Waist Circumference and Spirometric Measurements in Chronic Obstructive Pulmonary Disease
Article information
Abstract
Objectives
The aim of this study was to evaluate whether the waist circumference of patients with chronic obstructive pulmonary disease (COPD), had an impact on lung function.
Methods
There were 180 patients with COPD recruited into this prospective cross-sectional study. The age, weight, body mass index and waist circumference (WC) were measured. Spirometry parameters including forced vital capacity (FVC), and forced expiratory volume in the first second (FEV1), were measured and FEV1/FVC calculated.
Results
The mean FEV1/FVC in both normal weight and overweight patients, did not statistically significantly correlate with WC. The COPD assessment test, positively correlated with WC ( p = 0.031). A positive correlation with body mass index ( p < 0.001), smoking ( p = 0.027), and global initiative for chronic obstructive lung disease score ( p = 0.009), were observed to positively associate with WC. WC, age, C-reactive protein, duration of disease, and gender (male), were observed to be statistically significant risk factors for the severity of COPD.
Conclusion
WC was not observed to impact upon lung function in this study but it was a predictive factor for COPD severity in patients.
Introduction
Chronic obstructive pulmonary disease (COPD) is a chronic lung disease that is preventable and treatable [1]. COPD is a major cause of disability, reduced quality of life, and mortality throughout the world, and is the 4th most common cause of death in the United States by 2020, accounting for more than 120,000 deaths [2]. COPD is known not only as a disease of the lungs, but it also affects many organs and tissues [3], and patients typically have 1 or more components of metabolic syndrome [4–9].
Abdominal obesity and particularly visceral obesity is the key feature of metabolic syndrome that is also associated with many chronic diseases, particularly cardiovascular, and respiratory diseases [10]. In order to predict the severity of illness and the functional limitations of lungs, specific anthropometric measurements are very valuable because of ease, availability, and cost-effectiveness [11]. Likewise, body mass index (BMI), waist circumference (WC), and waist-to-hip ratio can be used to estimate the abdominal visceral fat measurement [12].
Generally, lack of physical activity is one of the highest causes of visceral fat accumulation in patients with COPD [13]. The visceral fat tissues are identified as the source of pro-inflammatory cytokines such as Interleukin-6 that can induce
C-reactive protein (CRP) synthesis in hepatocytes. Subsequently, accumulation of visceral fat leads to high levels of Interleukin-6 and tumor necrosis factor alpha, and low levels of adiponectin (an anti-inflammatory cytokine that reduces the risk of heart disease) [14]. Furthermore, systemic inflammation is associated with the pathogenesis of metabolic syndrome and COPD [5] and metabolic syndrome is prevalent in COPD patients [15, 16].
WC assessment is a good indicator of individuals with a health risk due to the accumulation of extra fat around the internal organs, and with increasing age, men tend to gain fat around the waist, whilst women accumulate fat in buttocks, gluteal regions, and around the thighs and hips. As we know a waist circumference of 102 centimeters (40 inches) or more in men, or 88 centimeters (35 inches) or more in women, is associated with health problems such as type 2 diabetes, heart disease and high blood pressure. WC measures abdominal fat but it can also give information about distribution of body fat. WC may affect mechanical ventilation of the lungs that leads to a restriction of movement of the diaphragm [16]. Measurements of obesity may indicate the progression and severity of COPD, and WC may be a predictive factor of visceral fat accumulation which plays a role in the inflammatory process. The objective of this study was to investigate the impact of WC on the severity of the obstruction of airways, forced expiratory volume in the first second (FEV1)/forced vital capacity (FVC) and FEV1 by spirometry analysis.
Materials and Methods
1. Ethics approval and patient consent
Research ethics were approved for this study on 2015-10-06, (IR.GUMS.REC.1394.272). This prospective cross-sectional study was carried out on 180 patients with COPD who were admitted to Razi Hospital, Rasht, Iran, between 2014 and 2015. COPD was confirmed in patients according to the global initiative for chronic obstructive lung disease (GOLD) score, and the patients were enrolled consecutively after giving written informed consent.
