Search
- Page Path
- HOME > Search
Original Articles
- Developing a national surveillance system for stroke and acute myocardial infarction using claims data in the Republic of Korea: a retrospective study
- Tae Jung Kim, Hak Seung Lee, Seong-Eun Kim, Jinju Park, Jun Yup Kim, Jiyoon Lee, Ji Eun Song, Jin-Hyuk Hong, Joongyub Lee, Joong-Hwa Chung, Hyeon Chang Kim, Dong-Ho Shin, Hae-Young Lee, Bum Joon Kim, Woo-Keun Seo, Jong-Moo Park, Soo Joo Lee, Keun-Hwa Jung, Sun U. Kwon, Yun-Chul Hong, Hyo-Soo Kim, Hyun-Jae Kang, Juneyoung Lee, Hee-Joon Bae
- Osong Public Health Res Perspect. 2024;15(1):18-32. Published online January 31, 2024
- DOI: https://doi.org/10.24171/j.phrp.2023.0248
- 925 View
- 58 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 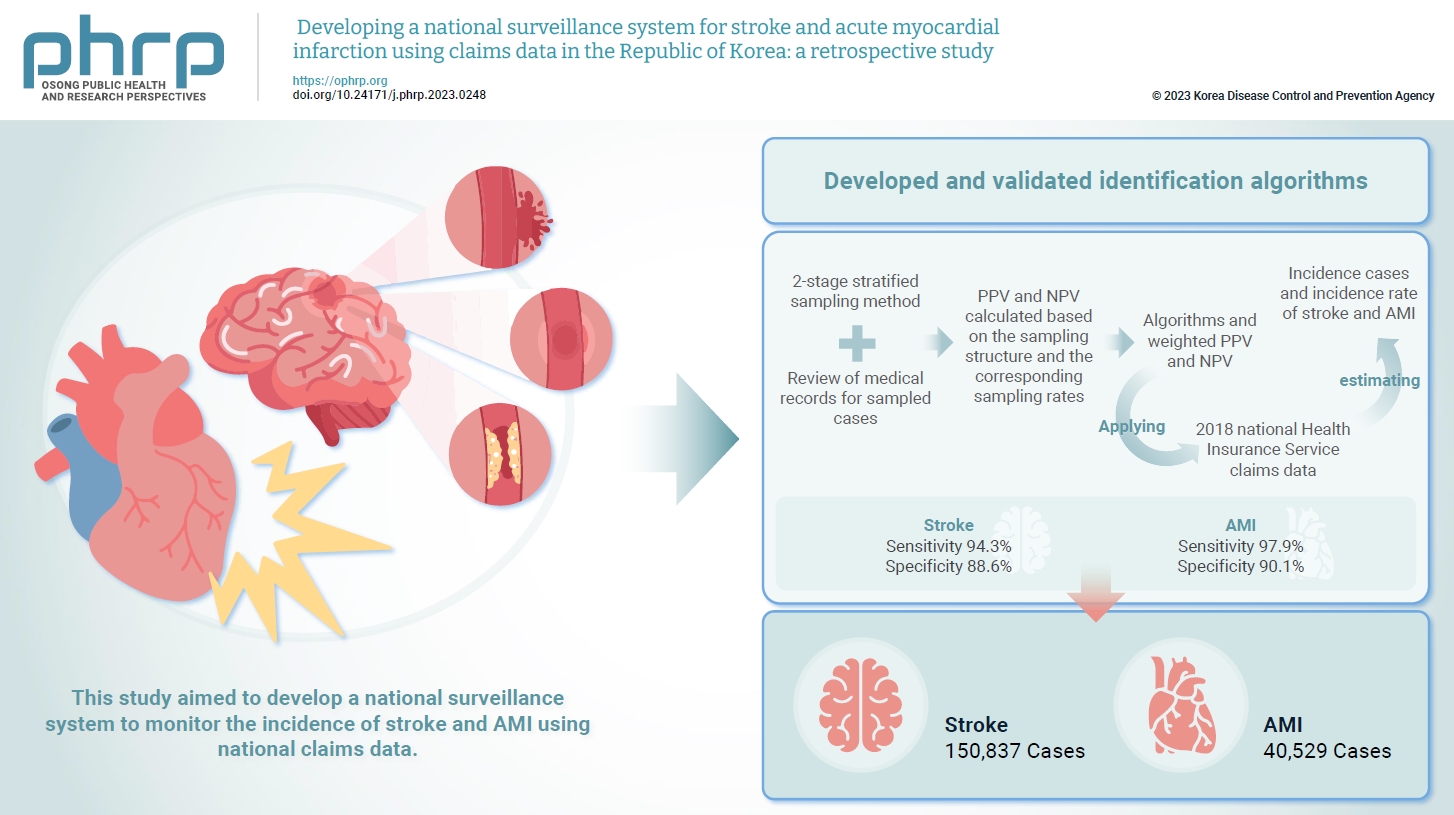
- Objectives
Limited information is available concerning the epidemiology of stroke and acute myocardial infarction (AMI) in the Republic of Korea. This study aimed to develop a national surveillance system to monitor the incidence of stroke and AMI using national claims data. Methods: We developed and validated identification algorithms for stroke and AMI using claims data. This validation involved a 2-stage stratified sampling method with a review of medical records for sampled cases. The weighted positive predictive value (PPV) and negative predictive value (NPV) were calculated based on the sampling structure and the corresponding sampling rates. Incident cases and the incidence rates of stroke and AMI in the Republic of Korea were estimated by applying the algorithms and weighted PPV and NPV to the 2018 National Health Insurance Service claims data. Results: In total, 2,200 cases (1,086 stroke cases and 1,114 AMI cases) were sampled from the 2018 claims database. The sensitivity and specificity of the algorithms were 94.3% and 88.6% for stroke and 97.9% and 90.1% for AMI, respectively. The estimated number of cases, including recurrent events, was 150,837 for stroke and 40,529 for AMI in 2018. The age- and sex-standardized incidence rate for stroke and AMI was 180.2 and 46.1 cases per 100,000 person-years, respectively, in 2018. Conclusion: This study demonstrates the feasibility of developing a national surveillance system based on claims data and identification algorithms for stroke and AMI to monitor their incidence rates.
