Search
- Page Path
- HOME > Search
Original Articles
- Prevalence and patterns of adverse events following childhood immunization and the responses of mothers in Ile-Ife, South West Nigeria: a facility-based cross-sectional survey
- Olorunfemi Akinbode Ogundele, Funmito Omolola Fehintola, Mubarak Salami, Rahmat Usidebhofoh, Mary Aderemi Abaekere
- Osong Public Health Res Perspect. 2023;14(4):291-299. Published online July 27, 2023
- DOI: https://doi.org/10.24171/j.phrp.2023.0071
- 2,264 View
- 134 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 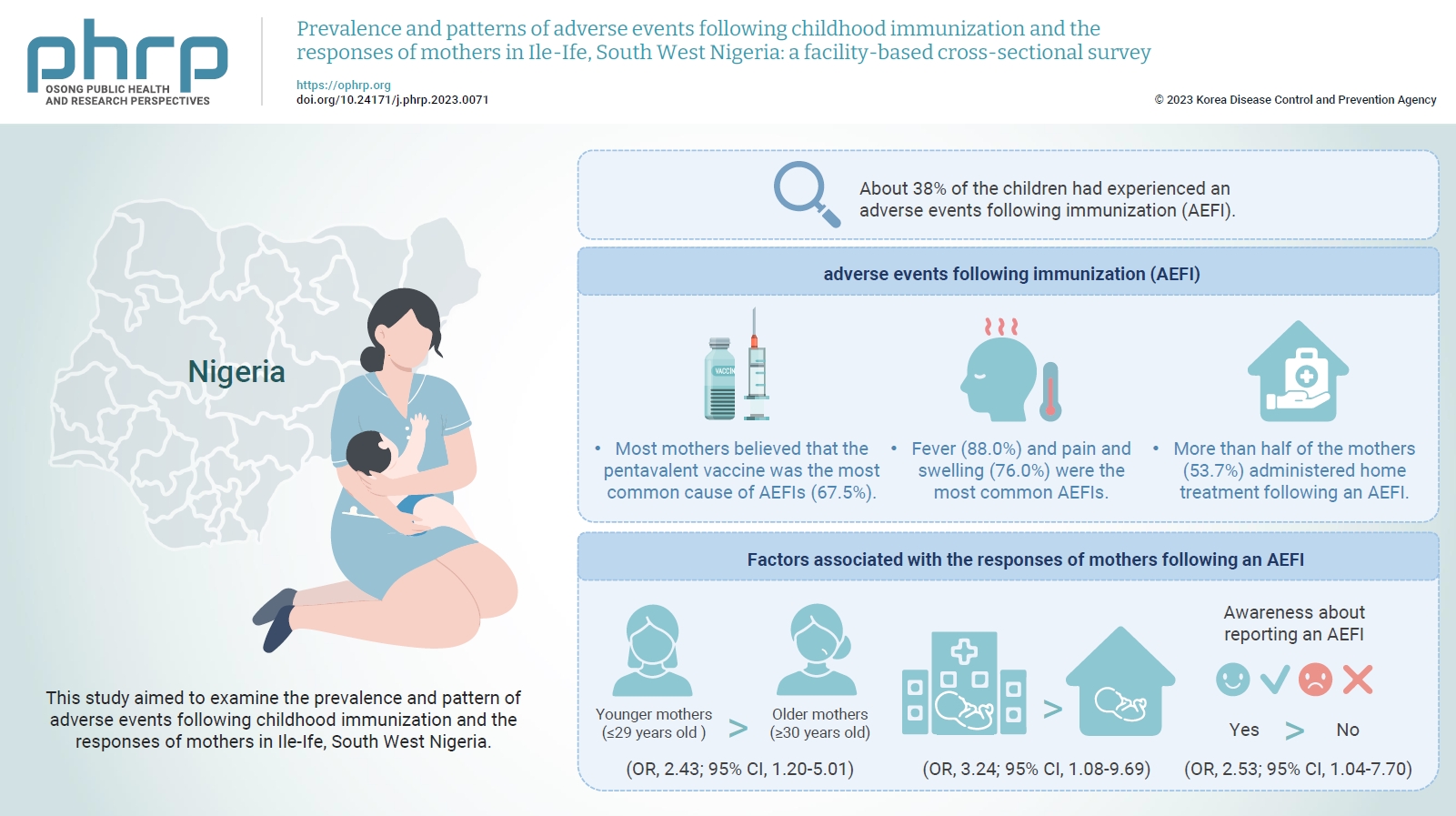
- Objectives
This study aimed to examine the prevalence and pattern of adverse events following childhood immunization and the responses of mothers in Ile-Ife, South West Nigeria.
