Search
- Page Path
- HOME > Search
- Impact of long COVID-19 on posttraumatic stress disorder as modified by health literacy: an observational study in Vietnam
- Han Thi Vo, Tien Duc Dao, Tuyen Van Duong, Tan Thanh Nguyen, Binh Nhu Do, Tinh Xuan Do, Khue Minh Pham, Vinh Hai Vu, Linh Van Pham, Lien Thi Hong Nguyen, Lan Thi Huong Le, Hoang Cong Nguyen, Nga Hoang Dang, Trung Huu Nguyen, Anh The Nguyen, Hoan Van Nguyen, Phuoc Ba Nguyen, Hoai Thi Thanh Nguyen, Thu Thi Minh Pham, Thuy Thi Le, Thao Thi Phuong Nguyen, Cuong Quoc Tran, Kien Trung Nguyen
- Osong Public Health Res Perspect. 2024;15(1):33-44. Published online February 19, 2024
- DOI: https://doi.org/10.24171/j.phrp.2023.0261
- 663 View
- 52 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 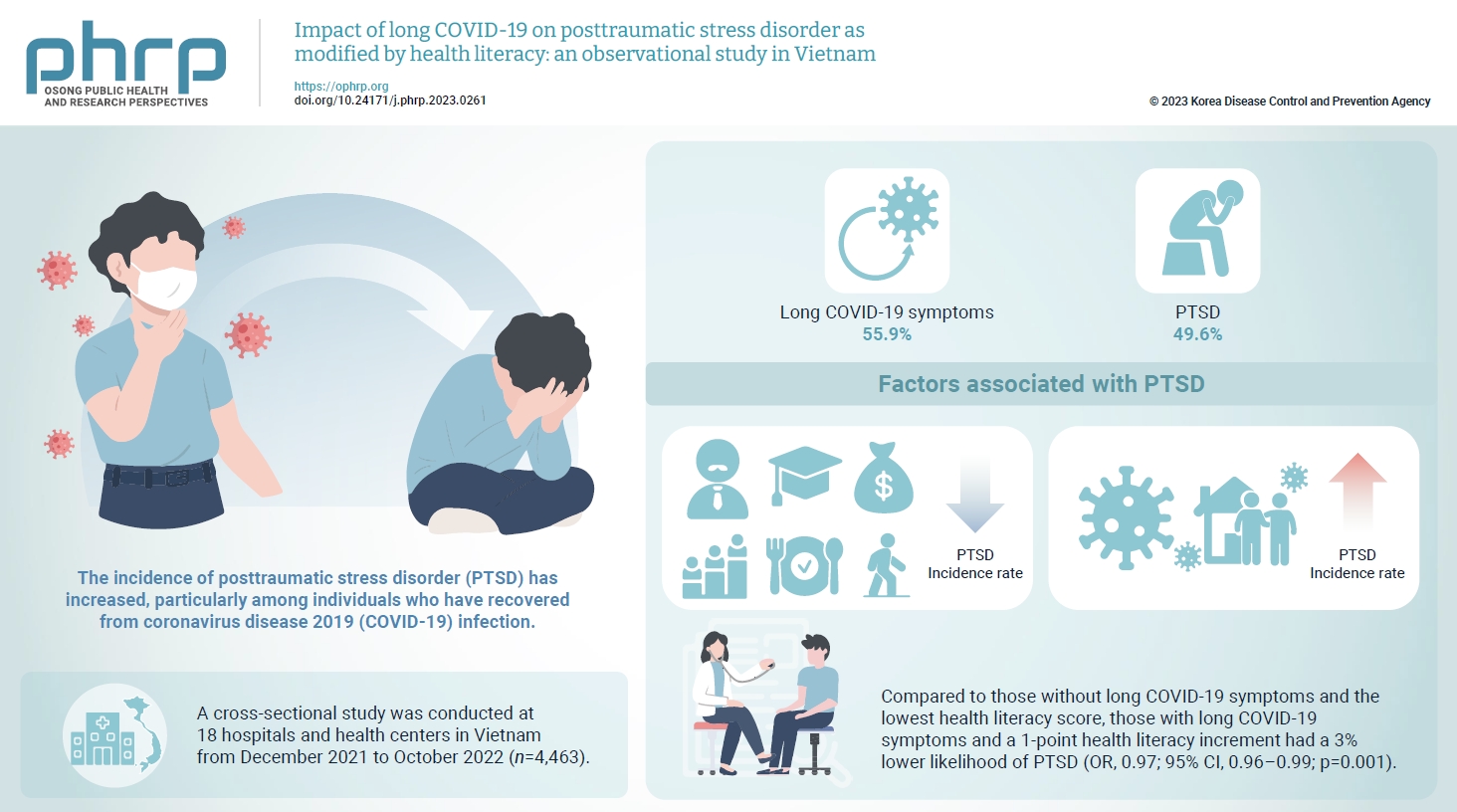
- Objectives
The prevalence of posttraumatic stress disorder (PTSD) has increased, particularly among individuals who have recovered from coronavirus disease 2019 (COVID-19) infection. Health literacy is considered a “social vaccine” that helps people respond effectively to the pandemic. We aimed to investigate the association between long COVID-19 and PTSD, and to examine the modifying role of health literacy in this association. Methods: A cross-sectional study was conducted at 18 hospitals and health centers in Vietnam from December 2021 to October 2022. We recruited 4,463 individuals who had recovered from COVID-19 infection for at least 4 