- Association between face covering policies and the incidence of coronavirus disease 2019 in European countries
- Sookhyun Kim, Jiyoung Oh, Sangwoo Tak
- Osong Public Health Res Perspect. 2023;14(1):31-39. Published online February 1, 2023
- DOI: https://doi.org/10.24171/j.phrp.2022.0287
- 2,013 View
- 72 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 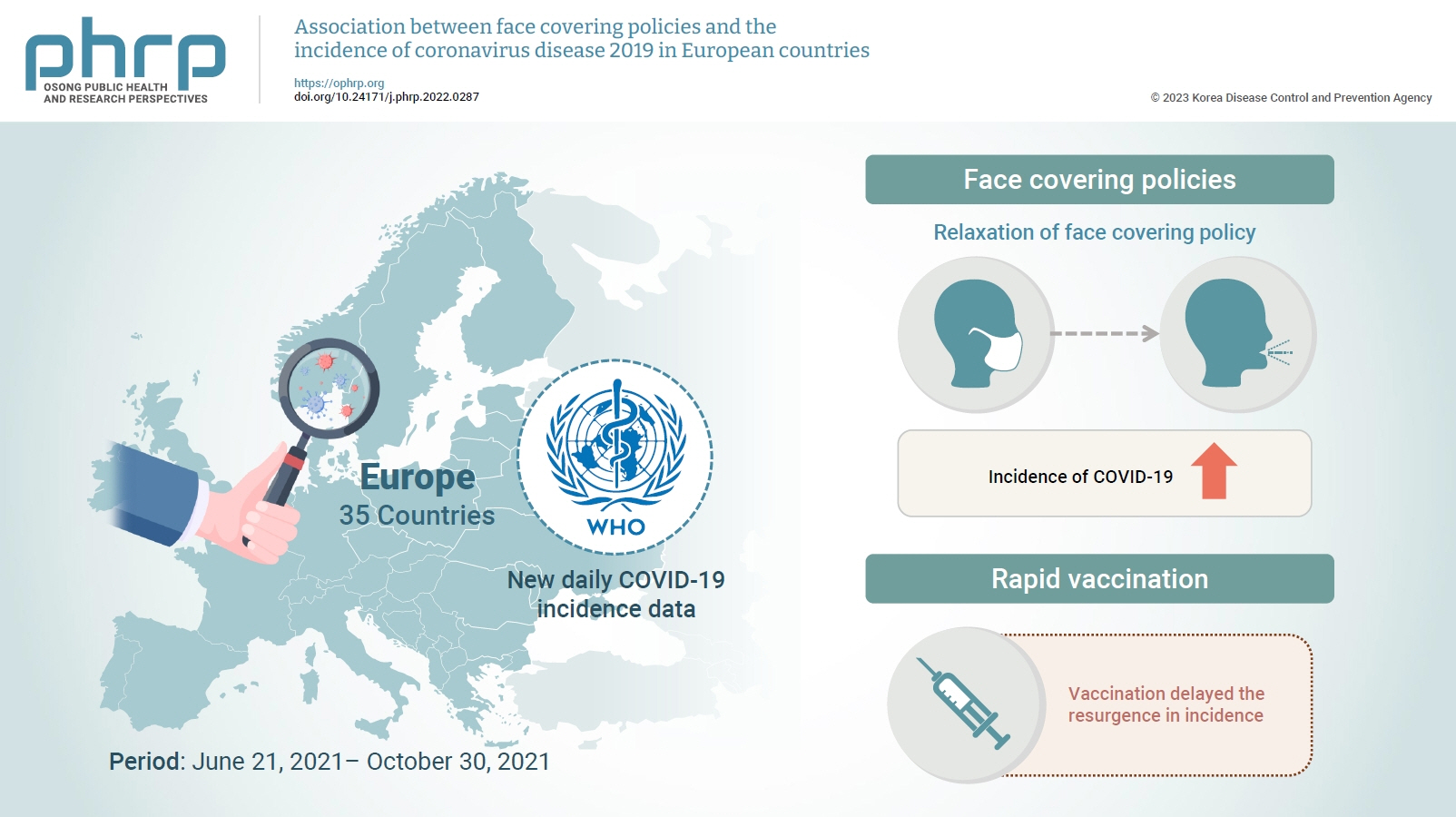
- Objectives
This study was conducted to determine the impact of the strengthening or relaxation of face covering mandates on the subsequent national case incidence of coronavirus disease 2019 (COVID-19) in Europe as the full vaccination rate was increasing.
Methods
European countries in which case incidence increased for 3 consecutive weeks were monitored and analyzed using COVID-19 incidence data shared by the World Health Organization (WHO). The epidemic trend of COVID-19 in Europe was compared with that of countries elsewhere in the world based on WHO weekly epidemiological reports from June 20 to October 30, 2021. In addition, this study provided insight into the impact of government mask mandates on COVID-19 incidence in Europe by measuring the index scores of those facial covering policies before and after mandate relaxation or strengthening. The effects of the vaccination rate and the speed of vaccination on COVID-19 incidence were also analyzed.
Results
The incidence of COVID-19 after the relaxation of face covering mandates was significantly higher than before relaxation. However, no significant difference was observed in vaccination rate between countries with increased and decreased incidence. Instead, rapid vaccination delayed the resurgence in incidence.
Conclusion
The findings suggest that face covering policies in conjunction with rapid vaccination efforts are essential to help mitigate the spread of COVID-19.