2. Inclusion/exclusion criteria
Patients who were included in the study had been diagnosed with COPD. Patients excluded in the study had cystic fibrosis, tuberculosis, bronchial asthma, bronchogenic carcinoma, external lung tissue disease, pulmonary surgery, cardiovascular disease, diabetes mellitus, uremia, or sarcoidosis. Patients who used azithromycin, long-term, and patients who were prescribed antiepileptic drugs were also excluded.
3. Demographic data
A checklist including details of gender, age, hypertension, diabetes, cigarette smoking, high-density lipoprotein (HDL), cholesterol, triglyceride, fasting blood sugar (FBS), and CRP test was recorded. The height was measured by stadiometer and weight of patients was measured by scales. BMI was calculated by dividing weight by the square of height (kg/m2). The WC was measured at the lower edge of the rib and the iliac spine, and the hip circumference was determined at widest point above the buttocks, using a standard tape measure.
4. Lung volume measurements
Lung volume measurements were conducted using a spiroanalyser (MIR Spirolab spirometer, Italy), in a sitting position, with help from a nurse at the Razi hospital. The patients performed maximum and appropriate deep breaths. The observations from the spirometry examination were expressed as forced vital capacity (FVC), FEV1 and FEV1/FVC was calculated. The grading of COPD was carried out according to the latest report of GOLD criteria. The disease quality control questionnaire was completed based on COPD assessment and the COPD assessment test (CAT) score.
5. CAT Score
CAT score is a complementary tool used alongside methods such as FEV1 to assesses COPD [17]. The CAT score results from a short and simple 8-item questionnaire that the patient completes. This test is commonly used in clinical practice to determine the health status of patients with COPD [18].
6. Statistics analysis
Variables were analyzed using a normality test. Parametric tests such as the “T test” were used to compare WC and severity of COPD (based on GOLD score). Otherwise, the non-parametric “Mann Whitney U test” was applied. Estimating the normal distribution of variables was analyzed using “Pearson’s correlation coefficient test” to study the relationship between WC and the spirometry data. Otherwise, “Spearman’s coefficient test” was applied. The Scatter plot was drawn to demonstrate the dependence distribution. The multiple linear regression method was utilized to determine the predicted spirometry values based on WC. An alpha of 0.05 was applied as the cut off for statistical significance (p < 0.05).
Results
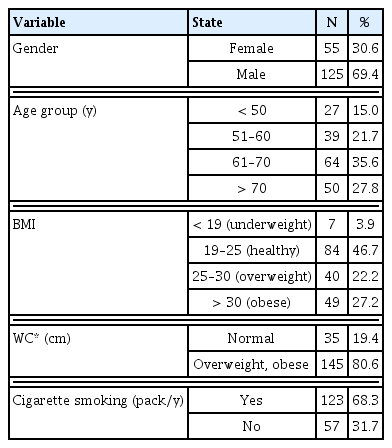
There were 180 patients with COPD included in this study, of which 69.4% were males who had a mean age of 35.6 years (61–70 years; Table 1). There were 46.7% of patients who had a healthy BMI (kg/m2). It was observed that 49.4% of patients had a overweight WC. As shown in Table 1, 68.3% of the patients were cigarette smokers (Table 1). The mean BMI of the patients was 34.5 ± 43.26 kg/m2. The average WC in women and men were 95.11 ± 94.1 cm and 46.10 ± 11.108 cm, respectively. The mean disease duration in COPD patients was 49.16 ± 2.27 months. The average consumption of cigarettes smoking was 24.7 ± 15.6 (Table 1). The mean CAT score in COPD patients was 94.7 ± 36.18. On the other hands, Figure 1 demonstrate relationships between BMI (A), consumption cigarette smoking (B), gold score (C), CAT score (D), and waist circumference of patients with COPD (Figure 1).