weeks. Participants provided information about their sociodemographics, clinical parameters, health-related behaviors, health literacy (using the 12-item short-form health literacy scale), long COVID-19 symptoms and PTSD (Impact Event Scale-Revised score of 33 or higher). Logistic regression models were used to examine associations and interactions. Results: Out of the study sample, 55.9% had long COVID-19 symptoms, and 49.6% had PTSD. Individuals with long COVID-19 symptoms had a higher likelihood of PTSD (odds ratio [OR], 1.86; 95% confidence interval [CI], 1.63–2.12; p<0.001). Higher health literacy was associated with a lower likelihood of PTSD (OR, 0.98; 95% CI, 0.97–0.99; p=0.001). Compared to those without long COVID-19 symptoms and the lowest health literacy score, those with long COVID-19 symptoms and a 1-point health literacy increment had a 3% lower likelihood of PTSD (OR, 0.97; 95% CI, 0.96–0.99; p=0.001). Conclusion: Health literacy was found to be a protective factor against PTSD and modified the negative impact of long COVID-19 symptoms on PTSD.
- Predictors of outcomes 3 to 12 months after traumatic brain injury: a systematic review and meta-analysis
- Younes Iderdar, Maryem Arraji, Nadia Al Wachami, Morad Guennouni, Karima Boumendil, Yassmine Mourajid, Noureddine Elkhoudri, Elmadani Saad, Mohamed Chahboune
- Osong Public Health Res Perspect. 2024;15(1):3-17. Published online February 5, 2024
- DOI: https://doi.org/10.24171/j.phrp.2023.0288