- Epidemiology and Inequality in the Incidence and Mortality of Nasopharynx Cancer in Asia
- Neda Mahdavifar, Mahshid Ghoncheh, Abdollah Mohammadian-Hafshejani, Bahman Khosravi, Hamid Salehiniya
- Osong Public Health Res Perspect. 2016;7(6):360-372. Published online December 31, 2016
- DOI: https://doi.org/10.1016/j.phrp.2016.11.002
- 4,010 View
- 21 Download
- 45 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
One of the most common head and neck cancers is nasopharynx cancer. Knowledge about the incidence and mortality of this disease and its distribution in terms of geographical areas is necessary for further study and better planning. Therefore, this study was conducted with the aim of determining the incidence and mortality rates of nasopharynx cancer and its relationship with the Human Development Index (HDI) in Asia in 2012.
Methods
The aim of this ecologic study was to assess the correlation between age-specific incidence rate (ASIR) and age-specific mortality rate (ASMR) with HDI and its components, which include the following: life expectancy at birth, mean years of schooling, and gross national income per capita. Data about SIR and SMR for every Asian country for 2012 were obtained from the global cancer project. We used the correlation bivariate method for the assessment. Statistical significance was assumed if p < 0.05. All reported p values are two-sided. Statistical analyses were performed using SPSS (Version 15.0, SPSS Inc.).
Results
A total of 68,272 cases (males, 71.02%; females, 28.97%; sex ratio, 2.45) and 40,530 mortalities (males, 71.63%; females, 28.36%; sex ratio, 2.52) were recorded in Asian countries in 2012. The five countries with the highest ASIR of nasopharynx cancer were Malaysia, Singapore, Indonesia, Vietnam, and Brunei, and the five countries with the highest ASMR were Indonesia, Vietnam, Singapore, Malaysia, and Brunei. The correlation between HDI and ASIR was 0.097 (p = 0.520) [0.105 in men (p = 0.488) and 0.119 in women (p = 0.901)]. The correlation between HDI and ASMR was –0.102 (p = 0.502) [–0.072 in men (p = 0.633) and –0.224 in women (p = 0.134)].
Conclusion
Nasopharynx cancer is native to Southeast Asia. The highest incidence and mortality rates are found in Malaysia, Singapore, Indonesia, Vietnam, and Brunei. No significant relation was found between the standardized incidence and mortality rates of nasopharynx cancer and the HDI components. Further studies are recommended in Southeast Asian countries in order to find the etiology of cancer, as well as its diagnosis and treatment. -
Citations
Citations to this article as recorded by- Regulatory role of miRNAs in nasopharyngeal cancer involving PTEN/PI3K/AKT, TGFβ/SMAD, RAS/MAPK, Wnt/β‐catenin and pRB‐E2F signaling pathways: A review
Rabiatul Basria S. M. N. Mydin, Adam Azlan, Simon I. Okekpa, Nigel J. Gooderham
Cell Biochemistry and Function.2024;[Epub] CrossRef - Rapid and sensitive detection of Epstein-Barr virus antibodies in nasopharyngeal carcinoma by chemiluminescence strips based on iron-porphyrin single atom nanozyme
Daji Wang, Jie Wang, Dan Liu, Jiuyang He, Meiying Wang, Haibing Huang, Guohui Nie, Hui Ding, Xiyun Yan
Nano Research.2024; 17(3): 1827. CrossRef - The association between chronic sinonasal inflammation and nasopharyngeal carcinoma - A systematic review and meta-analysis
Yuxing Wang, Kylynn Kathleen Koh, Elizabeth Chua, Kimberley Liqin Kiong, Yu Heng Kwan, Tze Choong Charn
American Journal of Otolaryngology.2024; 45(2): 104206. CrossRef - Correlation between socioeconomic indices and epidemiological indices of thyroid cancer from 1990 to 2019 year: a global ecologic study
Zahra Maleki, Jafar Hassanzadeh, Haleh Ghaem
BMC Cancer.2024;[Epub] CrossRef - Study of Three Potential Diagnostic Biomarkers in Nasopharyngeal Carcinoma Samples from Guilan, North of Iran
Saghi Jani Kargar Moghaddam, Amaneh Mohammadi Roushandeh, Mehryar Habibi Roudkenar, Shadman Nemati, Nima Najafi-Ghalehlou, Toofan Pakzad, Masoud Hamidi
International Archives of Otorhinolaryngology.2023; 27(03): e461. CrossRef - Oncogenic Viruses-Encoded microRNAs and Their Role in the Progression of Cancer: Emerging Targets for Antiviral and Anticancer Therapies
Mahmoud Kandeel
Pharmaceuticals.2023; 16(4): 485. CrossRef - Nasopharyngeal Carcinoma Subtype Discovery via Immune Cell Scores from Tumor Microenvironment
Yanbo Sun, Yun Liu, Hanqi Chu, Zhen-Jian Zhuo
Journal of Immunology Research.2023; 2023: 1. CrossRef - The application of Aptamer in biomarker discovery
Yongshu Li, Winnie Wailing TAM, Yuanyuan Yu, Zhenjian Zhuo, Zhichao Xue, Chiman Tsang, Xiaoting Qiao, Xiaokang Wang, Weijing Wang, Yongyi Li, Yanyang Tu, Yunhua Gao
Biomarker Research.2023;[Epub] CrossRef - Blood-based DNA methylation in advanced Nasopharyngeal Carcinoma exhibited distinct CpG methylation signature