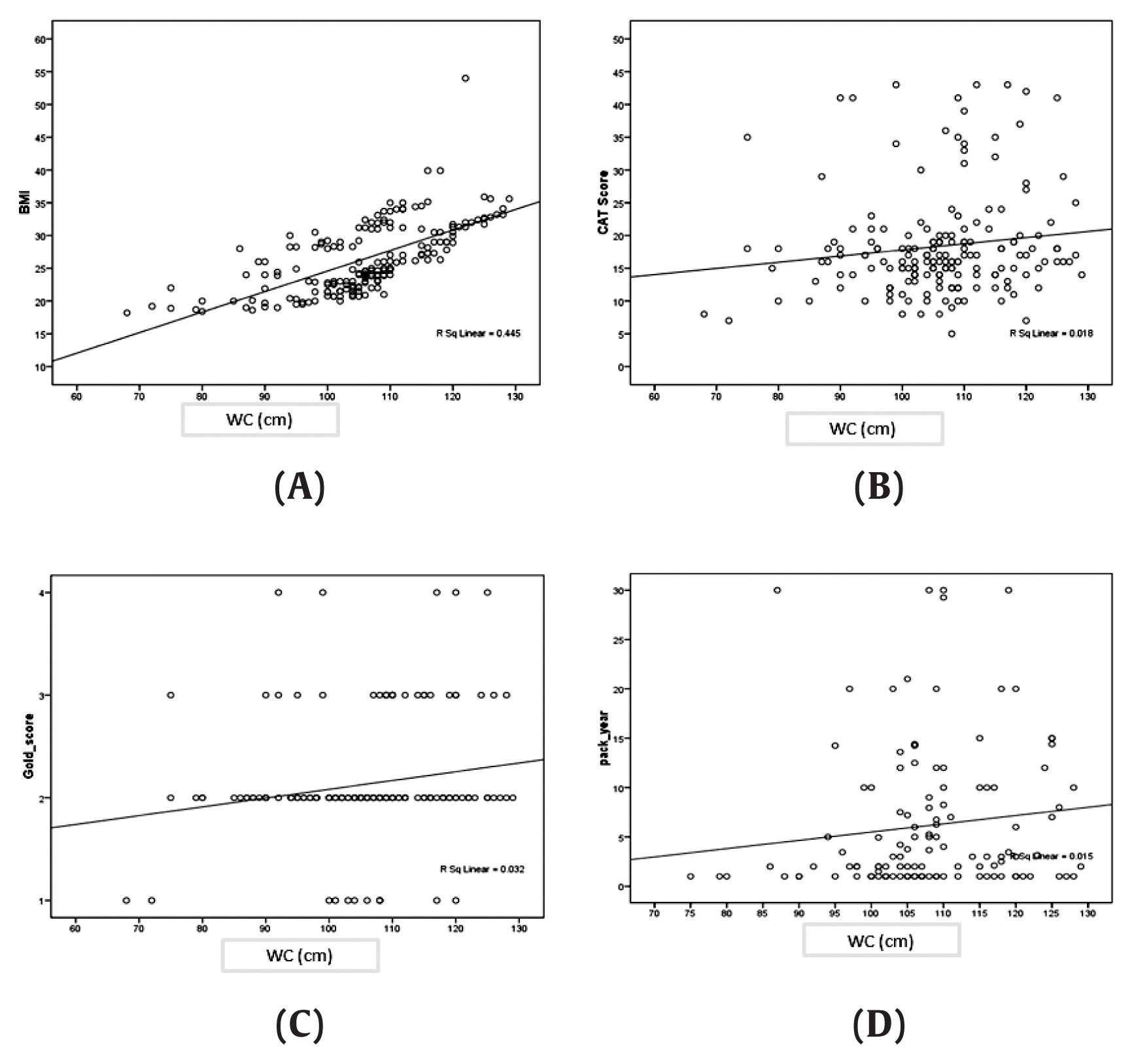
Distribution chart of BMI (A) cigarette smoking (B), gold score (C), CAT score (D), and WC of patients with COPD.
BMI = body mass index; CAT = COPD assessment test; COPD = chronic obstructive pulmonary disease; WC = waist circumference.