Methods
This descriptive cross-sectional study was conducted among 422 mothers of children aged 0 to 24 months attending any of the 3 leading immunization clinics in Ile-Ife, Nigeria. The respondents were selected using the multi-stage sampling technique. Data were collected using a pretested structured interviewer-administered questionnaire and analyzed using IBM SPSS ver. 26.0. The chi-square test was used to test associations, while binary logistic regression was used to determine the predictors of mothers’ responses to adverse events following immunization (AEFIs). A p-value of <0.05 was considered statistically significant.
Results
The mean age of the respondents was 29.99±5.74 years. About 38% of the children had experienced an AEFI. Most mothers believed that the pentavalent vaccine was the most common cause of AEFIs (67.5%). Fever (88.0%) and pain and swelling (76.0%) were the most common AEFIs. More than half of the mothers (53.7%) administered home treatment following an AEFI. Younger mothers (odds ratio [OR], 2.43; 95% confidence interval [CI], 1.20–5.01), mothers who delivered their children at a healthcare facility (OR, 3.24; 95% CI, 1.08–9.69), and mothers who were knowledgeable about reporting AEFIs (OR, 2.53; 95% CI, 1.04–7.70) were most likely to respond appropriately to AEFIs.
Conclusion
The proportion of mothers who responded poorly to AEFIs experienced by their children was significant. Therefore, strategies should be implemented to improve mothers’ knowledge about AEFIs to improve their responses.
- Phylogenetic and genome-wide mutational analysis of SARS-CoV-2 strains circulating in Nigeria: no implications for attenuated COVID-19 outcomes
- Daniel B. Kolawole, Malachy I. Okeke
- Osong Public Health Res Perspect. 2022;13(2):101-113. Published online April 22, 2022
- DOI: https://doi.org/10.24171/j.phrp.2021.0329
- 3,361 View
- 65 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 
- Objectives
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is the causative agent of coronavirus disease 2019 (COVID-19). The COVID-19 incidence and mortality rates are low in Nigeria compared to global trends. This research mapped the evolution of SARS-CoV-2 circulating in Nigeria and globally to determine whether the Nigerian isolates are genetically distinct from strains circulating in regions of the world with a high disease burden. Methods: Bayesian phylogenetics using BEAST 2.0, genetic similarity analyses, and genomewide mutational analyses were used to characterize the strains of SARS-CoV-2 isolated in Nigeria. Results: SARS-CoV-2 strains isolated in Nigeria showed multiple lineages and possible introductions from Europe and Asia. Phylogenetic clustering and sequence similarity analyses demonstrated that Nigerian isolates were not genetically distinct from strains isolated in other parts of the globe. Mutational analysis demonstrated that the D614G mutation in the spike protein, the P323L mutation in open reading frame 1b (and more specifically in NSP12), and the R203K/ G204R mutation pair in the nucleocapsid protein were most prevalent in the Nigerian isolates. Conclusion: The SARS-CoV-2 strains in Nigeria were neither phylogenetically nor genetically distinct from virus strains circulating in other countries of the world. Thus, differences in SARS-CoV-2 genomes are not a plausible explanation for the attenuated COVID-19 outcomes in Nigeria.
