Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 12(4); 2021 > Article
-
Original Article
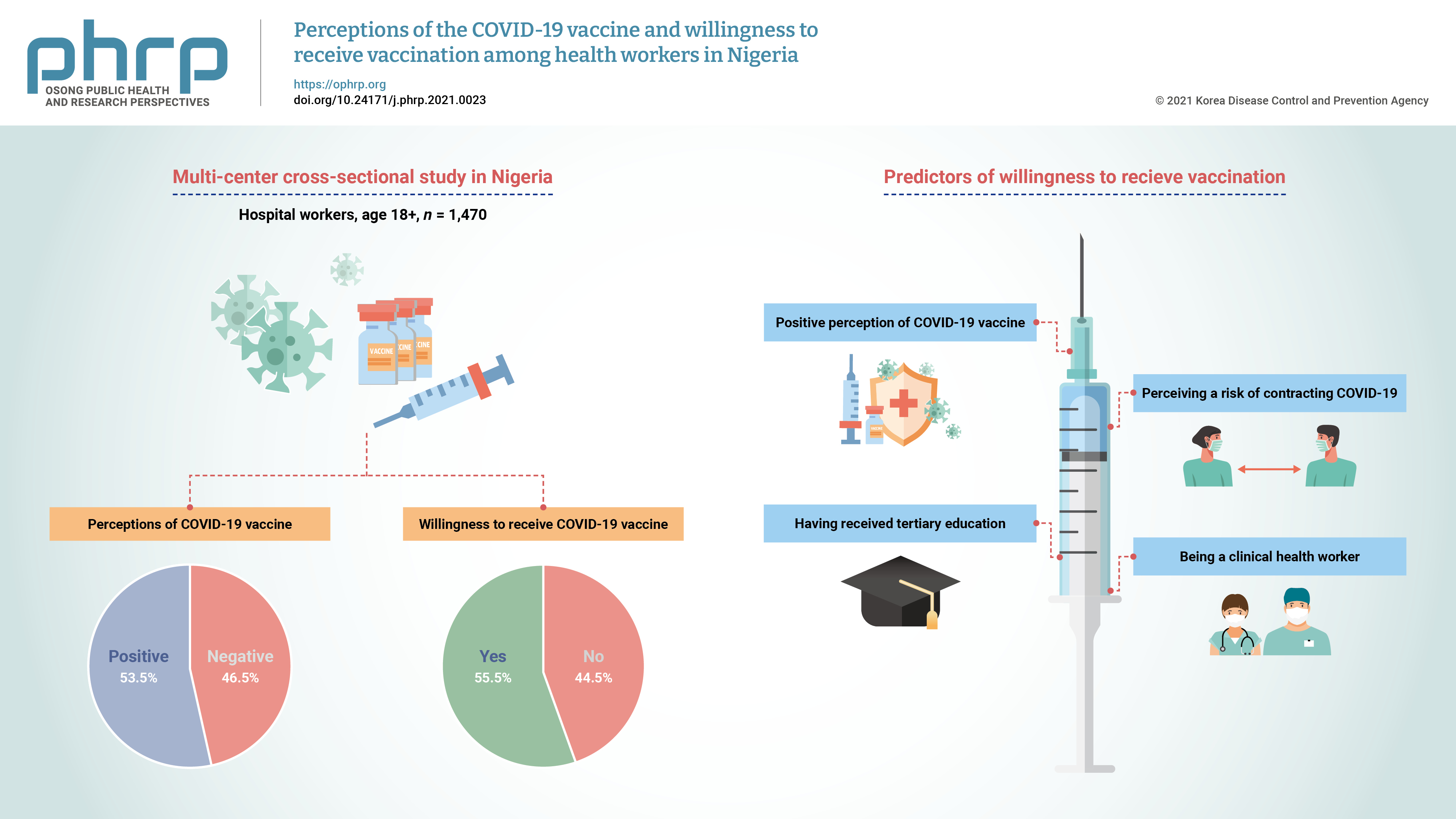
Perceptions of the COVID-19 vaccine and willingness to receive vaccination among health workers in Nigeria -
Oluseyi Ademola Adejumo1
 , Olorunfemi Akinbode Ogundele2
, Olorunfemi Akinbode Ogundele2 , Cynthia Roli Madubuko3
, Cynthia Roli Madubuko3 , Rosena Olubanke Oluwafemi4
, Rosena Olubanke Oluwafemi4 , Ogochukwu Chinedum Okoye5
, Ogochukwu Chinedum Okoye5 , Kenechukwu Chukwuemeka Okonkwo1
, Kenechukwu Chukwuemeka Okonkwo1 , Sunday Samson Owolade1
, Sunday Samson Owolade1 , Oladimeji Adedeji Junaid1
, Oladimeji Adedeji Junaid1 , Olutoyin Morenike Lawal1
, Olutoyin Morenike Lawal1 , Adenike Christianah Enikuomehin1
, Adenike Christianah Enikuomehin1 , Maureen Iru Ntaji6
, Maureen Iru Ntaji6 , Aisha Sokunbi3
, Aisha Sokunbi3 , Aina Omodele Timothy3
, Aina Omodele Timothy3 , Olatunji Sunday Abolarin1
, Olatunji Sunday Abolarin1 , Emmanuel Olalekan Ali1
, Emmanuel Olalekan Ali1 , John Oghenevwirhe Ohaju-Obodo5
, John Oghenevwirhe Ohaju-Obodo5
-
Osong Public Health and Research Perspectives 2021;12(4):236-243.
DOI: https://doi.org/10.24171/j.phrp.2021.0023
Published online: July 19, 2021
1Department of Internal Medicine, University of Medical Sciences, Ondo City, Nigeria
2Department of Community Medicine, University of Medical Sciences, Ondo City, Nigeria
3Department of Internal Medicine, University of Benin Teaching Hospital, Benin City, Nigeria
4Department of Paediatrics, University of Medical Sciences, Ondo City, Nigeria
5Department of Internal Medicine, Delta State University, Abraka, Nigeria
6Department of Community Medicine, Delta State University, Abraka, Nigeria
- Corresponding author: Olorunfemi Akinbode Ogundele Department of Community Medicine, University of Medical Sciences, Laje Road, PMB 536 Ondo City, Ondo State, Nigeria E-mail: femidele@gmail.com
• Received: January 22, 2021 • Revised: June 7, 2021 • Accepted: June 8, 2021
© 2021 Korea Disease Control and Prevention Agency
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Figure & Data
References
Citations
Citations to this article as recorded by 

- Nigerians’ attitudes and perceptions towards vaccine acceptance during and after the COVID-19 pandemic
Jonas Lotanna Ibekwe, Victor Oluwafemi Femi-Lawal, Jolly Akor Thomas, Faith Uzoamaka Okei, Moses Ojomakpenen Ojile, Oluwatobiloba Oladipupo Akingbulugbe