- 914 View
- 65 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 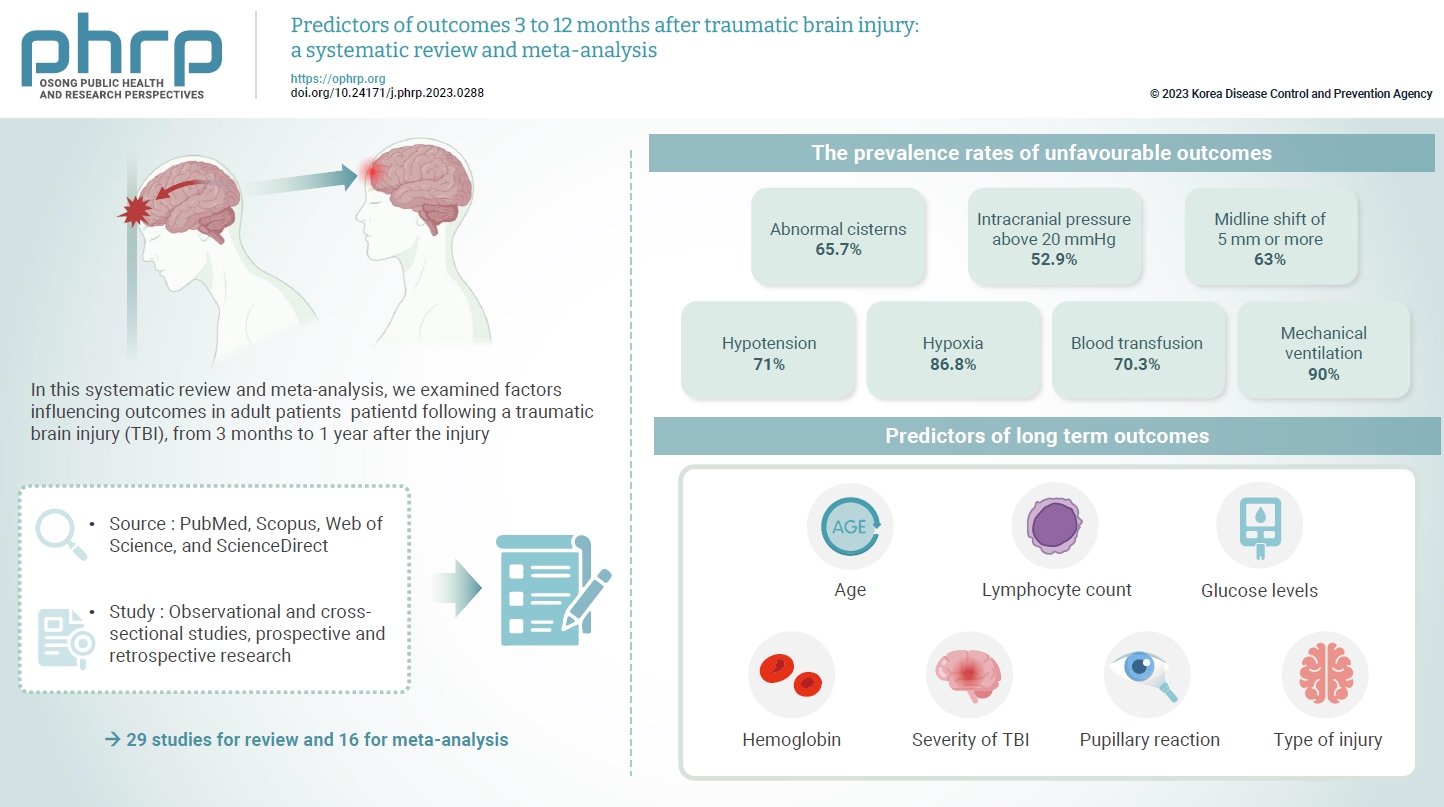
- The exact factors predicting outcomes following traumatic brain injury (TBI) remain elusive. In this systematic review and meta-analysis, we examined factors influencing outcomes in adult patients with TBI, from 3 months to 1 year after injury. A search of four electronic databases—PubMed, Scopus, Web of Science, and ScienceDirect—yielded 29 studies for review and 16 for meta-analysis, in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines. In patients with TBI of any severity, mean differences were observed in age (8.72 years; 95% confidence interval [CI], 4.77–12.66 years), lymphocyte count (−0.15 109/L; 95% CI, −0.18 to −0.11), glucose levels (1.20 mmol/L; 95% CI, 0.73–1.68), and haemoglobin levels (−0.91 g/dL; 95% CI, −1.49 to −0.33) between those with favourable and unfavourable outcomes. The prevalence rates of unfavourable outcomes were as follows: abnormal cisterns, 65.7%; intracranial pressure above 20 mmHg, 52.9%; midline shift of 5 mm or more, 63%; hypotension, 71%; hypoxia, 86.8%; blood transfusion, 70.3%; and mechanical ventilation, 90%. Several predictors were strongly associated with outcome. Specifically, age, lymphocyte count, glucose level, haemoglobin level, severity of TBI, pupillary reaction, and type of injury were identified as potential predictors of long-term outcomes.