- Perceptions of the COVID-19 vaccine and willingness to receive vaccination among health workers in Nigeria
- Oluseyi Ademola Adejumo, Olorunfemi Akinbode Ogundele, Cynthia Roli Madubuko, Rosena Olubanke Oluwafemi, Ogochukwu Chinedum Okoye, Kenechukwu Chukwuemeka Okonkwo, Sunday Samson Owolade, Oladimeji Adedeji Junaid, Olutoyin Morenike Lawal, Adenike Christianah Enikuomehin, Maureen Iru Ntaji, Aisha Sokunbi, Aina Omodele Timothy, Olatunji Sunday Abolarin, Emmanuel Olalekan Ali, John Oghenevwirhe Ohaju-Obodo
- Osong Public Health Res Perspect. 2021;12(4):236-243. Published online July 19, 2021
- DOI: https://doi.org/10.24171/j.phrp.2021.0023
- 11,600 View
- 455 Download
- 38 Web of Science
- 36 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 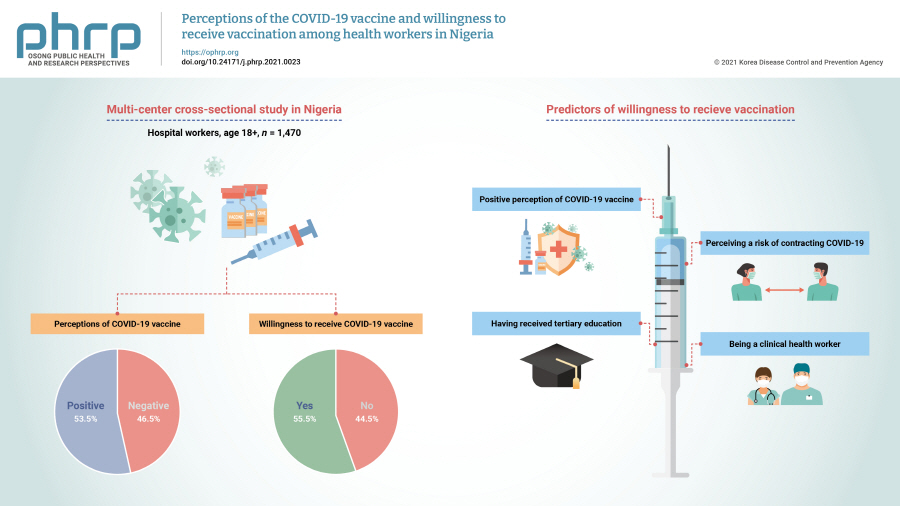
- Objectives
The study aimed to examine health workers’ perceptions of the coronavirus disease 2019 (COVID-19) vaccine in Nigeria and their willingness to receive the vaccine when it becomes available.
Methods
This multi-center cross-sectional study used non-probability convenience sampling to enroll 1,470 hospital workers aged 18 and above from 4 specialized hospitals. A structured and validated self-administered questionnaire was used for data collection. Data entry and analysis were conducted using IBM SPSS ver. 22.0.
Results
The mean age of respondents was 40±6 years. Only 53.5% of the health workers had positive perceptions of the COVID-19 vaccine, and only slightly more than half (55.5%) were willing to receive vaccination. Predictors of willingness to receive the COVID-19 vaccine included having a positive perception of the vaccine (adjusted odds ratio [AOR], 4.55; 95% confidence interval [CI], 3.50−5.69), perceiving a risk of contracting COVID-19 (AOR, 1.50; 95% CI, 1.25–3.98), having received tertiary education (AOR, 3.50; 95% CI, 1.40−6.86), and being a clinical health worker (AOR, 1.25; 95% CI, 1.01−1.68).
