Early Epidemiological and Clinical Characteristics of 28 Cases of Coronavirus Disease in South Korea
Article information
Abstract
Objectives
The first confirmed case of coronavirus disease 2019 (COVID-19) in South Korea was reported in January 2020, with 28 confirmed cases reported as of February 14th, 2020. The epidemiological and clinical characteristics of all 28 cases were analyzed in response to this disease.
Methods
The epidemiological characteristics and early clinical features of the 28 patients from Korea with confirmed COVID-19 were analyzed using COVID-19 reporting and surveillance data and the epidemiological investigation reports prepared by the rapid response team.
Results
There were 16 patients that entered Korea from foreign countries: Wuhan, China (11 patients), Zhuhai, China, (1 patient), Singapore (2 patients), Japan (1 patient), and Thailand (1 patient). The early symptoms were fever, sore throat, cough or sputum production, chills, and muscle ache. Three patients were asymptomatic, however, 18 developed pneumonia. Of the 28 cases, 16 were index cases imported from abroad, with 10 cases of secondary infection originating in Korea, and the route of transmission still under investigation for 2 patients. The 10 patients with secondary infection were infected from contact with family members or acquaintances of primary patients, and the suspected sites of transmission were mostly at home.
Conclusion
COVID-19 in Korea was spread by 16 infected individuals traveling from other countries, leading to second-generation cases. The initial symptoms were mostly minor, but the disease was infectious at this stage, resulting from close contact, particularly at home. Establishing an early detection strategy for COVID-19 is crucial for managing the transmission of the disease.
Introduction
Twenty-seven patients in Wuhan City, Hubei Province of China were reported to have pneumonia of an unknown cause on December 31st, 2019 and were subsequently reported to have a novel coronavirus infection caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). After the announcement of 41 confirmed coronavirus disease 2019 (COVID-19) cases in Wuhan City, China on January 11th, infected patients were identified in Thailand on January 13th and in Japan on January 16th. More cases were confirmed in some areas of China outside Wuhan, including Beijing and Shenzhen City, Guangdong Province on January 20th, and the number of confirmed cases has continued to rise. Moreover, there have been reports of secondary transmission from China and countries including Singapore, Japan, Thailand, Malaysia, and Vietnam into Korea [1].
In Korea, 28 confirmed cases of COVID-19 had been reported as of February 14th, since the first case was confirmed on January 20th, 2020. Of these, 16 were cases imported into the country (57.1%) and 10 were believed to be secondary cases of infections originating in Korea; in the other 2 cases, the route of transmission remained undetermined.
The initial symptoms of COVID-19 are known to be respiratory symptoms such as coughing, in association with fevers, but the disease epidemiology remains largely unknown. To treat new infections and prevent further transmission, it is necessary to analyze and share epidemiological data on the cases reported to date [2].
Materials and Methods
This is a case series of the 28 patients with confirmed COVID-19 in Korea as of February 14th, 2020. To obtain demographic, epidemiological, and early clinical information, COVID-19 reporting and surveillance data from Korea Centers for Disease Control and Prevention (KCDC), and the 28 case reports of the epidemiological investigation conducted by KCDC rapid response team was utilized.
Patient age was provided on the date of diagnosis, and key indicators such as estimated duration of exposure, date of onset of symptoms, and route of transmission were identified by an epidemiological investigator who participated in the field investigation and the epidemiological investigation team at KCDC headquarters. The incubation period was estimated based on the estimated exposure date and the date of symptom onset. However, it must be noted that the data presented in this study may change depending on the results of further epidemiological investigation.
Results
1. Response to COVID-19 in Korea
On December 31st, 2019, in Wuhan City, Hubei Province of China, 27 individuals developed pneumonia and all individuals had visited the seafood market in the area. The local centers for disease control and prevention, upon concluding that the novel infection had originated from overseas, established a “countermeasures taskforce against pneumonia of unknown cause” and set the crisis level to Blue. Accordingly, the situation overseas was constantly monitored, and surveillance in China was initiated, and responses initiated to suspected cases of infection. For suspected cases, a basic epidemiological assessment was conducted at the local health center and at the discretion of the central investigator, the patient was either admitted to a state-designated, negative-pressure isolation ward for further testing, or control measures of self-isolation and active surveillance were undertaken [3].
On January 20th, the first case of infection from abroad was confirmed in Korea. Subsequently, the crisis level was scaled up from Blue to Yellow, and KCDC headquarters for the COVID-19 rapid response team was established. On January 27th, the crisis level was scaled up from Yellow to Orange, and the Ministry of Health and Welfare Central Accident Management Headquarters for the COVID-19 was established. Currently, all ministries of the government are cooperating in response to this novel emerging infectious disease.
