The Effect of a Complex Intervention Program for Unilateral Neglect in Patients with Acute-Phase Stroke: A Randomized Controlled Trial
Article information
Abstract
Objectives
The purpose of this study was to examine the combined effects of Prism Adaptation (PA) plus functional electrical stimulation (FES) on stroke patients with unilateral neglect, and suggest a new intervention method for acute-phase stroke patients.
Methods
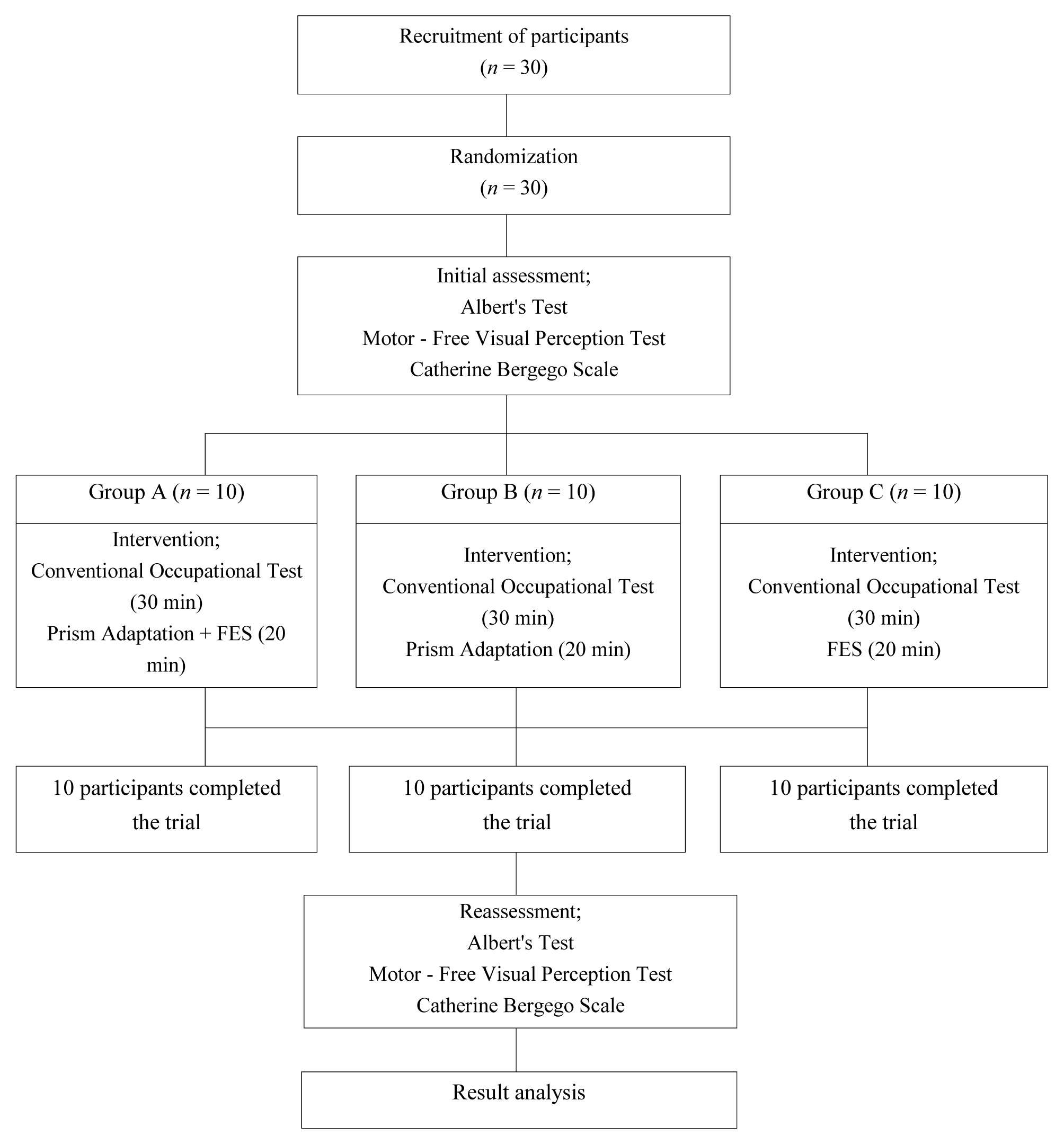
There were 30 patients included in this study from April to October 2016 that had unilateral neglect whilst hospitalized following a stroke (diagnosed by a professional). The participants, who were patients receiving occupational therapy, understood the purpose of the study and agreed to participate. The patients were randomly divided into 3 groups: PA plus FES group (Group A), PA group (Group B), and FES group (Group C). Treatments lasted for 50 minutes per day, 5 times per week, for 3 weeks in total. Reevaluation was conducted after 3 weeks of intervention.