Koustav Chatterjee, Sudipa Mal, Monalisha Ghosh, Nabanita Roy Chattopadhyay, Sankar Deb Roy, Koushik Chakraborty, Syamantak Mukherjee, Moatoshi Aier, Tathagata Choudhuri
Scientific Reports.2023;[Epub] CrossRef - Circular RNA circ_0008450 regulates the proliferation, migration, invasion, apoptosis and chemosensitivity of CDDP-resistant nasopharyngeal carcinoma cells by the miR-338-3p/SMAD5 axis
Lin Liu, Bin Lu, Yan Li
Anti-Cancer Drugs.2022; 33(1): e260. CrossRef - Hypermethylation of the RASSF1A gene promoter as the tumor DNA marker for nasopharyngeal carcinoma
Thuan Duc Lao, Hue Hong Thieu, Dung Huu Nguyen, Thuy Ai Huyen Le
The International Journal of Biological Markers.2022; 37(1): 31. CrossRef - miR-135b-5p Targets SIRT1 to Inhibit Deacetylation of c-JUN and Increase MMP7 Expression to Promote Migration and Invasion of Nasopharyngeal Carcinoma Cells
Yali Cheng
Molecular Biotechnology.2022; 64(6): 693. CrossRef - Trends in the Incidence of Nasopharyngeal Cancer in Saudi Arabia Across One Decade (2007 to 2016)
Abdualrahman F Kabli, Khalil F Miyajan, Abdulmohsen S Alqurashi, Ammar K Mandili, Revan M Mujahed, Bayan F Hafiz, Roaa M Mandora, Ameen Z Herabi
Cureus.2022;[Epub] CrossRef - Causes of Death in Long-Term Nasopharyngeal Carcinoma Survivors
Shi-Ping Yang, Ming-Yue Rao, Qing-Shuang Chen, Ping Zhou, Chen-Lu Lian, San-Gang Wu
Frontiers in Public Health.2022;[Epub] CrossRef - Epstein-Barr Virus (EBV) Is Mostly Latent and Clonal in Angioimmunoblastic T Cell Lymphoma (AITL)
Racha Bahri, François Boyer, Mohamad Adnan Halabi, Alain Chaunavel, Jean Feuillard, Arnaud Jaccard, Sylvie Ranger-Rogez
Cancers.2022; 14(12): 2899. CrossRef - Ferroptosis-related gene ATG5 is a novel prognostic biomarker in nasopharyngeal carcinoma and head and neck squamous cell carcinoma
Ming Shi, Jiangnan Du, Jingjing Shi, Yunchuanxiang Huang, Yan Zhao, Lan Ma
Frontiers in Bioengineering and Biotechnology.2022;[Epub] CrossRef - Platelet to Lymphocytes Ratio to Predict Nasopharyngeal Carcinoma Progressivity
Goesti Yudistira, Yussy Afriani Dewi, Melati Sudiro
Open Access Macedonian Journal of Medical Sciences.2022; 10(B): 2189. CrossRef - Skin sparing in intensity-modulated radiation therapy of nasopharyngeal carcinoma
MisbaHamid Baba, BenoyK Singh, Shaq ulQamar Wani
Journal of Medical Physics.2022; 47(3): 243. CrossRef - Assessment of Response to Chemoradiation and Radiation Therapy in Patients with Nasopharyngeal Carcinoma
Sebastian Ario Susanto, Yussy Afriani Dewi, Raden Ayu Hardianti Saputri
Open Access Macedonian Journal of Medical Sciences.2022; 10(B): 2307. CrossRef - Genetic variants in NKG2D axis and susceptibility to Epstein–Barr virus-induced nasopharyngeal carcinoma
Nguyen Hoang Viet, Nguyen Quang Trung, Le Thanh Dong, Ly Quoc Trung, J. Luis Espinoza
Journal of Cancer Research and Clinical Oncology.2021; 147(3): 713. CrossRef - Corticosteroid Therapy in Optic Neuropathy Secondary to Nasopharyngeal Carcinoma
Zulaikha Wahab, Evelyn Tai, Wan-Hazabbah Wan Hitam, Khairy Shamel Sonny Teo
Cureus.2021;[Epub] CrossRef - The Effect of Hispidulin, a Flavonoid from Salvia plebeia, on Human Nasopharyngeal Carcinoma CNE-2Z Cell Proliferation, Migration, Invasion, and Apoptosis
Yiqun Dai, Xiaolong Sun, Bohan Li, Hui Ma, Pingping Wu, Yingping Zhang, Meilin Zhu, Hong-Mei Li, Minjian Qin, Cheng-Zhu Wu
Molecules.2021; 26(6): 1604. CrossRef - δ-Tocotrienol induces apoptosis and inhibits proliferation of nasopharyngeal carcinoma cells
Junjun Shen, Tao Yang, Yiping Tang, Tianyi Guo, Ting Guo, Tao Hu, Feijun Luo, Qinlu Lin
Food & Function.2021; 12(14): 6374. CrossRef - WNT8B as an Independent Prognostic Marker for Nasopharyngeal Carcinoma
Chawalit Ngernsombat, Pongphol Prattapong, Noppadol Larbcharoensub, Krittika Khotthong, Tavan Janvilisri
Current Oncology.2021; 28(4): 2529. CrossRef - Nasopharyngeal Carcinoma and Its Association with Epstein-Barr Virus
Harish N. Vasudevan, Sue S. Yom
Hematology/Oncology Clinics of North America.2021; 35(5): 963. CrossRef - Association between stage and histopathological type of nasopharyngeal cancer on occurrence of postirradiation otitis media with effusion
Lina Lasminingrum, Shinta Fitri Boesoeri, Sally Mahdiani, Eveline Sabrina Ranti
International Journal of Surgery Open.2021; 36: 100376. CrossRef - Current Status and Future Perspectives about Molecular Biomarkers of Nasopharyngeal Carcinoma
Pui Yan Siak, Alan Soo-Beng Khoo, Chee Onn Leong, Boon-Peng Hoh, Shiau-Chuen Cheah
Cancers.2021; 13(14): 3490. CrossRef - Carcinomatous‑like mastitis due to axillary lymphadenopathy in a case of nasopharyngeal carcinoma: A case report
Cristina Oprean, Nusa Segarceanu, Alexandra Stan, Cristian Suciu, Daciana Grujic, Ioana Rivis, Alis Liliana Dema, Ana Bredicean
Experimental and Therapeutic Medicine.2021;[Epub] CrossRef - Dosimetric Comparison of Helical Tomotherapy, Volume-Modulated Arc Therapy, and Fixed-Field Intensity-Modulated Radiation Therapy in Locally Advanced Nasopharyngeal Carcinoma