Conclusion
Perceptions of the COVID-19 vaccine and willingness to receive the vaccine were sub-optimal among this group. Educational interventions to improve health workers' perceptions and attitudes toward the COVID-19 vaccine are needed. -
Citations
Citations to this article as recorded by- Nigerians’ attitudes and perceptions towards vaccine acceptance during and after the COVID-19 pandemic
Jonas Lotanna Ibekwe, Victor Oluwafemi Femi-Lawal, Jolly Akor Thomas, Faith Uzoamaka Okei, Moses Ojomakpenen Ojile, Oluwatobiloba Oladipupo Akingbulugbe
Journal of Medicine, Surgery, and Public Health.2024; 2: 100066. CrossRef - Knowledge, attitudes, and factors determining the willingness for COVID-19 vaccination among students in Bangladesh: An online-based cross-sectional study
Ashis Talukder, Soheli Sharmin, Chuton Deb Nath, Iqramul Haq, Md. Ismail Hossain, Md. Jakaria Habib, Sabiha Shirin Sara
Journal of Public Health.2024; 32(4): 663. CrossRef - Healthcare professionals’ perception and COVID-19 vaccination attitudes in North-Western Ghana: A multi-center analysis
Augustine Ngmenemandel Balegha, Suburu Abdul-Aziz, Louis Mornah, Pracheth Raghuveer
PLOS ONE.2024; 19(2): e0298810. CrossRef - Behavioral Insights from Vaccine Adoption in Nigeria: Cross-Sectional Survey Findings
Sohail Agha, Ifeanyi Nsofor, Drew Bernard, Sarah Francis, Nandan Rao
Interactive Journal of Medical Research.2024; 13: e47817. CrossRef - COVID-19 vaccine hesitancy in Latin America and Africa: a scoping review
Bruna Aparecida Gonçalves, Camila Carvalho de Souza Amorim Matos, Jonathan Vicente dos Santos Ferreira, Renata Fortes Itagyba, Vinicius Rocha Moço, Marcia Thereza Couto
Cadernos de Saúde Pública.2023;[Epub] CrossRef - Suspecting the Figures: What Church Leaders Think About Government’s Commitment to Combating COVID-19 in Nigeria
Uchechukwu M. Agbo, George C. Nche
Journal of Asian and African Studies.2023; 58(5): 725. CrossRef - Access to COVID-19 vaccines and testing in Africa: the importance of COVAX - Nigeria as a case study
Rafaella Fortini Queiroz Grenfell, Oyetunde Timothy Oyeyemi
Pathogens and Global Health.2023; 117(2): 152. CrossRef - COVID-19 vaccine acceptance prediction: The roles of students’ attitude towards science and mathematics and knowledge of COVID-19 pandemic
Sunday Ogbu, Ogochukwu Ebere Emenike, Amaka Loretta Nwankwo
Electronic Journal of Medical and Educational Tech.2023; 16(2): em2304. CrossRef - Factors associated with COVID-19 vaccine hesitancy among healthcare workers in Cameroon and Nigeria: a web-based cross-sectional study
Jerry Brown Aseneh, Valirie Ndip Agbor, Benjamin Momo Kadia, Elvis Anyaehiechukwu Okolie, Chinelo Janefrances Ofomata, Christie Linonge Etombi, Domin Sone M Ekaney, Yvonne Walburga Joko Fru
International Health.2023; 15(6): 702. CrossRef - Willingness to COVID-19 vaccination: Empirical evidence from EU
Imran Ur Rahman, Arslan Austin, Naveed Nelson
Heliyon.2023; 9(5): e15776. CrossRef - Radiographers’ knowledge, attitude and adherence to standard COVID-19 precautions and the policy implications: a national cross-sectional study in Nigeria
Charles Ikechukwu Ezema, Okechukwu Felix Erondu, Ogochukwu Kelechi Onyeso, Chiedozie James Alumona, Andrew Wueseter Ijever, Charity Ndidiamaka Amarachukwu, Amaeze Augustine Amaeze