Results
All 3 groups showed unilateral neglect reduction after the intervention, but PA plus FES (complex intervention method) was more effective than PA or FES alone [effect size: Motor-free Visual Perception Test (0.80), Albert test (0.98), CBS (0.92)].
Conclusion
The results of this study support further studies to examine complex intervention for the treatment of unilateral neglect.
Introduction
A stroke is an upper motor neurological condition in which blood flow to the brain is restricted due to cerebral vessel blockage or rupture resulting in brain cell death, that causes paralysis or paralysis on 1 side of the body. The patient’s symptoms and prognosis are determined by the mechanism, location, and range of the damage [1]. With advancements in medical technology, the death rate due to stroke has decreased. Only 30% of stroke patients recover completely, while the remaining 60%–70% experience lingering disabilities, making independent daily activities impossible [2].
Timing of intervention is one of the key factors of stroke rehabilitation [3]. Active treatment for acute-phase patients has a positive effect on post-stroke recovery [4]. The functional level of stroke patients improves most within 3 months of onset, then continues to gradually improve between 3 to 6 months. Langhorne and colleagues [5] said that starting rehabilitation during the acute-phase was essential. Active movement during the acute-phase is particularly important. This not only activates the brain and increases its potential, but also helps improve the quality of life [6]. A guideline published by the Australian National Stroke Foundation recommends that it is best to start rehabilitation as soon as possible within 6 months of stroke, and recommends receiving rehabilitation for 2–3 hours, 5 times per week. Therefore, according to these guidelines, it is important to have treatment access and receive rehabilitation during the acute-phase [7].
Unilateral neglect is of particular concern and refers to a variety of neuropsychological disorders in which responses to stimulation in the affected area are not perceived [8]. It can occur due to the perceptual and cognitive impairments of stroke patients, may interfere with the recovery of function after stroke and cause longer hospitalization time [9,10]. The probability of unilateral neglect varies from study to study, and the prevalence rate is estimated to be between 13–85% [11]. Unilateral neglect refers to having difficulty in reacting or paying attention to meaningful stimulation on the side opposite to the damaged brain, even if there is no abnormality in the motion or sensory system [12]. It is observed most often in patients with right cerebral hemisphere damage, resulting in adverse effects on their motor skills, particularly on their left side [13,14]. Some unilateral neglect patients cannot eat food placed on the left side of a dish, and in extreme cases show difficulty performing daily life activities such as leaving excessive space on the left when writing, and writing in the direction of right to left [15]. Therefore, Gail and Beverly [16] stated that using efficient strategies for the treatment of unilateral neglect in stroke patients is very important, and Kamath et al [17] stated that providing appropriate treatment early is very important given that the severity of unilateral neglect in acute-phase stroke patients is higher than that in recovery-phase stroke patients. Furthermore, Yun et al [18] said that early diagnosis of and appropriate treatment of unilateral neglect in acute-phase stroke patients can have positive effects on the reduction of unilateral neglect symptoms and functional recovery.
Unilateral neglect treatment has developed rapidly over the past few decades and have proven to be effective despite the aetiology [19]. Unilateral neglect treatments include Neck Vibration, Visual Scanning Training (VST), Eye Patch, Prism Adaptation (PA), Limb Activation Training, and Functional Electrical Stimulation (FES). Neck vibration allows spatial frame reformation around the neck by providing a unique sensory input that affects head and body posture [20]. VST is the most commonly used method among clinicians, and several studies have shown its effectiveness in reducing unilateral neglect. However, evidence that VST has long-lasting effects after treatment are lacking [21].
