseph Oppong, Verna Vanderpuye, Er
Breast Cancer Research.2023;[Epub] CrossRef - Endocrine disrupting chemicals and breast cancer: a systematic review of epidemiological studies
Murphy Lam Yim Wan, Vanessa Anna Co, Hani El-Nezami
Critical Reviews in Food Science and Nutrition.2022; 62(24): 6549. CrossRef - Epidemiology beyond its limits
Lauren E. McCullough, Maret L. Maliniak, Avnika B. Amin, Julia M. Baker, Davit Baliashvili, Julie Barberio, Chloe M. Barrera, Carolyn A. Brown, Lindsay J. Collin, Alexa A. Freedman, David C. Gibbs, Maryam B. Haddad, Eric W. Hall, Sarah Hamid, Kristin R. V
Science Advances.2022;[Epub] CrossRef - Plasma concentrations of chlorinated persistent organic pollutants and their predictors in the general population of Algiers, Algeria
El Hadia Mansouri, Mohamed Reggabi
Emerging Contaminants.2021; 7: 35. CrossRef - Association between type 2 diabetes and exposure to chlorinated persistent organic pollutants in Algeria: A case-control study
El Hadia Mansouri, Mohamed Reggabi
Chemosphere.2021; 264: 128596. CrossRef - Extraction of Chlorobenzenes and PCBs from Water by ZnO Nanoparticles
Yuntao Zhang, Ran Chen, Jim E. Riviere, Jeffrey Comer
Processes.2021; 9(10): 1764. CrossRef - Two Cases of Possible Familial Chronic Myeloid Leukemia in a Family with Extensive History of Cancer
Marisa J.L. Aitken, Christopher B. Benton, Ghayas C. Issa, Koji Sasaki, Musa Yilmaz, Nicholas J. Short
Acta Haematologica.2021; 144(5): 585. CrossRef - In utero DDT exposure and breast density before age 50
Nickilou Y. Krigbaum, Piera M. Cirillo, Julie D. Flom, Jasmine A. McDonald, Mary Beth Terry, Barbara A. Cohn
Reproductive Toxicology.2020; 92: 85. CrossRef - DDT exposure during pregnancy and DNA methylation alterations in female offspring in the Child Health and Development Study
Hui-Chen Wu, Barbara A. Cohn, Piera M. Cirillo, Regina M. Santella, Mary Beth Terry
Reproductive Toxicology.2020; 92: 138. CrossRef - Prediagnostic serum concentrations of organochlorine pesticides and non-Hodgkin lymphoma: A nested case–control study in the Norwegian Janus Serum Bank Cohort
Dazhe Chen, Tom K. Grimsrud, Hilde Langseth, Dana B. Barr, Bryan A. Bassig, Aaron Blair, Kenneth P. Cantor, Marilie D. Gammon, Qing Lan, Nathaniel Rothman, Lawrence S. Engel
Environmental Research.2020; 187: 109515. CrossRef - Global trends in pesticides: A looming threat and viable alternatives
Akanksha Sharma, Ananya Shukla, Kriti Attri, Megha Kumar, Puneet Kumar, Ashish Suttee, Gurpal Singh, Ravi Pratap Barnwal, Neha Singla
Ecotoxicology and Environmental Safety.2020; 201: 110812. CrossRef - Exposure to Endocrine Disrupting Chemicals and Risk of Breast Cancer
Louisane Eve, Béatrice Fervers, Muriel Le Romancer, Nelly Etienne-Selloum
International Journal of Molecular Sciences.2020; 21(23): 9139. CrossRef - Breast Cancer and Exposure to Organochlorines in the CECILE Study: Associations with Plasma Levels Measured at the Time of Diagnosis and Estimated during Adolescence
Delphine Bachelet, Marc-André Verner, Monica Neri, Émilie Cordina Duverger, Corinne Charlier, Patrick Arveux, Sami Haddad, Pascal Guénel
International Journal of Environmental Research an.2019; 16(2): 271. CrossRef - Risk of breast cancer and adipose tissue concentrations of polychlorinated biphenyls and organochlorine pesticides: a hospital-based case-control study in Chinese women
Wenlong Huang, Yuanfang He, Jiefeng Xiao, Yuanni Huang, Anna Li, Meirong He, Kusheng Wu