Annals of Medicine.2023;[Epub] CrossRef - Declining trends in vaccine confidence across sub-Saharan Africa: A large-scale cross-sectional modeling study
A. de Figueiredo, E. Temfack, R. Tajudeen, H. J. Larson
Human Vaccines & Immunotherapeutics.2023;[Epub] CrossRef - Knowledge and acceptance of COVID-19 vaccine among healthcare workers in Enugu metropolis, Enugu state, Nigeria
Kelechi U. Imediegwu, Jude C. Abor, Chiamaka Q. Onyebuchukwu, Hilary I. Ugwu, Ogechi I. Ugwu, Udo Ego Anyaehie, Oluchi A. Onyia
Frontiers in Public Health.2023;[Epub] CrossRef - COVID-19 vaccination acceptance (uptake, hesitancy, intention to receive and timeliness of the intention to receive) and the determinants among health workers in Ebonyi state, Nigeria: an analytical cross-sectional study
Ugwu I Omale, Onyinyechukwu U Oka, Chidinma I Amuzie, Victor U Uduma, Azuka S Adeke, Cordis O Ikegwuonu, Glory E Nkwo, Ugochi I A Nwali, Osarhiemen Iyare, Richard L Ewah, Olaedo O Nnachi, Okechukwu O Ukpabi, Ifeyinwa M Okeke
BMJ Open.2023; 13(7): e068668. CrossRef - Hesitação vacinal contra a COVID-19 na América Latina e África: uma revisão de escopo
Bruna Aparecida Gonçalves, Camila Carvalho de Souza Amorim Matos, Jonathan Vicente dos Santos Ferreira, Renata Fortes Itagyba, Vinicius Rocha Moço, Marcia Thereza Couto
Cadernos de Saúde Pública.2023;[Epub] CrossRef - The Social Ecological Model: A Framework for Understanding COVID-19 Vaccine Uptake among Healthcare Workers—A Scoping Review
Damian Naidoo, Anna Meyer-Weitz, Kaymarlin Govender
Vaccines.2023; 11(9): 1491. CrossRef - Health service factors affecting the COVID-19 vaccination campaign in a Ghanaian metropolis: A qualitative exploratory study
Susanna Aba Aba Abraham, John Oti Amoah, Dorcas Frempomaa Agyare, Deogratias Kaheeru Sekimpi, Diana Bosomtwe-Duker, Andrews Adjei Druye, Gifty Osei Berchie, Dorcas Obiri-Yeboah
BMJ Open.2023; 13(12): e076184. CrossRef - ‘Why Should I Take the COVID-19 Vaccine after Recovering from the Disease?’ A Mixed-methods Study of Correlates of COVID-19 Vaccine Acceptability among Health Workers in Northern Nigeria
Zubairu Iliyasu, Muhammad R. Garba, Auwalu U. Gajida, Taiwo G. Amole, Amina A. Umar, Hadiza M. Abdullahi, Aminatu A. Kwaku, Hamisu M. Salihu, Muktar H. Aliyu
Pathogens and Global Health.2022; 116(4): 254. CrossRef - A Global Map of COVID-19 Vaccine Acceptance Rates per Country: An Updated Concise Narrative Review
Malik Sallam, Mariam Al-Sanafi, Mohammed Sallam
Journal of Multidisciplinary Healthcare.2022; Volume 15: 21. CrossRef - Knowledge, Attitudes, and Perception towards COVID-19 Vaccination among the Adult Population: A Cross-Sectional Study in Turkey
Meliha Cagla Sonmezer, Taha Koray Sahin, Enes Erul, Furkan Sacit Ceylan, Muhammed Yusuf Hamurcu, Nihal Morova, Ipek Rudvan Al, Serhat Unal
Vaccines.2022; 10(2): 278. CrossRef - Factors influencing COVID-19 vaccine uptake among adults in Nigeria
Halimat Adedeji-Adenola, Olubusola A. Olugbake, Shakirat A. Adeosun, Ismaeel Yunusa
PLOS ONE.2022; 17(2): e0264371. CrossRef - Perception and Prevention Practices Relating to Covid 19 Infection Among Elderly in Ogun State, Nigeria
Adenitire G., Agbede C.O.