A half-opaque eye patch is a widely used method for improving the visuospatial attention and focus on the neglected side by artificially masking the view of the normal side [22]. PA is a method used to facilitate distortion of inherent sensation and vision, thereby improving the unilateral neglect by relocating the coordinate system [23,24]. Functional electrical stimulation therapy can be used for passive arm activation training in patients with unilateral neglect [16].
These treatment methods are usually used individually when treating unilateral neglect, but it was noted that there was a tendency for strong and long-lasting effect when treatment techniques were combined rather than applied alone [25]. Simultaneous application of left somatosensory system stimulation and VST was found to be more effective than VST alone, simultaneous application of neck vibration and PA was found to be more effective than PA alone, and simultaneous application of Transcutaneous Electrical Nerve Stimulation and optokinetic stimulation was found to be more effective than optokinetic stimulation alone [18,26,27].
Among the treatment techniques used in this study, PA is a self-administered active orthodontic treatment that does not rely on the assistance of an orthosis or a therapist because [28], and it is also the treatment used in a bottom-up approach, that modifies the underlying cause using devices that generally manipulate the stimuli in the patient’s environment, or enhance the perception on the neglected sides [29]. FES therapy is a passive treatment method not significantly affected by the patient’s concentration or participation, and is a compensatory treatment influenced by feedback from practice, or by the type of help provided by the therapist [30]. These 2 treatment methods have different advantages and are frequently used in clinical practice, however, the number of patients who have been treated with these 2 methods simultaneously have been limited.
Therefore, in this study, we aimed to examine the effects of simultaneous intervention with FES and PA on unilateral neglect in acute-phase stroke patients.
Materials and Methods
1. Participants
This study was conducted on 30 patients who met the participant selection criteria among those who were hospitalized with stroke diagnosis via Computer Tomography or Magnetic Resonance Image in Hospital A in Seoul and Hospital B in Incheon, between April 2016 and October 2016. Specific participant criteria were as follows: (1) Individual with diagnosis of unilateral neglect from a medical doctor and the number of lines neglected in the Albert test above 70%; (2) Individual without brain lesions other than stroke; (3) Individual with less than 3 months since stroke; (4) Individual with The Korean version of the Mini-Mental Status Examination (K-MMSE) score of at least 20, who can follow directions and does not have hearing or vision impairments; (5) Individual informed about the purpose and methods of this study who agreed to participate. Individuals voluntarily agreed to the study after explaining the study purpose and participation method. In order to carry out the research using survey contents and assessment report measurements, all details of this study’s procedures received ethics approval from the Science Research Ethics Committee of Inje University. IRB number is 2-1041024-AB-N-01-20160408-HR-017.
2. Outcome measurements
2.1. K-MMSE
The K-MMSE is an assessment tool that has been translated into Korean and standardized by Kang et al [31]. It contains a total of 6 categories and 27 items consisting of: orientation to time, orientation to place, registration, attention and calculation, recall, language, and visuospatial composition ability. The maximum score was 30, with scores higher than 24 indicating normal, 20–23 points indicating mild cognitive impairment, 10–19 points indicating moderate cognitive impairment, and scores of 9 or less indicating severe cognitive impairment [31,32]. The sensitivity of the K-MMSE was 97.2%, and the specificity was 42.9% [33]. Inclusion criteria required patients with a score of 20 or higher.
2.2. Albert Test
The Albert Test is a type of line crossing test which evaluates unilateral neglect [34]. The test was administered so that the participants were asked to cross out 40 lines on a test sheet. On an A4-size test sheet, 6 lines, each 2.5 cm in length, were placed such that 2 were on the left, 2 in the middle, and 2 on the right, with 4 in the center. The evaluator placed the test paper at the center in front of the participant and demonstrated the test method by marking the 4 lines in the middle of the paper. There was no restriction on the head and eye movement or time. If the participant indicated that all lines had been marked, the test was terminated.
A higher number of uncrossed lines indicated more severe unilateral neglect. Identifying the number of neglected lines in the left, middle, and right sections can indicate the area of unilateral neglect. In this study, the unilateral neglect test was used; therefore, the number of neglected lines among the total 40 lines was measured. The test-retest reliability of the Albert test was highly reliable as r = 0.99 [35].