Journal of Medicine, Surgery, and Public Health.2024; 2: 100066. CrossRef - Knowledge, attitudes, and factors determining the willingness for COVID-19 vaccination among students in Bangladesh: An online-based cross-sectional study
Ashis Talukder, Soheli Sharmin, Chuton Deb Nath, Iqramul Haq, Md. Ismail Hossain, Md. Jakaria Habib, Sabiha Shirin Sara
Journal of Public Health.2024; 32(4): 663. CrossRef - Healthcare professionals’ perception and COVID-19 vaccination attitudes in North-Western Ghana: A multi-center analysis
Augustine Ngmenemandel Balegha, Suburu Abdul-Aziz, Louis Mornah, Pracheth Raghuveer
PLOS ONE.2024; 19(2): e0298810. CrossRef - Behavioral Insights from Vaccine Adoption in Nigeria: Cross-Sectional Survey Findings
Sohail Agha, Ifeanyi Nsofor, Drew Bernard, Sarah Francis, Nandan Rao
Interactive Journal of Medical Research.2024; 13: e47817. CrossRef - COVID-19 vaccine hesitancy in Latin America and Africa: a scoping review
Bruna Aparecida Gonçalves, Camila Carvalho de Souza Amorim Matos, Jonathan Vicente dos Santos Ferreira, Renata Fortes Itagyba, Vinicius Rocha Moço, Marcia Thereza Couto
Cadernos de Saúde Pública.2023;[Epub] CrossRef - Suspecting the Figures: What Church Leaders Think About Government’s Commitment to Combating COVID-19 in Nigeria
Uchechukwu M. Agbo, George C. Nche
Journal of Asian and African Studies.2023; 58(5): 725. CrossRef - Access to COVID-19 vaccines and testing in Africa: the importance of COVAX - Nigeria as a case study
Rafaella Fortini Queiroz Grenfell, Oyetunde Timothy Oyeyemi
Pathogens and Global Health.2023; 117(2): 152. CrossRef - COVID-19 vaccine acceptance prediction: The roles of students’ attitude towards science and mathematics and knowledge of COVID-19 pandemic
Sunday Ogbu, Ogochukwu Ebere Emenike, Amaka Loretta Nwankwo
Electronic Journal of Medical and Educational Tech.2023; 16(2): em2304. CrossRef - Factors associated with COVID-19 vaccine hesitancy among healthcare workers in Cameroon and Nigeria: a web-based cross-sectional study
Jerry Brown Aseneh, Valirie Ndip Agbor, Benjamin Momo Kadia, Elvis Anyaehiechukwu Okolie, Chinelo Janefrances Ofomata, Christie Linonge Etombi, Domin Sone M Ekaney, Yvonne Walburga Joko Fru
International Health.2023; 15(6): 702. CrossRef - Willingness to COVID-19 vaccination: Empirical evidence from EU
Imran Ur Rahman, Arslan Austin, Naveed Nelson
Heliyon.2023; 9(5): e15776. CrossRef - Radiographers’ knowledge, attitude and adherence to standard COVID-19 precautions and the policy implications: a national cross-sectional study in Nigeria