In particular, to block the transmission of infection among patients under quarantine, Wuhan City was designated as an endemic center for infection on January 8th. Based on the health questionnaire filled out by travelers from Wuhan at the point of entry, people with body temperature higher than 37.5°C or respiratory symptoms including coughing were classified as symptomatic and isolated for testing. On January 23rd, Wuhan airport, which has an average of 300 travelers per day, was shut down by the Chinese government, and travel restrictions were implemented later in Hubei Province, including Wuhan City.
However, between January 20th and January 28th, 4 patients who presented with symptoms outside of the Hubei province who had visited Wuhan, tested positive for SARS-CoV-2, and the number of cases outside Wuhan continued to increase. On January 28th, other areas in China where the infection was reported, were also quarantined. On February 4th, a special quarantine procedure was implemented on flights from China. The procedure not only involved the assessment of symptoms upon arrival, but also included the identification of individuals confirmed to have COVID-19 and those who had been in close contact with these infected individuals.
As of February 14th, a total of 7,242 patients were suspected of having COVID-19 and had been tested. Of those, 28 were confirmed to have COVID-19 of which 7 were discharged and 21 were treated.
2. Epidemiological characteristics
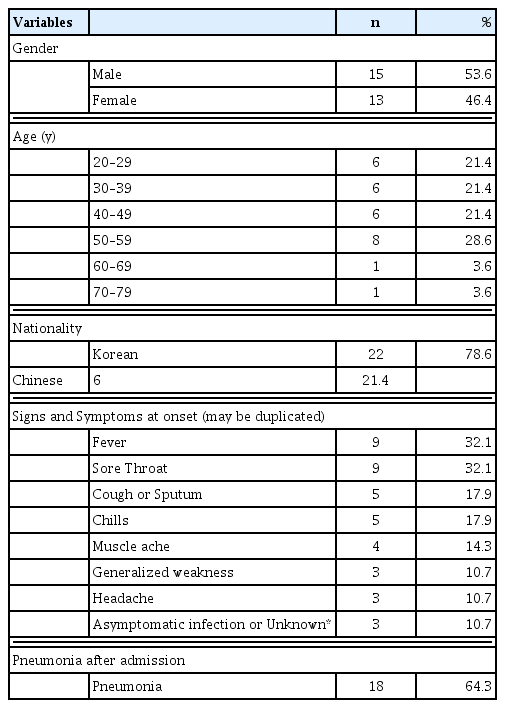
Of the 28 patients with COVID-19, 15 were men (53.6%) and 13 were women (46.1%), with a mean age of 42.6 years (range: 20–73 years). Regarding age groups, 8 patients were in their 50’s (28.6%), 6 patients each were in their 20’s, 30’s, and 40’s (21.4%), and 1 patient each was in their 60’s and 70’s (3.6%). Of the 28 patients, 22 were Korean and 6 were Chinese, of whom 2 were visitors.
Of the 16 index cases imported from abroad (57.1%), 6 contributed to the occurrence of secondary infections in 10 patients in Korea. Of those with secondary infection, 7 were first-generation patients (25.0%) and 3 were second-generation patients (10.7%). In the remaining 2 patients (7.2%), the route of transmission remains under investigation.
The initial symptoms were fever or feeling hot (9 patients, 32.1%), sore throat (9 patients, 32.1%), cough or sputum production (5 patients, 17.9%), chills (5 patients, 17.9%), and muscle ache (4 patients, 14.3%). However, 3 patients were asymptomatic. In 18 patients, pneumonia was confirmed using imaging once hospitalized (64.3%). As of February 14th, 7 out of 28 patients had been discharged, and the average length of hospital stay was 12.7 days (range: 8–19 days).
One patient had visited a marketplace in China, while 2 had visited a medical facility in Wuhan City. Of the 28 patients, 10 (35.7%) had at least 1 underlying disease including hypertension, diabetes, asthma, chronic rhinitis, dyslipidemia, and hypothyroidism, and 1 patient had undergone surgery for lung cancer (Table 1).
“Test count” refers to the number of cases that were reported to KCDC by local health centers and were then tested. Prior to February 7th, tests were conducted by KCDC and the Research Institute of Public Health and Environment in the corresponding cities/provinces, the number of reports and test counts matched. After February 7th, additional tests were conducted for each individual suspected of having COVID-19 increasing the number of reports, aside from those initially conducted by the local health center.