2.3. Motor-free Visual Perception Test
The Motor-free Visual Perception Test (MVPT) is a standardized assessment tool that assesses the overall visual perception performance of children and adults alike. It was comprised of 36 items that evaluated 5 categories of Visual Discrimination, Figure-ground, Visual Memory, Visual Closure, and Spatial Relation. The results of the test were measured with a total score, or the number of correct items overall, and response scores, or the numbers of answered left and right items, with average time spent for each item. Scoring was conducted with 1 point per item, with the total raw score being 36. Higher scores indicated better visual perception abilities. In this study, the response score in the participants’ responses to the items left was measured. The test-retest reliability of the MVPT was highly reliable as r = 0.77–0.83 [36].
2.4. Catherine Bergego Scale
The Catherine Bergego Scale (CBS) is a behavioural unilateral neglect assessment tool and was designed to assess the existence and extent of unilateral neglect in the scope of daily activities. Unilateral neglect of daily life activities was scored based on 10 items. For each item, 0 point was given for no spatial neglect observed; 1 point was given if the participant always explored the non-affected hemi-space and hesitated toward the affected hemi-space, or the affected hemi-space was sometimes omitted; 2 points were given if the participant always and constantly showed omission or collision of the affected hemi-space; and 3 points were given if the participant does not find or explore the affected hemi-space at all. The total score of 0 indicated normal, 1–10 mild hemi-neglect, 11–20 moderate hemi-neglect, and 21–30 severe hemi-neglect. The CBS is an assessment tool that has a high sensitivity in evaluating hemi-neglect, and its inter-researcher reliability was highly reliable as r = 0.93 [37].
3. Intervention and procedure
For this research, we selected 30 participants that met the participant selection criteria and randomly allocated them into 3 groups: PA plus FES group (Group A), PA group (Group B), and FES group (Group C). Before conducting intervention on the 3 groups, each was assessed with the Albert Test, MVPT, and CBS to test for homogeneity before intervention. All evaluations and interventions were conducted by an occupational therapist with more than 3-year experience. The research director conducted training on the evaluation and intervention methods. Group A received 30 minutes of conventional occupational therapy, followed by FES application on the upper limb on the affected side and PA treatment for 20 minutes, for a total of 50 minutes. Group B received 30 minutes of conventional occupational therapy, followed by PA on the upper limb on the affected side for 20 minutes, for a total of 50 minutes. Group C received 30 minutes of conventional occupational therapy, followed by FES application for 20 minutes, for a total of 50 minutes (Figure 1).
Conventional occupational therapy was conducted for 30 minutes and included joint movement, task-oriented training, and daily life activity training. Joint movement was conducted and included passive joint movement, active adjuvant joint movement, and active joint movement. Task-oriented training considered functional level of the patient and used tools to sequentially conduct activities such as cup-stacking and skateboarding. Daily life activity training included using the restroom, eating a meal, personal hygiene activities, wearing and taking off clothes, and transferring the chair or bed. For PA, following the previous research of Shiraish et al [38], participants wore prism glasses that deflect the axis of vision to the right by 15 degrees, with the proximal surface shaped like a triangle facing the left. PA stimulates the center point by transforming the spatial information from the perceptual coordination of the retinal center in the body-centerd motion coordination to recognise the object’s position, thereby inducing the adaptation effect [24]. When prism glasses were applied, a screen was placed in front of the participant and a scale plate was placed behind the screen. The cover plate was used to prevent visually compensating the patient’s ability to see the movement of his or her arm when pointing to the target. Wearing the prism glasses, the patient performed 50 training repetitions of raising the unimpaired hand to point at the spot thought to be the center of the grid placed in front of him. At this time, the therapist did not mention the point in the center. After 50 repetitions, the participant rested for 30 seconds before starting again, and this was done for a total of 20 minutes [23]. For FES, a product from Micro stim was used. One channel was used, and was set to apply, in shifts, 10 seconds of rest and 10 seconds of stimulation. It was attached below the elbow on the affected side. Although an intensity of 20 Hz is normally recommended, the threshold for electrical stimulation is different for each participant. Therefore, it was set to contract muscles enough to produce sufficient finger and wrist movements [39].