Shan Lu, Huiqi Fan, Xueyuan Hu, Xin Li, Yingying Kuang, Deyang Yu, Shanshan Yang
Frontiers in Oncology.2021;[Epub] CrossRef - The dosimetric comparison between tomotherapy and RapidArc in normal tissue sparing for nasopharyngeal carcinoma
Pubade Kaewpruk, Somvilai Chakrabandhu, Somsak Wanwilairat, Wannapha Nobnop
Journal of Radiotherapy in Practice.2020; 19(3): 237. CrossRef - Combination of Plasma MIF and VCA-IgA Improves the Diagnostic Specificity for Patients With Nasopharyngeal Carcinoma
Ning Xue, Shan Xing, Weiguo Ma, Jiahe Sheng, Zhiliang Huang, Qingxia Xu
Technology in Cancer Research & Treatment.2020; 19: 153303382093577. CrossRef - Pathological features of nasopharyngeal carcinoma: A single-center study in Vietnam
Nguyen Cuong Pham, Thanh Xuan Nguyen, Nguyen Tuong Pham, Thanh Chinh Phan, Hai Thanh Phan
Annals of Cancer Research and Therapy.2020; 28(2): 125. CrossRef - Association between variant alleles of major histocompatibility complex class II regulatory genes and nasopharyngeal carcinoma susceptibility
Ping Zhou, Sha Liu, Nan-Nan Ji, Shuang Zhang, Peng Wang, Bing Lin, Ping Yang, Xian-Tao Lin, Yi-Zheng Cai, Zi-Ming Wang, Han Zhou, Shi-Yao Sun, Xin-Bao Hao
European Journal of Cancer Prevention.2020; 29(6): 531. CrossRef - Hyperperfusion Syndrome and Baroreflex Failure following Carotid Artery Angioplasty and Stenting for Symptomatic Radiation-Associated Carotid Artery Stenosis
Hui-Meng Chang
Case Reports in Neurology.2020; 12(Suppl. 1): 76. CrossRef - Novel patterns of the Epstein-Barr nuclear antigen (EBNA-1) V-Val subtype in EBV-associated nasopharyngeal carcinoma from Vietnam
LD Thuan, ND Kha, NT Minh, LHA Thuy
Balkan Journal of Medical Genetics.2019; 22(1): 61. CrossRef - miR-29c regulates resistance to paclitaxel in nasopharyngeal cancer by targeting ITGB1
Limin Huang, Chaoquan Hu, Hui Chao, Rongpin Wang, He Lu, Hong Li, Hui Chen
Experimental Cell Research.2019; 378(1): 1. CrossRef - Systematic review and meta-analysis of prognostic microRNA biomarkers for survival outcome in nasopharyngeal carcinoma
Shanthi Sabarimurugan, Chellan Kumarasamy, Siddhartha Baxi, Arikketh Devi, Rama Jayaraj, Yukinori Takenaka
PLOS ONE.2019; 14(2): e0209760. CrossRef - Epstein‐Barr virus strain variation and cancer
Teru Kanda, Misako Yajima, Kazufumi Ikuta
Cancer Science.2019; 110(4): 1132. CrossRef - Nasopharyngeal cancer in Saudi Arabia: Epidemiology and possible risk factors
Abdullah Dakheel Alotaibi, Hussain Gadelkarim Ahmed, Abdelbaset Mohamed Elasbali
Journal of Oncological Sciences.2019; 5(1): 23. CrossRef - Association BetweenLMP-1,LMP-2, and miR-155 Expression as Potential Biomarker in Nasopharyngeal Carcinoma Patients: A Case/Control Study in Vietnam
Thuan Duc Lao, Thuy Ai Huyen Le
Genetic Testing and Molecular Biomarkers.2019; 23(11): 815. CrossRef - Lapatinib sensitivity in nasopharyngeal carcinoma is modulated by SIRT2-mediated FOXO3 deacetylation
Sathid Aimjongjun, Zimam Mahmud, Yannasittha Jiramongkol, Glowi Alasiri, Shang Yao, Ernesto Yagüe, Tavan Janvilisri, Eric W.-F. Lam
BMC Cancer.2019;[Epub] CrossRef - PPARβ/δ Agonist GW501516 Inhibits Tumorigenicity of Undifferentiated Nasopharyngeal Carcinoma in C666-1 Cells by Promoting Apoptosis
Yangyang Ji, Hui Li, Fang Wang, Linglan Gu
Frontiers in Pharmacology.2018;[Epub] CrossRef - Pembrolizumab in Asia‐Pacific patients with advanced head and neck squamous cell carcinoma: Analyses from KEYNOTE‐012
Makoto Tahara, Kei Muro, Yasuhisa Hasegawa, Hyun Cheol Chung, Chia‐Chi Lin, Bhumsuk Keam, Kenichi Takahashi, Jonathan D. Cheng, Yung‐Jue Bang
Cancer Science.2018; 109(3): 771. CrossRef - Childhood Nasopharyngeal Carcinoma (NPC): A Review of Clinical-Imaging Features and Recent Trends in Management
Mark Yoi Sun Soo
International Journal of Pediatrics and Child Heal.2018; 6: 1. CrossRef - KISS1gene suppresses metastasis of nasopharyngeal cancerviaactivation of the ERK1/2 pathway
Tingting Li, Qian Sun, Yan Zhou, Zelai He, Hao Liu, Ping Xiang, Jin Xi, Xiazi Zhang, Hao Jiang
RSC Advances.2017; 7(84): 53445. CrossRef
- Regulatory role of miRNAs in nasopharyngeal cancer involving PTEN/PI3K/AKT, TGFβ/SMAD, RAS/MAPK, Wnt/β‐catenin and pRB‐E2F signaling pathways: A review
- Modification of AxSYM Human Immunodeficiency Virus Assay to Identify Recent Human Immunodeficiency Virus Infections in Korean Human Immunodeficiency Virus-Positive Individuals
- Jin-Sook Wang, Mee-Kyung Kee, Byeong-Sun Choi, Sung Soon Kim
- Osong Public Health Res Perspect. 2015;6(3):184-191. Published online June 30, 2015
- DOI: https://doi.org/10.1016/j.phrp.2015.06.002
- 2,715 View
- 18 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
To estimate human immunodeficiency virus (HIV) incidence using HIV avidity assays in Korea, we established a serological testing method to differentiate recent HIV infections from long-standing ones.
