Health-Related Quality of Life and its Associated Factors in COVID-19 Patients
Article information
Abstract
Objectives
Health-related quality of life (HRQoL) is one of the most important outcome measures for patients. The purpose of this study was to evaluate HRQoL and related factors in Coronavirus disease 2019 (COVID-19) patients.
Methods
A total of 420 COVID-19 patients who had been discharged from hospital were selected using a systematic sampling. The EuroQol 5-dimensional-5 levels (EQ-5D-5L) questionnaire along with medical records of the patients were used to gather the data. The t test and analysis of variance were employed to test the difference between mean EQ-5D-5L scores, and the BetaMix model was used to investigate factors associated with EQ-5D-5L scores.
Results
The mean score for the patients who completed the EQ-5D-5L questionnaire (n = 409) was 0.6125. The EQ-5D-5L scores were significantly higher in males, patients with younger age, those with a low level of education, the employed, patients who worked in uncrowded workplaces, patients without diabetes, and those who were not admitted to intensive care unit. The BetaMix model showed that gender, age, education, employment status, having diabetes, heart failure, and admission to the intensive care unit were significant independent predictors of the EQ-5D-5L index values.
Conclusion
The mean score for EQ-5D-5L in COVID-19 patients was low in this study. Some of the factors, especially aging and having diabetes, should be considered in the aftercare of patients to improve their HRQoL.
Introduction
Coronavirus disease 2019 (COVID-19) is a new infectious disease that was first discovered in Wuhan, China, on the 31st December 2019 [1]. It has subsequently spread to almost all countries around the world. According to the latest report by the World Health Organization (April 25th, 2020), this disease has spread to 210 countries and territories around the world, and 2 international conveyances [2]. Iran, with more than 100,000 cases of COVID-19, and a deaths-to-infections ratio of 6.4%, is amongst the highest ranked countries in terms of outbreak and mortality [2]. The spread of COVID-19 through all 31 provinces of Iran was very rapid (less than a month) [3]. Yazd, located in center of Iran, had more than 1,500 confirmed cases of COVID-19 in Iran in June 2020.
COVID-19 is a serious disease that can significantly affect the daily lives of recovered patients and their families in terms of mental health problems such as post-traumatic stress [4], depression [5], anxiety [6] and insomnia [7], as well as the negative impact COVID-19 has on patients quality of life (QoL) [8]. Since the patients are not immune to future infection [9], it may lead to a more negative impact on patients’ QoL. Health-related quality of life (HRQoL) is an important measure that is used for assessing the impact of diseases, disorders, or disabilities on the physical, mental, and social domains of patient health. The assessment of HRQoL helps healthcare providers identify the factors affecting QoL and recognize the aspects of COVID-19 management that needs to be enhanced for improving the QoL of patients [10,11].
The EuroQol 5-dimensional-5 levels (EQ-5D-5L) questionnaire is one of the most commonly used instruments for measuring HRQoL in clinical and outcome research, and its use is recommended by the National Institute for Health and Clinical Excellence [12,13]. This instrument was translated into Persian and was confirmed by the EuroQol group [14]. This study used the EQ-5D-5L instrument to describe the HRQoL of COVID-19 patients who had been discharged from the only hospital dedicated to COVID-19 patients in Yazd, and assessed the impact of socio-demographic and clinical factors on COVID-19 patients’ HRQoL.
Materials and Methods
1. Study design and data collection
This cross-sectional study was conducted in COVID-19 patients who had been discharged from the Shahid Sadoughi hospital (dedicated to the treatment of patients with COVID-19 in Yazd). According to the medical records of COVID-19 patients, a total of 420 patients were selected in systematic sampling in March 2020.
The EQ-5D-5L questionnaire, along with socio-demographic characteristics, were completed for patients during a telephone interview. Clinical data were extracted from the medical records of patients. Oral consent was obtained from all patients before participating in the study. All procedures performed were in accordance with the ethical standards of the national research committee (approval no.: IR.BUMS.REC. 1399.109)
2. EQ-5D-5L instrument
The EQ-5D-5L is a common instrument to assess HRQoL (developed by the EuroQol group in 2011) [15]. The EQ-5D-5L includes 5 dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression). Each of the dimensions has 5 levels of response options (no problems, slight problems, moderate problems, severe problems, and unable to/extreme problems) to define all possible health states. In addition, the EQ-5D-5L questionnaire has a visual analog scale measured on a vertical line to determine the overall health status of the respondents [0 (the worst imaginable health) to 100 (the best imaginable health)] [16].