4. Statistical analysis
SPSS widow version 23.0 (IBM Corp., Armonk, NY, USA) was used for statistical analysis. The significance level was set at p < 0.05. General characteristics of research participants were analysed for frequency using descriptive statistics. To compare the unilateral neglect before and after intervention for each group, a paired t test was conducted. One-way ANOVA was used to examine the effectiveness of intervention between the 3 groups.
Results
1. General characteristics of research participants
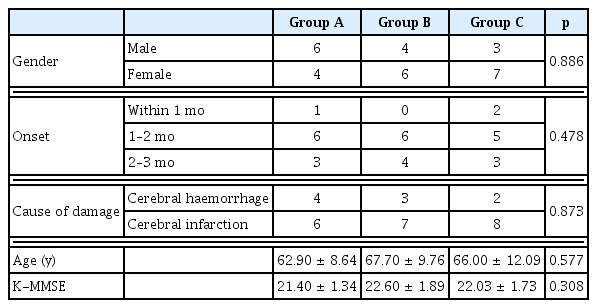
General characteristics of research participants who participated in this study are listed in Table 1. There was a total of 30 participants in this study, with more females (17 participants or 76.4%) than males (13 participants or 23.6%). In Group A, there were 6 males and 4 females; one with onset within 1 month, 6 within 1–2 months, and 3 within 2–3 months; the average age was 62.90 ± 8.64 years; the average K-MMSE score was 21.40 ± 1.34; and the cause of damage was cerebral haemorrhage for 4 people, and cerebral infarction for 6 people. In Group B, there were 4 males and 6 females; 6 with onset within 1–2 months and 4 within 2–3 months; the average age was 67.70 ± 9.76 years; the average K-MMSE score was 22.60 ± 1.89; and the cause of damage was cerebral hemorrhage for 3 people and cerebral infarction for 7 people. In Group C, there were 3 males and 7 females; 2 with onset within 1 month, 5 within 1–2 months, and 3 within 2–3 months; the average age was 66.00 ± 12.09 years; the average K-MMSE score was 22.03 ± 1.73; and the cause of damage was cerebral haemorrhage for 2 people and cerebral infarction for 8 people. There were no statistical differences in gender, onset, age, K-MMSE, or cause of damage among the three groups.
2. Comparison of the MVPT results before and after intervention
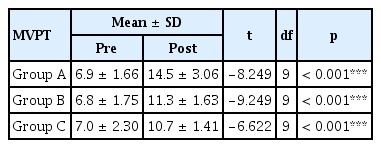
Comparison of the MVPT results before and after intervention were as follows: Statistically significant increases were seen in all 3 groups, from 6.90 ± 1.66 pre-intervention, to 14.50 ± 3.06 post-intervention in Group A (p < 0.001), from 6.80 ± 1.75 pre-intervention, to 11.30 ± 1.63 post-intervention in Group B (p < 0.001), and from 7.00 ± 2.30 pre-intervention, to 10.70 ± 1.41 post-intervention in Group C (p < 0.001; Table 2). However, examining the changes in the visual perception score in each group, the change in Group A was the greatest. The slope between Group B and Group C did not show a significant difference (Figure 2).