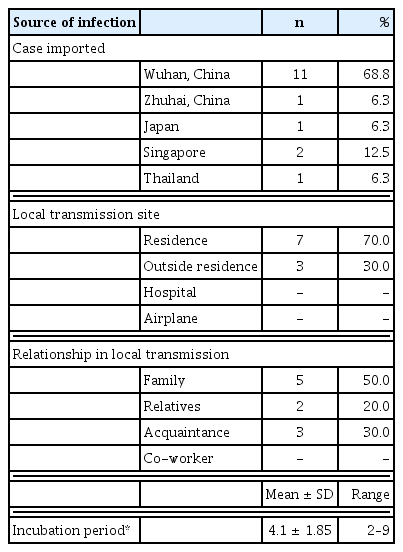
The earliest date of symptom onset among the 25 patients with a clear date of onset, was January 10th (for 3 patients, the date of onset was unclear). Since then, the number of confirmed index cases imported from abroad continued to increase, and symptoms were first confirmed in patients with secondary infection on January 26th. The incubation period was estimated to be 4.1 days based on the date of symptom onset and first exposure (among 9 patients, excluding 1 patient with an unclear date of onset) shown in Figure 1 and Table 2.
In the 16 index cases imported from abroad, the suspected sites where the infection was first contracted were Wuhan, China (11 cases, 68.3%), Singapore (2 cases, 12.5%), Zhuhai, China (1 case, 6.3%), Thailand (1 case, 6.3%), and Japan (1 case, 6.3%). The 10 patients with secondary infection for which the routes of transmission were known were either family members (7 cases, 70.0%) including relatives (2 cases), or acquaintances (3 cases, 30%) of the primary patients. The suspected sites of transmission were the home (7 cases, 70.0%), a restaurant (1 case, 10.0%), a church (1 case, 10.0%), and other locations (1 case, 10.0%).
With regard to the distribution of the 24 cases by region, excluding the 2 Wuhan residents and 2 patients who were evacuated via a charter flight, high incidence rates were reported in Gyeonggi-do (11 patients, 39.3%) and Seoul (9 patients, 32.1%), followed by Gwangju (2 patients, 7.1%), and Jeollabuk-do and Jeollanam-do (1 patient each, 3.6%) shown in Table 2.
3. Confirming the route of transmission
Regarding the course of disease development in the 28 patients with confirmed COVID-19 as of February 14th, 6 patients developed secondary infection, which they contracted from previously infected individuals, with each group including 2–6 patients (Figure 2).
The first group included the following index patients: Patient #3 was a 54-year-old man who was asymptomatic upon arrival in Korea on January 20th, but had developed a fever, chills, muscle ache, and nasal congestion by 13:00 on January 22nd. Patient #28, who was on the same flight bound from Wuhan to Korea as Patient #3, tested positive on February 10th during self-quarantine. The route of transmission is still under investigation. In addition, since Patient #28 underwent surgery following entry into the country, and was treated with antibiotics and analgesics, the exact date of onset of symptoms could not be calculated. Patient #6, an acquaintance of Patient #3, dined at a restaurant with Patient #3 on the evening of January 22nd for an hour and a half, developed symptoms including the chills on January 26th, and tested positive for COVID-19 on January 30th. Patients #10 and #11, the wife and son of Patient #6 who lived and dined at the restaurant with him, developed symptoms on January 29th and 30th, respectively, and tested positive for COVID-19. Patient #21, an acquaintance of Patient #6 who attended on January 26th, developed symptoms on January 30th and subsequently tested positive for COVID-19.
The index case imported from abroad in the second group involved Patient #5, a 32-year-old man from Wuhan who visited Korea on January 24th and started to develop aches similar to that observed in the common cold on January 26th. Patient #9, who developed a secondary infection, was an acquaintance of Patient #5 who stayed and dined at the same place as Patient #9 until January 29th. Patient #9 developed a headache on January 30th, was managed as a contact case, and tested positive on January 31st.
The third index case imported from abroad involved Patient #12, a 48-year-old man with a history of contact for business reasons, with a Japanese patient who had tested positive for COVID-19 in Japan. This was the first case imported from a country outside China. Following entry to Korea on January 19th, the patient started experiencing muscle aches on January 20th. However, COVID-19 was not suspected because he arrived in Korea from Japan, and thus reporting/testing was delayed. Patient #14 was his wife who stayed with him for more than 10 days before COVID-19 was confirmed. She developed symptoms on January 29th and subsequently tested positive.