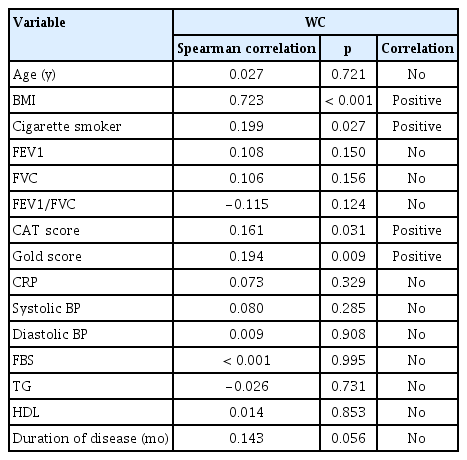
Positive correlations were observed between cigarette smoking, BMI, CAT scores, and GOLD scores, and WC in patients with COPD (Table 2). Predictive factors for the severity of COPD in patients with normal and overweight WC were assessed according to the GOLD scores. There is a significant difference between the mean of overweight WC and normal weight WC in the severity of patients with COPD based on GOLD score (p = 0.045; Table 3). This study showed that there is a significantly difference between WC and FEV1/FVC (p = 0.036; Table 3). We also showed significantly difference between WC and CAT score in patients with COPD (p = 0.045; Table 3). Ordinal logistic regression analysis of predictive factors for the severity of patients with COPD based on FVC (Table 4). Table 4 showed that there is a correlation between WC (p = 0.004), age (p = 0.027), duration of disease (p = 0.038), men gender (p < 0.001), and CRP (p < 0.001) with FVC as a predicting factor in severity COPD (Table 4).

Spirometric parameters and severity of patients with COPD in normal and overweight waist circumference.
Discussion
In the current study, pulmonary function and WC were investigated in 180 COPD patients. Clinical studies have showed that COPD patients typically have 1 or more components of metabolic syndrome. Abdominal obesity and particularly visceral obesity, have been shown to be key features of metabolic syndrome, which is also related to chronic diseases [10]. A correlation between coronary artery disease and abdominal obesity has been observed [10]. It has also been reported that in those people who smoke cigarettes and who have a high WC, there is an increased risk of developing heart disease [19]. Furthermore, several studies have indicated that WC, but not BMI, was associated with chronic heart failure, and that abdominal fat tissue was a stronger risk factor for obesity [19, 20]. It was also observed that the ratio of WC to FEV1/FVC might potentially have a higher predictive value [19, 20]. Gibson [20] and Chen et al [21] showed that there is a significant difference between obesity and coronary artery disease score in women and men.
A previous study of COPD [17] reported that physical inactivity may lead to dyspnea, which may explain why many patients lead an inactive and sedentary life. In addition, excess fat tissue may act as an additional mediator of inflammation [22, 23]. Other studies have reported that visceral fat, in the absence of obesity (especially in the advanced stages of the disease), was significantly higher in patients with COPD [22]. Furutate et al [17] showed that patients with COPD suffer from muscular atrophy and excessive accumulation of visceral fat, especially in the severe stages of COPD and emphysema. In advanced stages of COPD when energy consumption is high, it was reported that muscle mass was reduced [20]. Reduced physical activity (due to dyspnea) and capacity to exercise, inadequate dietary intake, or systemic inflammation leads to decreased muscle mass. Physical inactivity results in excessive accumulation of visceral fat, especially in more advanced stages of COPD, and severe emphysema. Visceral obesity was reported to be typically associated with dyslipidemia leading to systemic inflammation [20]. Excessive visceral fat was also another source of systemic inflammation in COPD patients. Reducing lung function in the COPD patients, lead to hypoxemia.
Patients with COPD may be more susceptible to hypoxemia, because systemic inflammation may be associated with systemic oxygen deficiency [23]. In the current study, the WC of patients with COPD showed a significant relationship between the FVC and FEV1 (p = 0.036) (Table 4). However, WC was not associated with FEV1/FVC. In fact, when WC increased by 1 cm, the values of FVC, FEV1 decreased by 13 mL and 11 mL, respectively (Figure 1). In this current study BMI, cigarette smoking, CAT score and GOLD score, had a positive correlation with WC in patients with COPD. Likewise, increasing BMI, cigarette smoking, CAT score, and GOLD score, led to increased WC. Finally, the study showed that poor lung function would be associated with higher levels of abdominal fat (WC) in COPD patients (Figure 1). The limitations of this study were the small sample size, and low power to detect an effect of WC on lung function in COPD patients.
Conclusion
In the current study, positive correlations were detected between the WC and BMI, cigarette smoking, CAT score, and GOLD score. Meanwhile, the predictive factors for COPD severity were WC, age, CRP, duration of the disease, and being male. WC, which is an easily measured parameter, can be used to estimate pulmonary function rate in patients with COPD.
Notes
Conflicts of Interest
The authors declare that they have no competing interests.