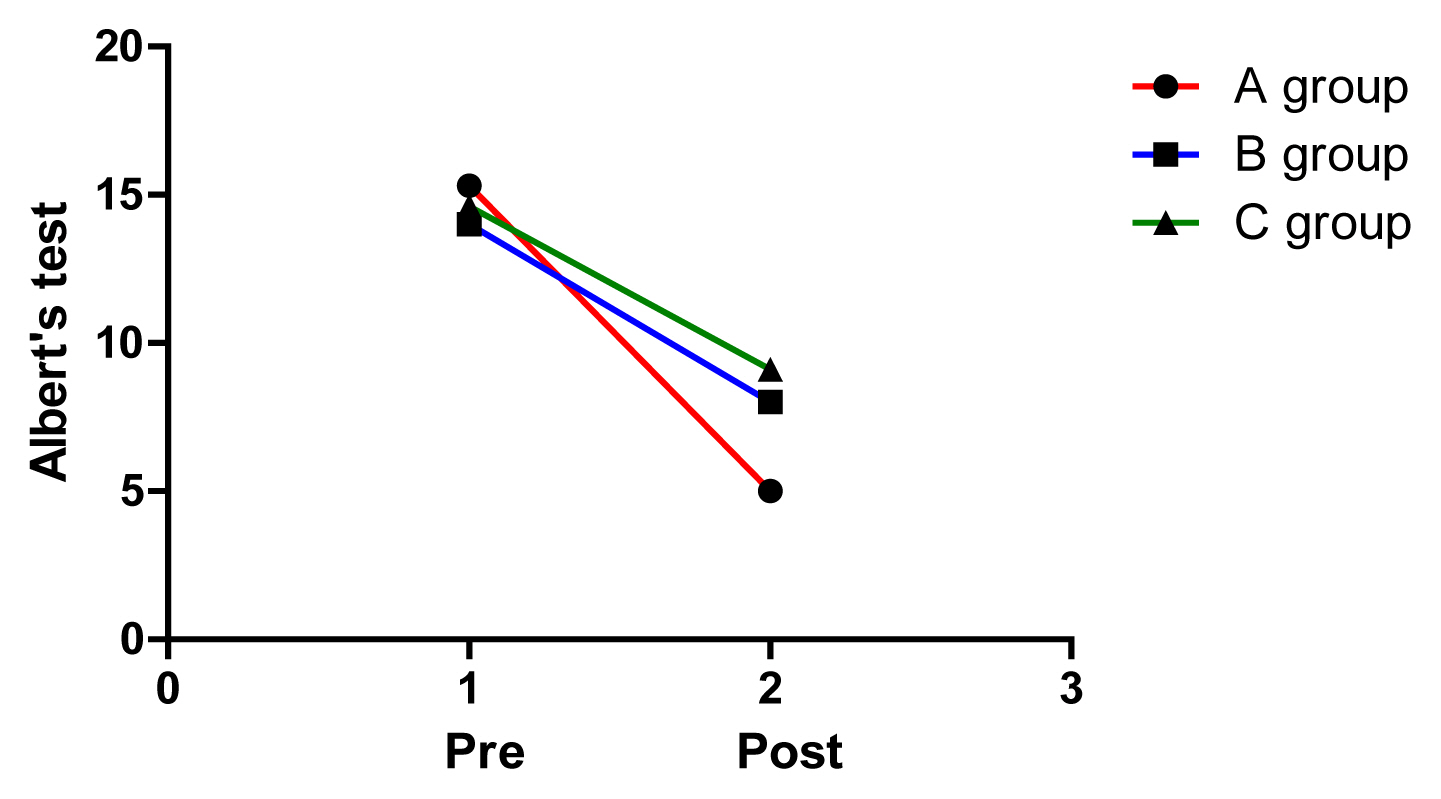
3. Comparison of the Albert’s Test results before and after intervention
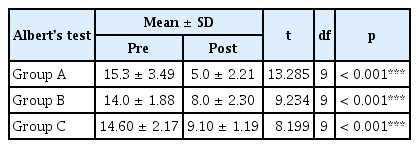
Comparison of the Albert’s Test results before and after intervention were as follows: Statistically significant increases were seen in all 3 groups, from 15.30 ± 3.49 pre-intervention, to 5.00 ± 2.21 post-intervention in Group A (p < 0.001), from 14.00 ± 1.88 pre-intervention, to 8.00 ± 2.30 post-intervention in Group B (p < 0.001), and from 14.60 ± 2.17 pre-intervention, to 9.10 ± 1.19 post-intervention in Group C (p < 0.001; Table 3). However, examining the changes in the visual perception score in each group, the change in Group A was the greatest. The slope between Group B and Group C did not show much difference (Figure 3).
4. Comparison of the CBS results before and after intervention
Comparison of the CBS results before and after intervention are as follows: Statistically significant increases were seen in all three groups, from 20.90 ± 2.99 pre-intervention, to 10.80 ± 2.78 post-intervention in Group A (p < 0.001), from 19.00 ± 2.98 pre-intervention, to 12.70 ± 3.88 post-intervention in Group B (p < 0.001), and from 20.10 ± 2.76 pre-intervention, to 14.80 ± 3.04 post-intervention in Group C (p < 0.001; Table 4). However, examining the changes in the visual perception score in each group, the change in Group A was the greatest. The slope between Group B and Group C did not show much difference (Figure 4).