Environmental Science and Pollution Research.2019; 26(31): 32128. CrossRef - Serum levels of Organochlorine Pesticides and Breast Cancer Risk in Iranian Women
Parisa Paydar, Gholamreza Asadikaram, Hossein Fallah, Hamid Zeynali Nejad, Hamed Akbari, Moslem Abolhassani, Vahid Moazed, Payam Khazaeli, Mahmoud Reza Heidari
Archives of Environmental Contamination and Toxico.2019; 77(4): 480. CrossRef - DDT exposure in early childhood and female breast cancer: Evidence from an ecological study in Taiwan
Simon Chang, Sonia El-Zaemey, Jane Heyworth, Meng-chi Tang
Environment International.2018; 121: 1106. CrossRef - Chiral pharmaceuticals: Environment sources, potential human health impacts, remediation technologies and future perspective
Yaoyu Zhou, Shikang Wu, Hao Zhou, Hongli Huang, Jia Zhao, Yaocheng Deng, Hua Wang, Yuan Yang, Jian Yang, Lin Luo
Environment International.2018; 121: 523. CrossRef - Organochlorine pesticides accumulation and breast cancer: A hospital-based case–control study
Ting-Ting He, An-Jun Zuo, Ji-Gang Wang, Peng Zhao
Tumor Biology.2017; 39(5): 101042831769911. CrossRef - Correlation between toxic organochlorine pesticides and breast cancer
SA Eldakroory, DA El Morsi, RH Abdel-Rahman, S Roshdy, MS Gouida, EO Khashaba
Human & Experimental Toxicology.2017; 36(12): 1326. CrossRef - Breast cancer and persistent organic pollutants (excluding DDT): a systematic literature review
Tafzila Akter Mouly, Leisa-Maree Leontjew Toms
Environmental Science and Pollution Research.2016; 23(22): 22385. CrossRef
- Validation and green profile assessment of a binary solvent liquid phase microextraction method for the determination of chlorbenside and fenobucarb in lake and wastewater samples by GC–MS
- Obesity and Asian Americans in the United States: Systematic Literature Review
- Sanggon Nam
- Osong Public Health Res Perspect. 2013;4(4):187-193. Published online August 31, 2013
- DOI: https://doi.org/10.1016/j.phrp.2013.06.001
- 2,776 View
- 19 Download
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
Obesity is one of the most serious health problems in the world today. Asian Americans are usually less overweight and obese than African Americans and Hispanic Americans, but the rate of obesity in Asian Americans is still increasing, especially in younger generations. This research examines Asian American obesity using existing research, as a means of finding the need for greater emphasis on Asian American obesity intervention research.
Methods
In this research literature review, Asian American obesity using existing research as a means of finding the need for greater emphasis on Asian American obesity intervention research is examined. A systematic review is done in order to find Asian American obesity research, due to the minimal amount of existing studies. In total, there were only nine papers which were not duplicates and which still met the criteria for inclusion, from an initial 106 papers.
Results
There is very little research on obesity in Asian Americans. Although the rate of obesity among Asian Americans is increasing, there are few related articles, projects, and surveys, and there is little information. There is a need for more specific and in-depth analysis of Asian American obesity. Asian Americans are associated with a lower waist circumference (WC) and BMI, while Hawaiian/Pacific Islanders are associated with a higher WC and BMI. Typically, Asian Americans who were born in the United States (US) tend to be overweight and more obese than those born in foreign countries.