Methods
We adopted two incidence assays, the BED HIV-1 incidence test (Calypte Biomedical) and an HIV avidity assay (using Abbott AxSYM HIV Antigen/Antibody Combo), and performed them on Korean HIV samples obtained from 81 HIV seroconverters (n = 193), 135 HIV-positive samples, and three HIV commercial incidence panels (PRB965, PRB933, and PRB601 from SeaCare). To determine the most optimal concentration of the chaotropic agent (Guanidine) and the cutoff value for the avidity assay, we evaluated the sensitivity and specificity of the assay at different concentration levels.
Results
We determined that the concentration of Guanidine to be used in the avidity assay was 1.5M. The cutoff value of the avidity index (AI) was 0.8, and the sensitivity and specificity were 90.2% and 83.8%, respectively, under this condition. The gray zone for the avidity assay was 0.75–0.85 AI. The mean of coefficient of variation was low, at 5.43%.
Conclusion
An optimized avidity assay for the diagnosis of recent HIV infections using Korean samples was established. This assay will be applied to investigate the level of recent infection and will provide basic data to the HIV prevention policy in Korea. -
Citations
Citations to this article as recorded by- Characteristics of recent HIV infection among individuals newly diagnosed as HIV-positive in South Korea (2008–2015)
Myeongsu Yoo, Jin-Sook Wang, Su-Jin Park, Jeong-ok Cha, Yoonhee Jung, Yoon-Seok Chung, Myung Guk Han, Byeong-Sun Choi, Sung-Soon Kim, Mee-Kyung Kee
Scientific Reports.2022;[Epub] CrossRef
- Characteristics of recent HIV infection among individuals newly diagnosed as HIV-positive in South Korea (2008–2015)
- Joint Disease Mapping of Two Digestive Cancers in Golestan Province, Iran Using a Shared Component Model
- Parisa Chamanpara, Abbas Moghimbeigi, Javad Faradmal, Jalal Poorolajal
- Osong Public Health Res Perspect. 2015;6(3):205-210. Published online June 30, 2015
- DOI: https://doi.org/10.1016/j.phrp.2015.02.002
- 2,755 View
- 16 Download
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
Recent studies have suggested the occurrence patterns and related diet factor of esophagus cancer (EC) and gastric cancer (GC). Incidence of these cancers was mapped either in general and stratified by sex. The aim of this study was to model the geographical variation in incidence of these two related cancers jointly to explore the relative importance of an intended risk factor, diet low in fruit and vegetable intake, in Golestan, Iran.
Methods
Data on the incidence of EC and GC between 2004 and 2008 were extracted from Golestan Research Center of Gastroenterology and Hepatology, Hamadan, Iran. These data were registered as new observations in 11 counties of the province yearly. The Bayesian shared component model was used to analyze the spatial variation of incidence rates jointly and in this study we analyzed the data using this model. Joint modeling improved the precision of estimations of underlying diseases pattern, and thus strengthened the relevant results.
Results
From 2004 to 2008, the joint incidence rates of the two cancers studied were relatively high (0.8–1.2) in the Golestan area. The general map showed that the northern part of the province was at higher risk than the other parts. Thus the component representing diet low in fruit and vegetable intake had larger effect of EC and GC incidence rates in this part. This incidence risk pattern was retained for female but for male was a little different.
Conclusion
Using a shared component model for joint modeling of incidence rates leads to more precise estimates, so the common risk factor, a diet low in fruit and vegetables, is important in this area and needs more attention in the allocation and delivery of public health policies. -
Citations
Citations to this article as recorded by- A Systematic Review of Joint Spatial and Spatiotemporal Models in Health Research
Getayeneh Antehunegn Tesema, Zemenu Tadesse Tessema, Stephane Heritier, Rob G. Stirling, Arul Earnest
International Journal of Environmental Research an.2023; 20(7): 5295. CrossRef - Multivariate Bayesian Semiparametric Regression Model for Forecasting and Mapping HIV and TB Risks in West Java, Indonesia
I. Gede Nyoman Mindra Jaya, Budhi Handoko, Yudhie Andriyana, Anna Chadidjah, Farah Kristiani, Mila Antikasari
Mathematics.2023; 11(17): 3641. CrossRef - Evaluating an intervention for neural tube defects in coal mining cites in China: a temporal and spatial analysis
Ningxu Zhang, Yilan Liao, Zhoupeng Ren
International Health.2021; 13(2): 161. CrossRef Epidemiologic Study of Gastric Cancer in Iran: A Systematic Review
Khadijeh Kalan Farmanfarma, Neda Mahdavifar, Soheil Hassanipour, Hamid Salehiniya
Clinical and Experimental Gastroenterology.2020; Volume 13: 511. CrossRef- Bivariate spatio-temporal shared component modeling: Mapping of relative death risk due to colorectal and stomach cancers in Iran provinces
Vahid Ahmadipanahmehrabadi, Akbar Hassanzadeh, Behzad Mahaki
International Journal of Preventive Medicine.2019; 10(1): 39. CrossRef - Spatial Patterns of Ischemic Heart Disease in Shenzhen, China: A Bayesian Multi-Disease Modelling Approach to Inform Health Planning Policies
Qingyun Du, Mingxiao Zhang, Yayan Li, Hui Luan, Shi Liang, Fu Ren
International Journal of Environmental Research an.2016; 13(4): 436. CrossRef - Disappeared persons and homicide in El Salvador
Carlos Carcach, Evelyn Artola
Crime Science.2016;[Epub] CrossRef
- A Systematic Review of Joint Spatial and Spatiotemporal Models in Health Research
- The Recency Period for Estimation of Human Immunodeficiency Virus Incidence by the AxSYM Avidity Assay and BED-Capture Enzyme Immunoassay in the Republic of Korea
- Hye-Kyung Yu, Tae-Young Heo, Na-Young Kim, Jin-Sook Wang, Jae-Kyeong Lee, Sung Soon Kim, Mee-Kyung Kee
- Osong Public Health Res Perspect. 2014;5(4):187-192. Published online August 31, 2014
- DOI: https://doi.org/10.1016/j.phrp.2014.06.002
- 2,700 View
- 19 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
Measurement of the incidence of the human immunodeficiency virus (HIV) is very important for epidemiological studies. Here, we determined the recency period with the AxSYM avidity assay and the BED-capture enzyme immunoassay (BED-CEIA) in Korean seroconverters.