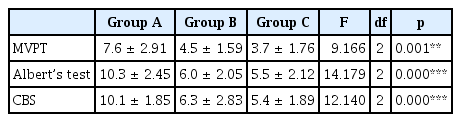
5. Between-group comparison of changes in the results before and after intervention
Between-group comparisons of changes in the results before and after intervention are listed in Table 5. To compare treatment effectiveness, we checked whether there were significant differences in the changes in the MVPT, Albert’s Test, and CBS of each group. Post-intervention the MVPT changes were shown to be 7.6 ± 2.91 for Group A, 4.5 ± 1.59 for Group B, and 3.7 ± 1.76 for Group C. Changes in the MVPT after intervention in Group A were larger in comparison to Group B and Group C, and also showed a statistically significant difference (p < 0.01). Changes in the Albert’s Test after intervention were shown to be 10.3 ± 2.45 for Group A, 6.0 ± 2.05 for Group B, and 5.5 ± 2.12 for Group C. Changes in the Albert’s Test after intervention in Group A were larger in comparison to Group B and Group C, and also showed a statistically significant difference (p < 0.001). Changes in the CBS after intervention were shown to be 10.1 ± 1.85 for Group A, 6.3 ± 2.83 for Group B, and 5.4 ± 1.89 for Group C. Changes in the CBS after intervention in Group A were larger in comparison to Group B and Group C, and also showed a statistically significant difference (p < 0.001).
Discussion
There are various intervention methods for unilateral neglect, however, insufficient research exists on combined intervention methods. Therefore, this study was conducted to examine the effects of combined intervention of PA plus FES, compared to PA intervention or FES intervention alone, for the reduction of unilateral neglect on acute-phase stroke patients.
The unilateral neglect reduced in all 3 groups improved from pre- to post-intervention. Results of previous research, including the study by Han et al [32], in which participants wore prism lenses with a deflection of 10 degrees to the right and pointed at a target 50 times, and of the study by Mizuno et al [40] in which participants wore prism lenses with a deflection of 12 degrees to the right and repeatedly pointed at the target for 20 minutes, showed improvements in unilateral neglect that was especially effective for mild unilateral neglect patients. Yun et al [41] showed that in participants who wore prism lenses with a deflection of 15 degrees to the right and pointed at the target for 15 minutes, showed reduced perceptual and representational neglect among unilateral neglect patients. According to studies by Turton et al [42] and Brink et al [43], PA has been reportedly effective in reducing unilateral neglect in daily life, but was only effective in the self-management part of daily life, as well as in reducing unilateral neglect. Gail and Beverly [16] showed reduction of unilateral neglect in various spaces when FES was applied to the hand on the affected side, while Harding and Riddoch [39] showed improvement in the function of the affected side and reduced unilateral neglect when FES was applied for 20 minutes to the area that stimulates the wrist extensor muscle on the affected side. These studies that applied PA and FES on patients with unilateral neglect showed similar results to our study. All of these studies found that PA and FES have positive effects on reducing unilateral neglect.
In many studies, the treatment effect of PA disappears after 1–2 hours, but the treatment effect persists for more than 1 day with repeated PA [44,45]. However, prism glasses have the limitation of causing patient fatigue [46]. In this study, a 15-degree deviation goggle was used as reported by Shiraishi et al [38], and most studies on PA varied from 7 to 15 degrees, not 10 degrees, with an average angle of 10.7 degrees [47]. However, effects of goggle deviation angle on PA for unilateral neglect should be investigated in future studies.
FES is economical and provides motion by contracting the muscles in the affected side. Thus, it is related to LAT, one of the intervention methods for unilateral neglect and perceptual stimulation. Therefore, this intervention method can reduce unilateral neglect [16]. However, FES is a form of passive limb activation training, and is less effective than active limb activation training [48]. Therefore, by modifying these 2 intervention methods to fit the needs of the clinical setting, and applying them to stroke patients with unilateral neglect, could result in a positive impact.