- Impacts of Social Distancing During the COVID-19 Outbreaks in Korea: Level 1 Trauma Center Data of Domestic Incidents and Intentional Injury
- Ye Rim Chang, Kyoung Min Kim, Hyo Joung Kim, Dong Hun Kim, Jeonsang Kim, Dongsub Noh, Dae Sung Ma, Jeongseok Yun, Jung-Ho Yun, Seok Won Lee, Seok Ho Choi, Yoonjung Heo, Sung Wook Chang
- Osong Public Health Res Perspect. 2020;11(6):345-350. Published online December 22, 2020
- DOI: https://doi.org/10.24171/j.phrp.2020.11.6.02
- 7,274 View
- 165 Download
- 6 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF Objectives As a protective measure to slow down the transmission of coronavirus disease 2019 in Korea, social distancing was implemented from February 29th, 2020. This study aimed to evaluate the prevalence of domestic incidents and intentional injury during March 2020 when social distancing was in effect.
Methods There were 12,638 patients who visited the Level 1 trauma center of Chungnam province with injuries from domestic incidents, familial discord, and intentional injury. The prevalence of injuries during March 2020 was compared with the average of the previous 5 years, and the average for every March between 2015 and 2019.
Results The prevalence of domestic incidents in March 2020 was significantly higher than the 5-year average, and the average for every March from 2015 to 2019 (
p < 0.001). Familial discord (p = 0.002) and intentional injury (p = 0.031) were more frequently observed in March 2020. Adolescents showed a markedly higher level of intentional injury in March 2020 than in both the 5-year average (p = 0.031), and average for every March over the previous 5 years (p = 0.037).Conclusion The prevalence of domestic incidents and intentional injury were significantly higher during the period of social distancing in Korea. There is a need for social consensus, better policies, and psychological support services, especially if faced with a second or third wave of coronavirus disease.
-
Citations
Citations to this article as recorded by- The Global Landscape of Domestic Violence against Women during the COVID-19 Pandemic: A Narrative Review
Priya Dharishini Kunasagran, Khalid Mokti, Mohd Yusof Ibrahim, Syed Sharizman Syed Abdul Rahim, Freddie Robinson, Adora J Muyou, Sheila Miriam Mujin, Nabihah Ali, Gary Goh Chun Chao, Rudi Nasib, Abraham Chiu En Loong, Nachia Banu Abdul Rahim, Mohd Hafizud
Korean Journal of Family Medicine.2024; 45(1): 3. CrossRef - Changes in interpersonal violence and utilization of trauma recovery services at an urban trauma center in the United States during the COVID-19 pandemic: a retrospective, comparative study
Kevin Y. Zhu, Kristie J. Sun, Mary A. Breslin, Mark Kalina Jr., Tyler Moon, Ryan Furdock, Heather A. Vallier
Journal of Trauma and Injury.2024; 37(1): 60. CrossRef - Impact of the COVID-19 Pandemic on Adolescent Self-Harm: Based on a National Emergency Department Information System
Ju-Hyeon Park, Young-Woo Seo, Seungbum Chae
International Journal of Environmental Research an.2023; 20(5): 4666. CrossRef - Changes in Injury Pattern and Outcomes of Trauma Patients after COVID-19 Pandemic: A Retrospective Cohort Study
Myungjin Jang, Mina Lee, Giljae Lee, Jungnam Lee, Kangkook Choi, Byungchul Yu
Healthcare.2023; 11(8): 1074. CrossRef - Intimate Partner Violence in the Orthopaedic Patient Population
Jennifer A. Kunes, Marisa N. Ulrich, Charlotte E. Orr, Lisa K. Cannada, Christen M. Russo
JBJS Reviews.2023;[Epub] CrossRef - Characteristics of Attempted and Completed Suicides During the COVID-19 Pandemic
Nathan Flesher, Marisa-Nicole Zayat, Elizabeth Ablah, Hayrettin Okut, Kelly Lightwine, James M. Haan
The American Surgeon™.2023; 89(12): 5795. CrossRef - Comparison of Clinical Characteristics of Traumatic Brain Injury Patients According to the Mechanism Before and After COVID-19
Jonghyun Sung, Jongwook Choi, Kum Whang, Sung Min Cho, Jongyeon Kim, Seung Jin Lee, Yeon gyu Jang
Korean Journal of Neurotrauma.2023; 19(3): 307. CrossRef - Effect of the COVID‐19 pandemic at a major Danish trauma center in 2020 compared with 2018–2019: A retrospective cohort study