Methods
Two hundred longitudinal specimens from 81 seroconverters with incident HIV infections that had been collected at the Korea National Institute of Health were subjected to the AxSYM avidity assay (cutoff = 0.8) and BED-CEIA (cutoff = 0.8). The statistical method used to estimate the recency period in recent HIV infections was nonparametric survival analyses. Sensitivity and specificity were calculated for 10-day increments from 120 days to 230 days to determine the recency period.
Results
The mean recency period of the avidity assay and BED-CEIA using a survival method was 158 days [95% confidence interval (CI), 135–181 days] and 189 days (95% CI, 170–208 days), respectively. Based on the use of sensitivity and specificity, the mean recency period for the avidity assay and BED-CEIA was 150 days and 200 days, respectively.
Conclusion
We determined the recency period to estimate HIV incidence in Korea. These data showed that the nonparametric survival analysis often led to shorter recency periods than analysis of sensitivity and specificity as a new method. These findings suggest that more data from seroconverters and other methodologies are needed to determine the recency period for estimating HIV incidence. -
Citations
Citations to this article as recorded by- Western Blot-Based Logistic Regression Model for the Identification of Recent HIV-1 Infection: A Promising HIV-1 Surveillance Approach for Resource-Limited Regions
Jiegang Huang, Minlian Wang, Chunyuan Huang, Bingyu Liang, Junjun Jiang, Chuanyi Ning, Ning Zang, Hui Chen, Jie Liu, Rongfeng Chen, Yanyan Liao, Li Ye, Hao Liang
BioMed Research International.2018; 2018: 1. CrossRef
- Western Blot-Based Logistic Regression Model for the Identification of Recent HIV-1 Infection: A Promising HIV-1 Surveillance Approach for Resource-Limited Regions
- Availability of Clean Tap Water and Medical Services Prevents the Incidence of Typhoid Fever
- Deog-Yong Lee, Esther Lee, HyeMin Park, SeongHan Kim
- Osong Public Health Res Perspect. 2013;4(2):68-71. Published online April 30, 2013
- DOI: https://doi.org/10.1016/j.phrp.2013.03.005
- 3,114 View
- 20 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objective:
In this study, the factors that induced a decrease in the incidence of typhoid fever were analyzed. Based on the study results, we propose a quantitative and concrete solution to reduce the incidence of typhoid fever.
Methods
We analyzed the incidence and fatality rate of typhoid fever in Korea. Tap water service rate and the number of pharmacies, which affect the incidence rate of typhoid fever, were used as environmental factors.
Results
To prevent typhoid fever in the community, it is necessary to provide clean tap water service to 35.5% of the population, with an individual requiring 173 L of clean water daily. Appropriate access to clean water (51% service coverage, 307 L) helped the population to maintain individual hygiene and food safety practices, which brought about a decrease in the incidence of typhoid fever, and subsequently a decrease in fatality rate, which was achieved twice. During the 8-year study period, the fatality rate decreased to 1% when the population has access to proper medical service.
Conclusion
The fatality rate was primarily affected by the availability of medical services as well as by the incidence of typhoid fever. However, an analysis of the study results showed that the incidence of typhoid fever was affected only by the availability of clean water through the tap water system. -
Citations
Citations to this article as recorded by- TIPICO X: report of the 10th interactive infectious disease workshop on infectious diseases and vaccines
Irene Rivero-Calle, Jose Gómez-Rial, Louis Bont, Bradford D. Gessner, Melvin Kohn, Ron Dagan, Daniel C. Payne, Laia Bruni, Andrew J. Pollard, Adolfo García-Sastre, Denise L. Faustman, Albert Osterhaus, Robb Butler, Francisco Giménez Sánchez, Francisco Álv
Human Vaccines & Immunotherapeutics.2021; 17(3): 759. CrossRef - Progress in the overall understanding of typhoid fever: implications for vaccine development
Peter J O’Reilly, Dikshya Pant, Mila Shakya, Buddha Basnyat, Andrew J Pollard
Expert Review of Vaccines.2020; 19(4): 367. CrossRef
- TIPICO X: report of the 10th interactive infectious disease workshop on infectious diseases and vaccines
- Are There Spatial and Temporal Correlations in the Incidence Distribution of Scrub Typhus in Korea?
- Maengseok Noh, Youngjo Lee, Chaeshin Chu, Jin Gwack, Seung-Ki Youn, Sun Huh
- Osong Public Health Res Perspect. 2013;4(1):39-44. Published online February 28, 2013
- DOI: https://doi.org/10.1016/j.phrp.2013.01.002
- 3,579 View
- 22 Download
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
A hierarchical generalized linear model (HGLM) was applied to estimate the transmission pattern of scrub typhus from 2001 to 2011 in the Republic of Korea, based on spatial and temporal correlation.
Methods
Based on the descriptive statistics of scrub typhus incidence from 2001 to 2011 reported to the Korean Centers for Disease Control and Prevention, the spatial and temporal correlations were estimated by HGLM. Incidences according to age, sex, and year were also estimated by the best-fit model out of nine HGLMs. A disease map was drawn to view the annual regional spread of the disease.