Charles Ikechukwu Ezema, Okechukwu Felix Erondu, Ogochukwu Kelechi Onyeso, Chiedozie James Alumona, Andrew Wueseter Ijever, Charity Ndidiamaka Amarachukwu, Amaeze Augustine Amaeze
Annals of Medicine.2023;[Epub] CrossRef - Declining trends in vaccine confidence across sub-Saharan Africa: A large-scale cross-sectional modeling study
A. de Figueiredo, E. Temfack, R. Tajudeen, H. J. Larson
Human Vaccines & Immunotherapeutics.2023;[Epub] CrossRef - Knowledge and acceptance of COVID-19 vaccine among healthcare workers in Enugu metropolis, Enugu state, Nigeria
Kelechi U. Imediegwu, Jude C. Abor, Chiamaka Q. Onyebuchukwu, Hilary I. Ugwu, Ogechi I. Ugwu, Udo Ego Anyaehie, Oluchi A. Onyia
Frontiers in Public Health.2023;[Epub] CrossRef - COVID-19 vaccination acceptance (uptake, hesitancy, intention to receive and timeliness of the intention to receive) and the determinants among health workers in Ebonyi state, Nigeria: an analytical cross-sectional study
Ugwu I Omale, Onyinyechukwu U Oka, Chidinma I Amuzie, Victor U Uduma, Azuka S Adeke, Cordis O Ikegwuonu, Glory E Nkwo, Ugochi I A Nwali, Osarhiemen Iyare, Richard L Ewah, Olaedo O Nnachi, Okechukwu O Ukpabi, Ifeyinwa M Okeke
BMJ Open.2023; 13(7): e068668. CrossRef - Hesitação vacinal contra a COVID-19 na América Latina e África: uma revisão de escopo
Bruna Aparecida Gonçalves, Camila Carvalho de Souza Amorim Matos, Jonathan Vicente dos Santos Ferreira, Renata Fortes Itagyba, Vinicius Rocha Moço, Marcia Thereza Couto
Cadernos de Saúde Pública.2023;[Epub] CrossRef - The Social Ecological Model: A Framework for Understanding COVID-19 Vaccine Uptake among Healthcare Workers—A Scoping Review
Damian Naidoo, Anna Meyer-Weitz, Kaymarlin Govender
Vaccines.2023; 11(9): 1491. CrossRef - Health service factors affecting the COVID-19 vaccination campaign in a Ghanaian metropolis: A qualitative exploratory study
Susanna Aba Aba Abraham, John Oti Amoah, Dorcas Frempomaa Agyare, Deogratias Kaheeru Sekimpi, Diana Bosomtwe-Duker, Andrews Adjei Druye, Gifty Osei Berchie, Dorcas Obiri-Yeboah
BMJ Open.2023; 13(12): e076184. CrossRef - ‘Why Should I Take the COVID-19 Vaccine after Recovering from the Disease?’ A Mixed-methods Study of Correlates of COVID-19 Vaccine Acceptability among Health Workers in Northern Nigeria
Zubairu Iliyasu, Muhammad R. Garba, Auwalu U. Gajida, Taiwo G. Amole, Amina A. Umar, Hadiza M. Abdullahi, Aminatu A. Kwaku, Hamisu M. Salihu, Muktar H. Aliyu
Pathogens and Global Health.2022; 116(4): 254. CrossRef - A Global Map of COVID-19 Vaccine Acceptance Rates per Country: An Updated Concise Narrative Review