Conclusion
Based on this literature review, it is concluded that there is a shortage of Asian American obesity research, even though there is an evident need for particular obesity intervention programs that target Asian Americans. -
Citations
Citations to this article as recorded by- Southern California Asian Americans and the Obesity Epidemic: A Qualitative Study to Improve Understanding and Cultural Competence
Alyssa Mae Carlos, Kathleen Doll
American Journal of Health Education.2023; 54(6): 463. CrossRef - The posterior tibial artery free flap for head and neck reconstruction
Alexandra E. Kejner
Current Opinion in Otolaryngology & Head & Neck Su.2022; 30(5): 358. CrossRef - Heterogeneity in Obesity Prevalence Among Asian American Adults
Nilay S. Shah, Cecily Luncheon, Namratha R. Kandula, Sadiya S. Khan, Liping Pan, Cathleen Gillespie, Fleetwood Loustalot, Jing Fang
Annals of Internal Medicine.2022; 175(11): 1493. CrossRef - Fruit and Vegetable Consumption Behavior Among Asian Americans: A Thematic Analysis
Chia-Liang Dai, Manoj Sharma, Taj Haider, Hema Sunchu
Journal of Primary Care & Community Health.2021; 12: 215013272098477. CrossRef - The effect of racial discrimination on mental and physical health: A propensity score weighting approach
Shanting Chen, Allen B. Mallory
Social Science & Medicine.2021; 285: 114308. CrossRef - Ethnic Enclaves and Pregnancy and Behavior Outcomes Among Asian/Pacific Islanders in the USA
Andrew D. Williams, Lynne C. Messer, Jenna Kanner, Sandie Ha, Katherine L. Grantz, Pauline Mendola
Journal of Racial and Ethnic Health Disparities.2020; 7(2): 224. CrossRef - Developing a Socioculturally Nuanced Systems Model of Childhood Obesity in Manhattan’s Chinese American Community via Group Model Building
Ewelina Swierad, Terry T.-K. Huang, Ellis Ballard, Karen Flórez, Sheng Li
Journal of Obesity.2020; 2020: 1. CrossRef - Healthy Living Behaviors Among Chinese–American Preschool-Aged Children: Results of a Parent Survey
Virginia Rall Chomitz, Alison Brown, Victoria Lee, Aviva Must, Kenneth Kwan Ho Chui
Journal of Immigrant and Minority Health.2018; 20(4): 926. CrossRef - Obesity Prevention Behaviors in Asian Indian Adolescent Girls: A Pilot Study
Annie Thomas, Linda Janusek
Journal of Pediatric Nursing.2018; 42: 9. CrossRef - Filipinos Fit and Trim - A feasible and efficacious DPP-based intervention trial
Melinda S. Bender, Bruce A. Cooper, Elena Flowers, Raymond Ma, Shoshana Arai
Contemporary Clinical Trials Communications.2018; 12: 76. CrossRef - The neighborhood environment and obesity: Understanding variation by race/ethnicity
Michelle S. Wong, Kitty S. Chan, Jessica C. Jones-Smith, Elizabeth Colantuoni, Roland J. Thorpe, Sara N. Bleich
Preventive Medicine.2018; 111: 371. CrossRef - STRIVE, San Diego! Methodology of a Community-Based Participatory Intervention to Enhance Healthy Dining at Asian and Pacific Islander Restaurants
Sarah Oropeza, Mary Grace Sadile, Chantine Nguyen Phung, Moana Cabiles, Sandy Spackman, Myleen Abuan, Fe Seligman, Maria Rosario Araneta
Journal of Nutrition Education and Behavior.2018; 50(3): 297. CrossRef - Geographic differences in obesity prevalence and its risk factors among Asian Americans: findings from the 2013–2014 California Health Interview Survey
Shaoqing Gong, Kesheng Wang, Ying Li, Arsham Alamian
Scientific Reports.2018;[Epub] CrossRef - American Heart Association’s Ideal Cardiovascular Health Metrics in Under-Represented Asian Americans
Freda Patterson, Guo Zhang, Adam Davey, Yin Tan, Grace X. Ma
Journal of Community Health.2016; 41(6): 1282. CrossRef - Genes and the intergenerational transmission of BMI and obesity
Timothy J. Classen, Owen Thompson
Economics & Human Biology.2016; 23: 121. CrossRef
- Southern California Asian Americans and the Obesity Epidemic: A Qualitative Study to Improve Understanding and Cultural Competence



 First
First Prev
Prev


