Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 7(4); 2016 > Article
-
Original Article
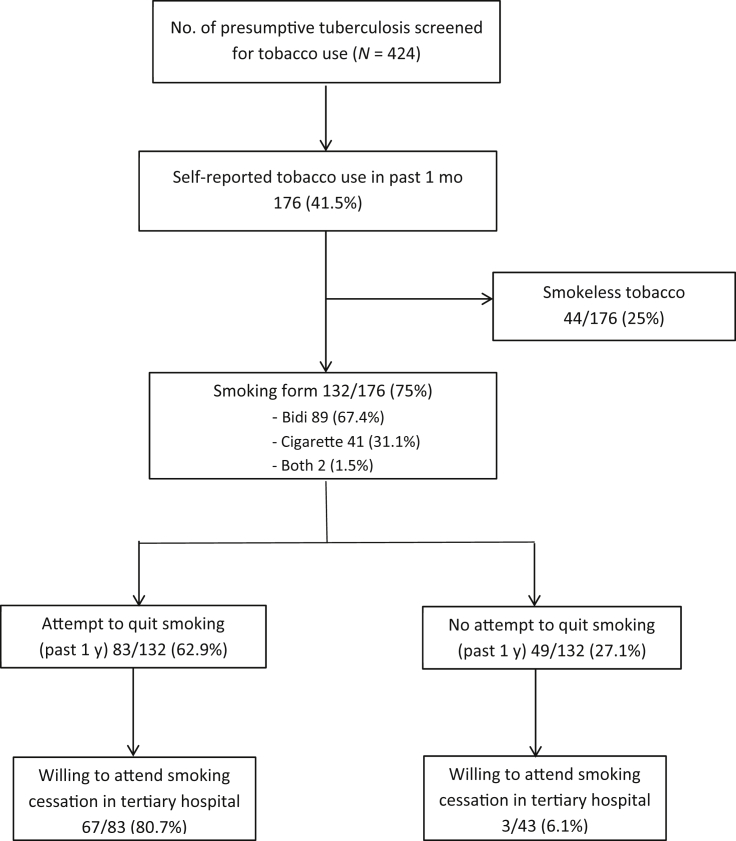
High Tobacco Use among Presumptive Tuberculosis Patients, South India: Time to Integrate Control of Two Epidemics - Kunal Pradip Kanakia, Marie Gilbert Majella, Pruthu Thekkur, Gomathi Ramaswamy, Divya Nair, Palanivel Chinnakali
-
Osong Public Health and Research Perspectives 2016;7(4):228-232.
DOI: https://doi.org/10.1016/j.phrp.2016.06.001
Published online: June 11, 2016
Department of Preventive and Social Medicine, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India
- ∗Corresponding author. palaniccm@gmail.com
• Received: September 19, 2015 • Revised: May 18, 2016 • Accepted: June 2, 2016
Copyright © 2016 Korea Centers for Disease Control and Prevention. Published by Elsevier Korea LLC.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Figure & Data
References
Citations
Citations to this article as recorded by 

- Smoking cessation interventions in South Asian Region: a systematic scoping review
Sajid Iqbal, Rubina Barolia, Pammla Petrucka, Laila Ladak, Rameesha Rehmani, Abdul Kabir
BMC Public Health.2022;[Epub] CrossRef - Tobacco use and nicotine dependence among newly diagnosed pulmonary tuberculosis patients in Ballabgarh tuberculosis unit, Haryana
Rakesh Kumar, Shashi Kant, Ankit Chandra, Anand Krishnan
Journal of Family Medicine and Primary Care.2020; 9(6): 2860. CrossRef - A narrative review of facilitators and barriers to smoking cessation and tobacco-dependence treatment in patients with tuberculosis in low- and middle-income countries
Kamila Zvolska, Alexandra Pankova, Iveta Nohavova, Rumana Huque, Helen Elsey, Melanie Boeckmann, Aziz Sheikh, Kamran Siddiqi, Eva Kralikova
Tobacco Induced Diseases.2020;[Epub] CrossRef - Effective Counseling: A Major Challenge of Tuberculosis Control Programme in Tackling the Dual Disease Burden of Tobacco Consumption among Tuberculosis Patients in India
Bidhata Khatri, K.K. Shyamala, Nehal LNU, Supriya Tiwari
Indian Journal of Respiratory Care.2020; 9(1): 77. CrossRef - Characteristics and sputum conversion of tuberculosis (TB) patients in Kalutara, Sri Lanka
Sumal Nandasena, Chaminda Senavirathna, Champa Munasinghe, Chapa Wijesena, Ridmi Sucharitharathna
Indian Journal of Tuberculosis.2019; 66(1): 76. CrossRef - Tuberculosis and cigarette smoke exposure: An update ofin vitroandin vivostudies
Y. López-Hernández, C. E. Rivas-Santiago, J. A. López, G. Mendoza-Almanza, R. Hernandez-Pando
Experimental Lung Research.2018; 44(2): 113. CrossRef


 PubReader
PubReader Cite
Cite