Malik Sallam, Mariam Al-Sanafi, Mohammed Sallam
Journal of Multidisciplinary Healthcare.2022; Volume 15: 21. CrossRef - Knowledge, Attitudes, and Perception towards COVID-19 Vaccination among the Adult Population: A Cross-Sectional Study in Turkey
Meliha Cagla Sonmezer, Taha Koray Sahin, Enes Erul, Furkan Sacit Ceylan, Muhammed Yusuf Hamurcu, Nihal Morova, Ipek Rudvan Al, Serhat Unal
Vaccines.2022; 10(2): 278. CrossRef - Factors influencing COVID-19 vaccine uptake among adults in Nigeria
Halimat Adedeji-Adenola, Olubusola A. Olugbake, Shakirat A. Adeosun, Ismaeel Yunusa
PLOS ONE.2022; 17(2): e0264371. CrossRef - Perception and Prevention Practices Relating to Covid 19 Infection Among Elderly in Ogun State, Nigeria
Adenitire G., Agbede C.O.
International Journal of Public Health and Pharmac.2022; 2(1): 29. CrossRef - Predicting nursing students' intention to attend face‐to‐face classes on school reopening: A theory of planned behavior application
Ryan Michael F. Oducado, Jerome V. Cleofas, Gil P. Soriano
Nursing Forum.2022; 57(5): 733. CrossRef - COVID-19 vaccination in Nigeria: A rapid review of vaccine acceptance rate and the associated factors
Oluwatosin Olu-Abiodun, Olumide Abiodun, Ngozi Okafor, Nusirat Elelu
PLOS ONE.2022; 17(5): e0267691. CrossRef - COVID-19 vaccine acceptance among health care workers in Africa: A systematic review and meta-analysis
Martin Ackah, Louise Ameyaw, Mohammed Gazali Salifu, Delali Pearl Afi Asubonteng, Cynthia Osei Yeboah, Eugene Narkotey Annor, Eunice Abena Kwartemaa Ankapong, Hosea Boakye, Muhammad Shahzad Aslam
PLOS ONE.2022; 17(5): e0268711. CrossRef - A national survey of COVID-19 vaccine acceptance in Nigeria
Ahmad Ibrahim Al-Mustapha, Ochulor Okechukwu, Ademola Olayinka, Oyeniyi Rasheed Muhammed, Muftau Oyewo, Samuel A. Owoicho, Ahmed Tijani Abubakar, Abdulsalam Olabisi, Aliyu Jibril, Simon Ereh, Oluwatosin Enoch Fakayode, Oluwaseun Adeolu Ogundijo, Nusirat E
Vaccine.2022; 40(33): 4726. CrossRef - COVID-19 vaccine hesitancy in Africa: a scoping review
Betty B. B. Ackah, Michael Woo, Lisa Stallwood, Zahra A. Fazal, Arnold Okpani, Ugochinyere Vivian Ukah, Prince A. Adu
Global Health Research and Policy.2022;[Epub] CrossRef - COVID-19 Vaccine Acceptance and Associated Factors Among College Students in Dessie City, Northeastern Ethiopia
Gete Berihun, Zebader Walle, Daniel Teshome, Leykun Berhanu, Mohammed Derso