The Iranian interim EQ-5D-5L value set (generated through the crosswalk technique introduced by the EuroQoL group [17]), and the interim value set confirmed by 2 studies in Iran [18,19] were used in this current study. This technique generated the value set for the EQ-5D-5L by making a correlation between the EQ-5D-5L and the EQ-5D-3L descriptive systems.
3. Statistical analysis
Given that the distribution of EQ-5D data is commonly skewed, multimodal, and is limited at the top and the bottom, and it often has a large number of observations at the top (ceiling effects), use of basic models such as ordinary least squares (OLS) and Tobit is theoretically inappropriate for analysis of such data [20]. Recently, 2 new mixture models were developed to deal with the distributional characteristics of the EQ-5D instrument [adjusted limited dependent variable mixture model and extensions to a beta mixture model (BetaMix model)]. In this study, the betamix command was used for assessing the factors affecting HRQoL.
Data was not normally distributed (using the Kolmogorov–Smirnov test) however, the t test and ANOVA were used in this study because parametric tests had the same results as nonparametric tests. All analyses were performed using Stata\Version 15.0 for Windows (StataCorp, College Station, TX, USA).
Results
Out of 420 interviews, 11 interviews were excluded from the final analysis because data on many of the dimensions of the EQ-5D-5L questionnaire were not available. Table 1 shows the socio-demographic and clinical characteristics of patients. The mean age of patients was 58.4 ± 18.21 years, and the average of household occupancy was 2.10 ± 0.18. Among COVID-19 patients, the majority were males, aged 51 to 60 years, married, unemployed, with a primary level of education, and in a household of between 1 to 2 members, and those who worked did so in a crowded environment.
The clinical characteristics of patients are presented in Table 2. The mean duration of hospitalization and days following hospital discharge was 8 ± 7 and 21.6 ± 14.8 days, respectively. The majority of COVID-19 patients had a hospital duration of ≤ 10 days and the duration of days following hospital discharge was > 30 days. In this study, 30% of the patients who were treated in the intensive care unit (ICU) were more than 60 years old.
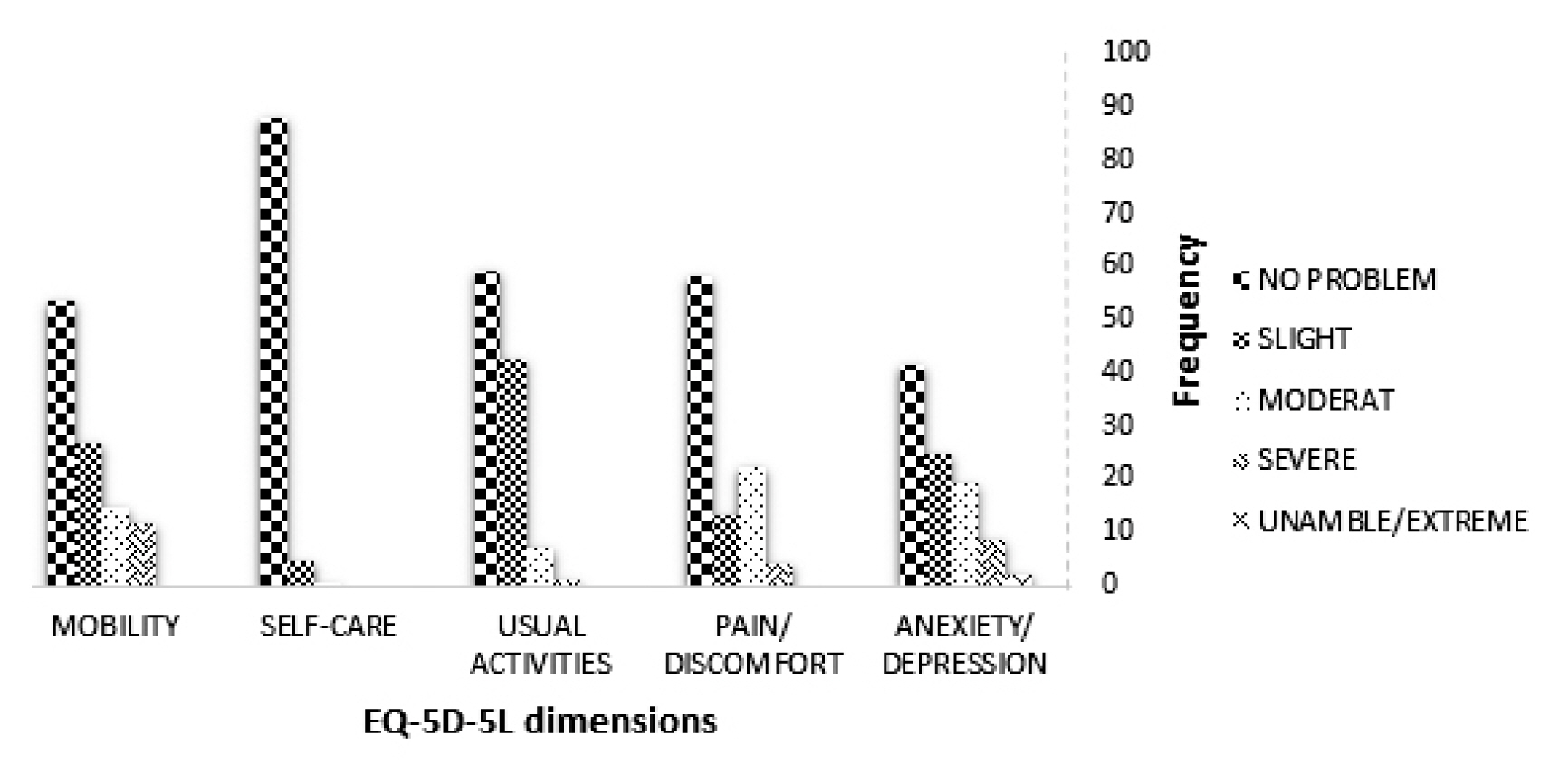
1. Distribution of the EQ-5D-5L dimensions
The distribution of HRQoL problems reported by patients for each of the EQ-5D-5L dimensions is shown in Figure 1. The percentage of patients reporting no problems (healthy state) for mobility, self-care, usual activities, pain/discomfort, and anxiety/depression was 53.34%, 87.75%, 58.97%, 57.97%, and 41.26%, respectively. Patients only reported unable to/extreme problems for the anxiety dimension.