The fourth index case involved Patient #15, a 43-year-old man who was being monitored after having close contact with Patient #4 on the plane. He developed a fever and a sore throat on February 1st and subsequently tested positive. Patient #20, a relative living in the same building but on a different floor, experienced a sore throat on February 4th and subsequently tested positive. It is likely that he was infected whilst eating with Patient #15.
The index case imported from abroad in the fifth group involved Patient #16, a 42-year-old woman who developed chills on January 25th after visiting Thailand and tested positive on February 4th. Since Patient #16 developed symptoms after visiting Bangkok and Pattaya, Thailand, between January 15th and January 19th, it is probable that she was either infected at a tourist destination in Thailand or Bangkok airport. The daughter of Patient #16 tested positive on February 5th and was designated as Patient #18. Among the other family members who dined with Patient #18 at her mother’s house on January 25th, the older brother (Patient #22) tested positive for COVID-19 on February 5th. Patients #18 and #22 were initially asymptomatic. Hence, the date of symptom onset could not be estimated. Moreover, Patient #18 had an overlapping history of visiting Thailand and a hospital visit with Patient #16 in Korea thus, the route of transmission was unclear and remained under investigation.
The sixth transmission case originating in Korea involved Patient #25, a 73-year-old woman who tested positive at a screening clinic. Later, her son (Patient #26) and daughter-in-law (Patient #27) tested positive during the process of epidemiological investigation. After patients #26 and #27 entered Korea on January 31st from Zhuhai, Guangdong Province of China, via Macau, the 3 patients remained in the same place of residence in Korea. Considering that Patient #27 developed symptoms on February 4th, earlier than Patients #25 and #26, and Patient #25 did not have any previous history of overseas travel, it is likely that Patients #25 and #26 were infected by Patient #27.
Of the 10 patients with secondary infection and known routes of transmission, 7 were family members including 2 relatives and 3 were acquaintances. All these patients either dined or resided together. Transmission from patients #3 to #6, and from patients #16 to #22 was assumed to have taken place while they dined together at the same place. Patients #6 and #21 did not dine together, but were together for 2 hours at a chapel. Regarding transmission, patients with secondary infection had a history of close contact with the primary patient including physical contact, co-dining, and co-habitation for a considerable amount of time.
In summary, of the 28 confirmed cases, 16 were index cases imported from abroad, 10 were secondary infection cases, and 2 remained under investigation to determine the route of transmission. As of February 14th, the 28 patients had come into close contact with 1,781 people, of whom 1,356 were released from surveillance, and 457 were under self-quarantine, and active surveillance. The suspected sites of transmission for the 10 patients with secondary infection were the home (7 patients, 60.0%), a restaurant, a church, and other locations (1 patient each, 8.3%). The relationship between the primary patient and patients with secondary infection were as follows: family (7 patients, 70.0%, including 2 relatives) and acquaintances (3 patients, 30.0%). This finding suggests that secondary infection occurred among individuals who were in close contact with an infected person for a considerable amount of time whilst they lived and dined together.
Discussion
Among the Korean patients, 15 were men (53.9%). It has been reported that 56%–73.2% of confirmed cases of COVID-19 in Wuhan, China are in men [4,5]. The estimated incubation period was 4.6 days to develop COVID-19, which was shorter than the period of 5.2 days reported in China [5]. The mean age of the Korean patients was 42.6 years, which was lower than the age reported in previous studies conducted in China (49 years, 55.5 years, and 59 years) [2,4,5].
Chen et al [2] and Huang et al [4] also reported that 32–51% of the hospitalized patients with confirmed COVID-19 had hypertension, diabetes, and cardiovascular diseases, while 10 of the 28 Korean patients (35.7%) had at least 1 underlying disease, including hypertension and diabetes. In addition, the early symptoms, such as a fever, coughing, a sore throat, the chills, and muscle ache, were similar to the reported symptoms of COVID-19 [4].
Currently, the COVID-19 cases originating in Korea have been reported to be index cases imported from abroad, and resultant first-generation and second-generation cases. So far, all the patients confirmed to have COVID-19 have identifiable epidemiological connections. In other words, cases of secondary infection were limited to closely related people (family and acquaintances) who spent time together co-dining and co-habiting. It is important to analyze and share such epidemiological and clinical data on COVID-19 to establish an effective response strategy.
Acknowledgments
We thank the relevant ministries, including the Ministry of Interior and Safety, cities and provinces, medical staff in health centers, and medical facilities for their effort in responding to cases of COVID-19.
Notes
Conflicts of Interest
The authors have no conflicts of interest to declare.