Journal of Multidisciplinary Healthcare.2022; Volume 15: 1735. CrossRef - Career Aspiration Fulfillment and COVID-19 Vaccination Intention among Nigerian Youth: An Instrumental Variable Approach
Abayomi Samuel Oyekale
International Journal of Environmental Research an.2022; 19(16): 9813. CrossRef - COVID-19 Vaccine Attitude and Its Predictors Among People Living With Chronic Health Conditions in Ibadan, Nigeria
Lucia Yetunde Ojewale, Rotimi Felix Afolabi, Adesola Ogunniyi
International Journal of Public Health.2022;[Epub] CrossRef - Associations between COVID-19 vaccine hesitancy and the experience of violence among women and girls living with and at risk of HIV in Nigeria
Morenike Oluwatoyin Folayan, Olujide Arije, Amaka Enemo, Aaron Sunday, Amira Muhammad, Hasiya Yunusa Nyako, Rilwan Mohammed Abdullah, Henry Okiwu, Erik Lamontagne
African Journal of AIDS Research.2022; 21(4): 306. CrossRef - Willingness to receive COVID-19 vaccine: A survey among medical radiation workers in Nigeria
Grace Ben Inah, Samuel Archibong Efanga, Ekaete Vincent Ukpong, Christiana Ifeyinwa Obiora
Calabar Journal of Health Sciences.2022; 6: 80. CrossRef - Acceptance of COVID-19 vaccine among healthcare workers in Africa, systematic review and meta-analysis
Zerihun Figa, Tesfaye Temesgen, Addisu Getnet Zemeskel, Moges Ganta, Asrat Alemu, Mesfin Abebe, Zemachu Ashuro
Public Health in Practice.2022; 4: 100343. CrossRef - Perception and willingness to accept COVID-19 Vaccines: A cross-sectional survey of the general population of Sokoto State, Nigeria
Oche Mansur Oche, Habibullah Adamu, Musa Yahaya, Hudu Garba Illo, Abdulaziz Mohammad Danmadami, Adamu Ijapa, Asmau Mohammad Wali, Hamza Yusuf, Hafsat Muhammad, Abba Aji, Harapan Harapan
PLOS ONE.2022; 17(12): e0278332. CrossRef - COVID-19 vaccination acceptance among community members and health workers in Ebonyi state, Nigeria: study protocol for a concurrent-independent mixed method analyses of intention to receive, timeliness of the intention to receive, uptake and hesitancy to
Ugwu I Omale, Osarhiemen Iyare, Richard L Ewah, Chidinma I Amuzie, Onyinyechukwu U Oka, Victor U Uduma, Azuka S Adeke, Cordis O Ikegwuonu, Olaedo O Nnachi, Okechukwu O Ukpabi, Ifeyinwa M Okeke, Glory E Nkwo, Ugochi IA Nwali
BMJ Open.2022; 12(12): e061732. CrossRef - Drivers of COVID-19 Vaccine Uptake amongst Healthcare Workers (HCWs) in Nigeria
Sohail Agha, Adaobi Chine, Mathias Lalika, Samikshya Pandey, Aparna Seth, Alison Wiyeh, Alyssa Seng, Nandan Rao, Akhtar Badshah
Vaccines.2021; 9(10): 1162. CrossRef




 PubReader
PubReader ePub Link
ePub Link Cite
Cite