2. Univariate analyses
The mean EQ-5D-5L index values for patients were 0.6125 ± 0.006. The results of univariate analysis for the association between socio-demographic factors and the EQ-5D-5L index values are presented in Table 1. The difference between the mean EQ-5D-5L index values was significant for gender (p = 0.002), age (p = 0.005), education status (p < 0.001), employment status (p < 0.001), and workplace status (p = 0.002). Univariate analysis also showed that among clinical factors, the difference between the mean EQ-5D-5L index values was significant if the patient had diabetes (p < 0.001), or heart failure (p = 0.002) and/or was admitted to hospital (p < 0.001).
3. Regression analyses
The factors associated with HRQoL scores using the BetaM model showed that female gender, older age, higher education level, being unemployed, ICU admission, and having diabetes had significant negative effects on the EQ-5D-5L index values (p < 0.05). The marginal effect analysis showed that the largest marginal effect was caused by age among the demographic variables (0.44), and having diabetes (0.31) among the clinical demographics (Table 3).
Discussion
This study evaluated HRQoL of COVID-19 patients using the EQ-5D-5L questionnaire and assessed the effects of socio-demographic and clinical factors on HRQoL. The results of this study provided important insights of the HRQoL based on the characteristics of hospitalized COVID-19 patients that can be used in the management of the disease. The mean EQ-5D-5L score for the patients was 0.6125.
A study conducted on people (n = 4,029) with suspected COVID-19 symptoms (S-COVID-19-S) visiting outpatient departments and health centers in Vietnam, in 2020 reported a mean score of 0.621 for the assessment of HRQoL [8]. The overall EQ-5D-5L score for COVID patients (0.612) in this study was lower than Asian patients suffering from diabetes (0.84) [21], type 2 diabetes (0.84) [22], cardiovascular diseases (0.84) [23], acute coronary syndrome (0.75) [24] human immunodeficiency virus (0.8) [25], skin diseases (0.73) [26], and respiratory diseases (0.66) [27], but higher than frail elderly (0.58) [28] and elderly patients after a fall injury (0.46) [29].
The percentage of individuals reporting problems affecting their HRQoL in each EQ-5D-5L dimension showed the most common problem was anxiety. Similar results also were reported by Nguyen et al [8]. They showed that the odds ratio of depression for people with S-COVID-19-S was higher than that of the people without S-COVID-19-S (3.69 vs. 1) [8].