Frederik Trier, Jesper Fjølner, Nikolaj Raaber, Anders H. Sørensen, Hans Kirkegaard
Acta Anaesthesiologica Scandinavica.2022; 66(2): 265. CrossRef - Impact of the COVID-19 lockdown on trauma team activations in a single major Lithuanian trauma center: A retrospective single-center study
Vytautas Aukstakalnis, Kristina Blaziene, Juozas Cepla, Greta Vileitaite, Kestutis Stasaitis, Dinas Vaitkaitis
International Journal of Critical Illness and Inju.2022; 12(1): 17. CrossRef - Transmission parameters of coronavirus disease 2019 in South Asian countries
Mridul Sannyal, Abul Mukid Md. Mukaddes
Osong Public Health and Research Perspectives.2022; 13(3): 191. CrossRef - The impact of the COVID-19 pandemic on presentations to health services following self-harm: systematic review
Sarah Steeg, Ann John, David J. Gunnell, Nav Kapur, Dana Dekel, Lena Schmidt, Duleeka Knipe, Ella Arensman, Keith Hawton, Julian P. T. Higgins, Emily Eyles, Catherine Macleod-Hall, Luke A. McGuiness, Roger T. Webb
The British Journal of Psychiatry.2022; 221(4): 603. CrossRef
- The Global Landscape of Domestic Violence against Women during the COVID-19 Pandemic: A Narrative Review
- Perceived Psychological Traumatic Childbirth in Iranian Mothers: Diagnostic Value of Coping Strategies
- Sedigheh Abdollahpour, Seyed Abbas Mousavi, Habibollah Esmaily, Ahmad Khosrav
- Osong Public Health Res Perspect. 2019;10(2):72-77. Published online April 30, 2019
- DOI: https://doi.org/10.24171/j.phrp.2019.10.2.05
- 22,124 View
- 45 Download
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Objectives The aim of this study was to investigate the diagnostic value of a stress coping scale for predicting perceived psychological traumatic childbirth in mothers.
Methods This cross-sectional study was performed on 400 new mothers (within 48 hours of childbirth). Psychological traumatic childbirth was evaluated using the 4 diagnostic criteria of Diagnostic and Statistical Manual of Mental Disorders. Coping was measured using Moss and Billings’ Stress Coping Strategies Scale.
Results The overall mean score of stress coping was 29 ± 14.2. There were 193 (43.8%) mothers that had experienced a psychological traumatic childbirth. A stress coping score ≤ 30, with a sensitivity of 90.16 (95% CI = 85.1–94.0), and a specificity of 87.44 (95% CI = 82.1–91.6), was determined as a predictor of psychological traumatic childbirth. So that among mothers with stress coping scores ≤ 30, 87% had experienced a psychological traumatic childbirth.
Conclusion Investigating the degree of coping with stress can be used as an accurate diagnostic tool for psychological traumatic childbirth. It is recommended that during pregnancy, problem-solving and stress management training programs be used as psychological interventions for mothers with low levels of stress control. This will ensure that they can better cope with traumatic childbirth and post-traumatic stress in the postpartum stage.
-
Citations
Citations to this article as recorded by- Validity and reliability of the Chinese version of traumatic childbirth perception scale in Chinese women
Caifeng Chen, Xiaoying Wang, Han Xu, Xuejie Liu, Yuhong Li
Current Psychology.2024; 43(8): 7205. CrossRef - Relationship between Experience of Antepartum Intervention and Posttraumatic
Stress Symptoms Following Childbirth: A Prospective Study
Sedigheh Abdollahpour, Mona Larki, Najme Rajabi, Elham Azmoude
Current Women s Health Reviews.2023;[Epub] CrossRef - The Effect of Labor Dance on Traumatic Childbirth Perception and Comfort: A Randomized Controlled Study
Bihter Akin, Hülya Yurteri Türkmen, Hacer Yalnız Dilcen, Ebru Sert
Clinical Nursing Research.2022; 31(5): 909. CrossRef - The relationship of psychosocial well‐being and social support with pregnant women's perceptions of traumatic childbirth
Hacer Yalnız Dilcen, Filiz Aslantekin, Naciye Aktaş
Scandinavian Journal of Caring Sciences.2021; 35(2): 650. CrossRef
- Validity and reliability of the Chinese version of traumatic childbirth perception scale in Chinese women



 First
First Prev
Prev