When intervention effects were compared between the groups, Group A showed a larger change than Group B or C in all tests and showed statistically significant differences. Planowska et al [26] combined left somatosensory stimulation and VST to 40 stroke patients with unilateral neglect for 45 minutes per session, once a day, for 20 sessions total, and reported reduction and activation of left- and right-brain connection more than with the use of VST alone. When Saevarsson et al [19] combined neck vibration and PA treatment to 12 stroke patients with unilateral neglect for 20 minutes, the authors reported more reduction of unilateral neglect and longer persistence of treatment effect compared to when PA treatment was used alone. Similar to these results, previous studies applying a combination of 2 intervention methods on patients with unilateral neglect support a combined intervention method of PA and FES than either treatment alone.
All of the groups in our study exhibited a pre- to post-intervention reduction in unilateral neglect. For the MVPT, all 3 groups showed reduction in unilateral neglect, but the scores for left response were found to be clearly different. All participants belonged in the “Indicate Neglect” group before intervention, but all participants except 2 participants in Group C, belonged in the “Suggest Neglect” group after the intervention. For the Albert’s Test, all 3 groups showed reduction in unilateral neglect, but the average neglect values were found to be clearly different. Group A’s score was 5.0 ± 2.21 with a 25% reduction, Group B’s score was 8.0 ± 2.30 with a 15% reduction, and Group C’s score was 9.10 ± 1.19 with a 14% reduction. For the CBS, all 3 groups showed reduction in unilateral neglect, but the average changes in the score were found to be clearly different among the groups. Group A’s score was 10.8 ± 2.78 with a 33% reduction, Group B’s score was 12.7 ± 3.88 with a 21% reduction, and Group C’s score was 14.8 ± 3.04 with a 18% reduction. All participants showed score decreases in the CBS items 1, 2, 4, and 6. In particular, all participants scored 0 on the items “When shaving or putting on makeup, I forget the left side of my face” and “After eating, I forget to wipe the left side of my mouth.” The CBS items 1, 2, 4, and 6 are items that reveal Personal Neglect, and all participants were shown to greatly improve in this area. Before unilateral neglect intervention, the CBS score was “moderate neglect” or between 11–20 points for 19 participants, and “severe neglect” or between 21–30 points for 11 participants. After intervention, the CBS scores changed to “mild neglect” or between 1–10 points for 12 participants, and “moderate neglect” or between 11–20 points for 18 participants. It is notable that mild neglect was the most common in Group A with 7 people, and there were none in Group C.
Functional changes of self-management in daily life could be identified with the numerical value of CBS; however, this is unreasonable because daily life movement evaluation was not performed in order to confirm the functional changes. Therefore, a method for observing functional changes in such studies should be established.
Comparing the pre- and post-intervention unilateral neglect between the combined intervention of PA plus FES, PA alone, and FES alone showed that all 3 groups showed statistically significant differences, but the combined intervention of PA plus FES showed a statistically significant reduction compared to the other 2 groups for the reduction of unilateral neglect.
The combination of FES and PA is easily accessible in a clinical treatment environment. Furthermore, we confirmed that the combined intervention of PA and FES has a significant effect on the reduction of unilateral neglect in stroke patients. This is significant in that this study provides data for the basis of combining and applying PA and FES in a clinical occupational therapy environment.
The limitations of this research include a small number of participants which makes generalization to all stroke patients with unilateral neglect difficult. In addition, we cannot ignore the effect that conventional occupational therapy will have had on unilateral neglect. Therefore, in future studies, research that considers these limitations is necessary. Moreover, additional comparative research is needed not only on the effects of the combined intervention of PA plus FES, but also the combination of other rehabilitation treatment methods.
Conclusion
The results of this study showed that treatment with FES, PA, and FES and PA combined, all showed statistically significant reduction in unilateral neglect after intervention. Combined PA and FES intervention showed statistically significant reduction in unilateral neglect in comparison to either of the intervention methods used alone. These results indicate that a combined PA and FES intervention method is more effective in unilateral neglect reduction than the individual treatments alone. Although the sample size of our study is insufficient to generalize results, our study supports future research on combined interventions for unilateral neglect.
Notes
Conflicts of Interest
The authors have no conflicts of interest to declare.