Among the demographic factors, univariate analyses showed that the mean EQ-5D-5L scores were significantly different depending on gender, age, education level, employment status, and workplace of the patients. The findings were similar to the findings reported in the study by Nguyen et al [8]. They reported the difference between mean HRQoL scores for people with S-COVID-19-S was significant depending on age, gender, marital status, education level, occupation status, ability to pay for medication, social status, comorbidity, and physical activity [8].
The older age groups of patients had lower scores of HRQoL compared with the younger patients. This may reflect the fact that COVID-19 impacts more on older patients. Sommer et al [30] reported that severe cases of COVID-19 (involving ICU admission) skewed towards patients who were > 60 years old. This current study revealed that women had lower scores for HRQoL than men. This finding may be due to a difference in the level of physical activity between men and women in developing countries, as women have a lower level of physical activity than men [31]. Another reason may be due to the fact that women are more worried about disease and may have less ability to cope. It was also observed that the difference between mean HRQoL scores in patients with different levels of education was significant. Lower scores of HRQoL were observed in patients with a higher level of education a greater level of awareness and concern of COVID-19 and its impact on life. Nguyen et al [8] observed that people with a college/university education had a higher prevalence of depression during the pandemic that created a burden of stress which further affected their HRQoL. The present study also showed that employed patients had higher scores of HRQoL. This could be due to the fact that the employed patients had not lost their income; therefore, they had more opportunity to have better healthcare [32]. A significant difference between HRQoL mean scores was also observed in workplaces of the patients. The patients who worked in crowded environments such as factories, shopping malls, and banks, had lower scores of HRQoL compared with people who worked in an uncrowded environment. The majority of the patients in crowded environments reported high anxiety of re-infection. We asked the patients to state their anxiety/depression regarding re-infection using the 5-Likert scale (no anxiety, slight anxiety, some anxiety, a lot of anxiety, or very anxious/depressed). In contrast to the results of this study, executives in Chongqing, China (n = 122) were reported to have a lower prevalence of depression and anxiety when they returned to work during COVID-19 pandemic [33]. There is an urgency to redesign training programs and communication activities for a more effective dissemination of information related to the COVID-19 [34].
Among clinical factors, the difference between mean scores of HRQoL was significant for ICU admission, having diabetes, and heart failure in this study. The mean HRQoL scores were different between the patients who had been admitted to hospital wards. The patients admitted to the ICU for COVID-19 treatment had lower scores of HRQoL than those admitted to a hospital wards, probably because ICU patients experienced more severe problems related to COVID-19. The mean scores of HRQoL were lower in the patients with diabetes than those without diabetes. This is because the disease was more severe in the patients with diabetes and it exacerbates their diabetes symptoms [35]. These results are consistent with the findings of a recent study conducted in critical care COVID-19 patients in the US. The study reported that COVID-19 in cases severe enough to require ICU admission, skewed the patient population towards patients with medical comorbidities, such as hypertension, diabetes mellitus, or cardiovascular diseases [30]. Furthermore, the patients with heart failure had lower HRQoL scores compared with those without heart failure.
The regression analysis showed that amongst demographic factors, age had the most marginal effect therefore, it has the most impact on HRQoL. It can be explained by the direct relationship between aging and increasing incidence of problems in patients. Among the clinical factors, having diabetes had the most marginal effect on HRQoL. Diabetes has been reported as a comorbidity of COVID-19 [35].
One limitation of the study was that the design was not cross-sectional, which did not allow the determination of the exact effects of patients’ socio-demographic and clinical factors on HRQoL. Further research is required using a longitudinal study to understand how these factors may affect the HRQoL. Another limitation is the use of crosswalk to calculate the Iranian EQ-5D-5L value set. The value set based on crosswalk is less reliable than the one obtained directly from the general public-preference. However, crosswalk is currently the only available technique to generate the EQ-5D-5L value set for countries that do not have the EQ-5D-5L value set based on their own context.
Conclusion
The mean score of HRQoL for the patients was 0.6125 in this study. Identifying strategies to improve the HRQoL in patients, especially in aging and diabetic patients, is therefore of particular importance. This study showed that gender, among demographic factors, and diabetes, among clinical factors, had the most marginal effect on the dimensions of EQ-5D-5L.
Acknowledgments
We would like to thank all patients who agreed to participate in this study.
Notes
Conflicts of Interest
The authors have no conflicts of interest to declare.