International Journal of Public Health and Pharmac.2022; 2(1): 29. CrossRef - Predicting nursing students' intention to attend face‐to‐face classes on school reopening: A theory of planned behavior application
Ryan Michael F. Oducado, Jerome V. Cleofas, Gil P. Soriano
Nursing Forum.2022; 57(5): 733. CrossRef - COVID-19 vaccination in Nigeria: A rapid review of vaccine acceptance rate and the associated factors
Oluwatosin Olu-Abiodun, Olumide Abiodun, Ngozi Okafor, Nusirat Elelu
PLOS ONE.2022; 17(5): e0267691. CrossRef - COVID-19 vaccine acceptance among health care workers in Africa: A systematic review and meta-analysis
Martin Ackah, Louise Ameyaw, Mohammed Gazali Salifu, Delali Pearl Afi Asubonteng, Cynthia Osei Yeboah, Eugene Narkotey Annor, Eunice Abena Kwartemaa Ankapong, Hosea Boakye, Muhammad Shahzad Aslam
PLOS ONE.2022; 17(5): e0268711. CrossRef - A national survey of COVID-19 vaccine acceptance in Nigeria
Ahmad Ibrahim Al-Mustapha, Ochulor Okechukwu, Ademola Olayinka, Oyeniyi Rasheed Muhammed, Muftau Oyewo, Samuel A. Owoicho, Ahmed Tijani Abubakar, Abdulsalam Olabisi, Aliyu Jibril, Simon Ereh, Oluwatosin Enoch Fakayode, Oluwaseun Adeolu Ogundijo, Nusirat E
Vaccine.2022; 40(33): 4726. CrossRef - COVID-19 vaccine hesitancy in Africa: a scoping review
Betty B. B. Ackah, Michael Woo, Lisa Stallwood, Zahra A. Fazal, Arnold Okpani, Ugochinyere Vivian Ukah, Prince A. Adu
Global Health Research and Policy.2022;[Epub] CrossRef - COVID-19 Vaccine Acceptance and Associated Factors Among College Students in Dessie City, Northeastern Ethiopia
Gete Berihun, Zebader Walle, Daniel Teshome, Leykun Berhanu, Mohammed Derso
Journal of Multidisciplinary Healthcare.2022; Volume 15: 1735. CrossRef - Career Aspiration Fulfillment and COVID-19 Vaccination Intention among Nigerian Youth: An Instrumental Variable Approach
Abayomi Samuel Oyekale
International Journal of Environmental Research an.2022; 19(16): 9813. CrossRef - COVID-19 Vaccine Attitude and Its Predictors Among People Living With Chronic Health Conditions in Ibadan, Nigeria
Lucia Yetunde Ojewale, Rotimi Felix Afolabi, Adesola Ogunniyi
International Journal of Public Health.2022;[Epub] CrossRef - Associations between COVID-19 vaccine hesitancy and the experience of violence among women and girls living with and at risk of HIV in Nigeria
Morenike Oluwatoyin Folayan, Olujide Arije, Amaka Enemo, Aaron Sunday, Amira Muhammad, Hasiya Yunusa Nyako, Rilwan Mohammed Abdullah, Henry Okiwu, Erik Lamontagne
African Journal of AIDS Research.2022; 21(4): 306. CrossRef - Willingness to receive COVID-19 vaccine: A survey among medical radiation workers in Nigeria
Grace Ben Inah, Samuel Archibong Efanga, Ekaete Vincent Ukpong, Christiana Ifeyinwa Obiora
Calabar Journal of Health Sciences.2022; 6: 80. CrossRef - Acceptance of COVID-19 vaccine among healthcare workers in Africa, systematic review and meta-analysis
Zerihun Figa, Tesfaye Temesgen, Addisu Getnet Zemeskel, Moges Ganta, Asrat Alemu, Mesfin Abebe, Zemachu Ashuro
Public Health in Practice.2022; 4: 100343. CrossRef - Perception and willingness to accept COVID-19 Vaccines: A cross-sectional survey of the general population of Sokoto State, Nigeria
Oche Mansur Oche, Habibullah Adamu, Musa Yahaya, Hudu Garba Illo, Abdulaziz Mohammad Danmadami, Adamu Ijapa, Asmau Mohammad Wali, Hamza Yusuf, Hafsat Muhammad, Abba Aji, Harapan Harapan
PLOS ONE.2022; 17(12): e0278332. CrossRef - COVID-19 vaccination acceptance among community members and health workers in Ebonyi state, Nigeria: study protocol for a concurrent-independent mixed method analyses of intention to receive, timeliness of the intention to receive, uptake and hesitancy to
Ugwu I Omale, Osarhiemen Iyare, Richard L Ewah, Chidinma I Amuzie, Onyinyechukwu U Oka, Victor U Uduma, Azuka S Adeke, Cordis O Ikegwuonu, Olaedo O Nnachi, Okechukwu O Ukpabi, Ifeyinwa M Okeke, Glory E Nkwo, Ugochi IA Nwali
BMJ Open.2022; 12(12): e061732. CrossRef - Drivers of COVID-19 Vaccine Uptake amongst Healthcare Workers (HCWs) in Nigeria
Sohail Agha, Adaobi Chine, Mathias Lalika, Samikshya Pandey, Aparna Seth, Alison Wiyeh, Alyssa Seng, Nandan Rao, Akhtar Badshah
Vaccines.2021; 9(10): 1162. CrossRef
- Nigerians’ attitudes and perceptions towards vaccine acceptance during and after the COVID-19 pandemic
- Modeling the Spread of Ebola
- Tae Sug Do, Young S. Lee
- Osong Public Health Res Perspect. 2016;7(1):43-48. Published online February 28, 2016
- DOI: https://doi.org/10.1016/j.phrp.2015.12.012
- 2,960 View
- 18 Download
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
This study aims to create a mathematical model to better understand the spread of Ebola, the mathematical dynamics of the disease, and preventative behaviors.
Methods
An epidemiological model is created with a system of nonlinear differential equations, and the model examines the disease transmission dynamics with isolation through stability analysis. All parameters are approximated, and results are also exploited by simulations. Sensitivity analysis is used to discuss the effect of intervention strategies.
Results
The system has only one equilibrium point, which is the disease-free state (S,L,I,R,D) = (N,0,0,0,0). If traditional burials of Ebola victims are allowed, the possible end state is never stable. Provided that safe burial practices with no traditional rituals are followed, the endemic-free state is stable if the basic reproductive number, R0, is less than 1. Model behaviors correspond to empirical facts. The model simulation agrees with the data of the Nigeria outbreak in 2004: 12 recoveries, eight deaths, Ebola free in about 3 months, and an R0 value of about 2.6 initially, which signifies swift spread of the infection. The best way to reduce R0 is achieving the speedy net effect of intervention strategies. One day's delay in full compliance with building rings around the virus with isolation, close observation, and clear education may double the number of infected cases.
Conclusion
The model can predict the total number of infected cases, number of deaths, and duration of outbreaks among others. The model can be used to better understand the spread of Ebola, educate about prophylactic behaviors, and develop strategies that alter environment to achieve a disease-free state. A future work is to incorporate vaccination in the model when the vaccines are developed and the effects of vaccines are known better. -
Citations
Citations to this article as recorded by- Fractional–Order Modeling and Control of COVID-19 with Shedding Effect
Isa A. Baba, Usa W. Humphries, Fathalla A. Rihan, J. E. N. Valdés
Axioms.2023; 12(4): 321. CrossRef - Projecting the impact of an ebola virus outbreak on endangered mountain gorillas
Dawn M. Zimmerman, Emily Hardgrove, Sara Sullivan, Stephanie Mitchell, Eddy Kambale, Julius Nziza, Benard Ssebide, Chantal Shalukoma, Mike Cranfield, Pranav S. Pandit, Sean P. Troth, Taylor Callicrate, Philip Miller, Kirsten Gilardi, Robert C. Lacy
Scientific Reports.2023;[Epub] CrossRef - Mathematical Models for Typhoid Disease Transmission: A Systematic Literature Review
Sanubari Tansah Tresna, Subiyanto, Sudradjat Supian
Mathematics.2022; 10(14): 2506. CrossRef - Fractional COVID-19 Modeling and Analysis on Successive Optimal Control Policies
Mohammed Subhi Hadi, Bülent Bilgehan
Fractal and Fractional.2022; 6(10): 533. CrossRef - Analysis of a Covid-19 model: Optimal control, stability and simulations
Seda İğret Araz
Alexandria Engineering Journal.2021; 60(1): 647. CrossRef - Modeling 2018 Ebola virus disease outbreak with Cholesky decomposition
Lagès Nadège Mouanguissa, Abdul A. Kamara, Xiangjun Wang
Mathematical Methods in the Applied Sciences.2021; 44(7): 5739. CrossRef - Mitigation strategies and compliance in the COVID-19 fight; how much compliance is enough?
Swati Mukerjee, Clifton M. Chow, Mingfei Li, Martin Chtolongo Simuunza
PLOS ONE.2021; 16(8): e0239352. CrossRef - A Generalized Mechanistic Model for Assessing and Forecasting the Spread of the COVID-19 Pandemic
Hamdi Friji, Raby Hamadi, Hakim Ghazzai, Hichem Besbes, Yehia Massoud
IEEE Access.2021; 9: 13266. CrossRef - Analytical solution for post-death transmission model of Ebola epidemics
Abdul A. Kamara, Xiangjun Wang, Lagès Nadège Mouanguissa
Applied Mathematics and Computation.2020; 367: 124776. CrossRef - Modelling the daily risk of Ebola in the presence and absence of a potential vaccine
Stéphanie M.C. Abo, Robert Smith
Infectious Disease Modelling.2020; 5: 905. CrossRef -
Data Fitting and Scenario Analysis of Vaccination in the 2014 Ebola Outbreak in Liberia
Zhifu Xie
Osong Public Health and Research Perspectives.2019; 10(3): 187. CrossRef - Effect of sexual transmission on the West Africa Ebola outbreak in 2014: a mathematical modelling study
Dongmei Luo, Rongjiong Zheng, Duolao Wang, Xueliang Zhang, Yi Yin, Kai Wang, Weiming Wang
Scientific Reports.2019;[Epub] CrossRef - Mathematical modeling of contact tracing as a control strategy of Ebola virus disease
T. Berge, A. J. Ouemba Tassé, H. M. Tenkam, J. Lubuma
International Journal of Biomathematics.2018; 11(07): 1850093. CrossRef - Challenges of Designing and Implementing High Consequence Infectious Disease Response
Joan M. King, Chetan Tiwari, Armin R. Mikler, Martin O’Neill
Disaster Medicine and Public Health Preparedness.2018; 12(5): 563. CrossRef - The potential impact of a prophylactic vaccine for Ebola in Sierra Leone
Erin N. Bodine, Connor Cook, Mikayla Shorten
Mathematical Biosciences and Engineering.2017; 15(2): 337. CrossRef
- Fractional–Order Modeling and Control of COVID-19 with Shedding Effect



 First
First Prev
Prev