Results
The total number of scrub typhus cases reported from 2001 to 2011 was 51,136: male, 18,628 (36.4%); female, 32,508 (63.6%). The best-fit model selected was a combination of the spatial model (Markov random-field model) and temporal model (first order autoregressive model) of scrub typhus transmission. The peak incidence was 28.80 per 100,000 persons in early October and the peak incidence was 40.17 per 100,000 persons in those aged 63.3 years old by the best-fit HGLM. The disease map showed the spread of disease from the southern central area to a nationwide area, excepting Gangwon-do (province), Gyeongsangbuk-do (province), and Seoul.
Conclusion
In the transmission of scrub typhus in Korea, there was a correlation to the incidence of adjacent areas, as well as that of the previous year. According to the disease map, we are unlikely to see any decrease in the incidence in the near future, unless ongoing aggressive measures to prevent the exposure to the vector, chigger mites, in rural areas, are put into place. -
Citations
Citations to this article as recorded by- Prevalence of chigger mites and Orientia tsutsugamushi strains in northern regions of Gangwon-do, Korea
Soojin Kim, In Yong Lee, Sezim Monoldorova, Jiro Kim, Jang Hoon Seo, Tai-Soon Yong, Bo Young Jeon
Parasites, Hosts and Diseases.2023; 61(3): 263. CrossRef - Urine Metabolite of Mice with Orientia tsutsugamushi Infection
Sangho Choi, Do-Hwan Ahn, Min-Gyu Yoo, Hye-Ja Lee, Seong Beom Cho, Hee-Bin Park, Sung Soon Kim, Hyuk Chu
The American Journal of Tropical Medicine and Hygi.2023; 108(2): 296. CrossRef - Spatiotemporal dynamics and environmental determinants of scrub typhus in Anhui Province, China, 2010–2020
Xianyu Wei, Junyu He, Wenwu Yin, Ricardo J. Soares Magalhaes, Yanding Wang, Yuanyong Xu, Liang Wen, Yehuan Sun, Wenyi Zhang, Hailong Sun
Scientific Reports.2023;[Epub] CrossRef - Epidemiological characteristics of cases with scrub typhus and their correlation with chigger mite occurrence (2019–2021): A focus on case occupation and activity locations
Se‐Jin Jeong, Jin‐Hwan Jeon, Kyung won Hwang
Entomological Research.2023; 53(7): 247. CrossRef - Epidemiological characteristics and spatiotemporal patterns of scrub typhus in Yunnan Province from 2006 to 2017
Pei-Ying Peng, Lei Xu, Gu-Xian Wang, Wen-Yuan He, Ting-Liang Yan, Xian-Guo Guo
Scientific Reports.2022;[Epub] CrossRef - Clinical and Laboratory Predictors associated with Complicated Scrub Typhus
Mi-Hee Kim, Si-Hyun Kim, Jung-Hyun Choi, Seong-Heon Wie
Infection & Chemotherapy.2019; 51(2): 161. CrossRef - Awareness and Work-Related Factors Associated with Scrub Typhus: A Case-Control Study from South Korea
Dong-Seob Kim, Dilaram Acharya, Kwan Lee, Seok-Ju Yoo, Ji-Hyuk Park, Hyun-Sul Lim
International Journal of Environmental Research an.2018; 15(6): 1143. CrossRef - Estimating the burden of scrub typhus: A systematic review
Ana Bonell, Yoel Lubell, Paul N. Newton, John A. Crump, Daniel H. Paris, Janet Foley
PLOS Neglected Tropical Diseases.2017; 11(9): e0005838. CrossRef - Spatiotemporal Dynamics of Scrub Typhus Transmission in Mainland China, 2006-2014
Yi-Cheng Wu, Quan Qian, Ricardo J. Soares Magalhaes, Zhi-Hai Han, Wen-Biao Hu, Ubydul Haque, Thomas A. Weppelmann, Yong Wang, Yun-Xi Liu, Xin-Lou Li, Hai-Long Sun, Yan-Song Sun, Archie C. A. Clements, Shen-Long Li, Wen-Yi Zhang, Mathieu Picardeau
PLOS Neglected Tropical Diseases.2016; 10(8): e0004875. CrossRef - Larval Chigger Mites Collected from Small Mammals in 3 Provinces, Korea
In-Yong Lee, Hyeon-Je Song, Yeon-Joo Choi, Sun-Hye Shin, Min-Kyung Choi, So-Hyun Kwon, E-Hyun Shin, Chan Park, Heung-Chul Kim, Terry A. Klein, Kyung-Hee Park, Won-Jong Jang
The Korean Journal of Parasitology.2014; 52(2): 225. CrossRef
- Prevalence of chigger mites and Orientia tsutsugamushi strains in northern regions of Gangwon-do, Korea
Article
- Spatial and Temporal Distribution of
Plasmodium vivax Malaria in Korea Estimated with a Hierarchical Generalized Linear Model - Maengseok Noh, Youngjo Lee, Seungyoung Oh, Chaeshin Chu, Jin Gwack, Seung-Ki Youn, Shin Hyeong Cho, Won Ja Lee, Sun Huh
- Osong Public Health Res Perspect. 2012;3(4):192-198. Published online December 31, 2012
- DOI: https://doi.org/10.1016/j.phrp.2012.11.003
- 3,362 View
- 20 Download
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
The spatial and temporal correlations were estimated to determine Plasmodium vivax malarial transmission pattern in Korea from 2001–2011 with the hierarchical generalized linear model.
Methods
Malaria cases reported to the Korea Centers for Disease Control and Prevention from 2001 to 2011 were analyzed with descriptive statistics and the incidence was estimated according to age, sex, and year by the hierarchical generalized linear model. Spatial and temporal correlation was estimated and the best model was selected from nine models. Results were presented as diseases map according to age and sex.
Results
The incidence according to age was highest in the 20–25-year-old group (244.52 infections/100,000). Mean ages of infected males and females were 31.0 years and 45.3 years with incidences 7.8 infections/100,000 and 7.1 infections/100,000 after estimation. The mean month for infection was mid-July with incidence 10.4 infections/100,000. The best-fit model showed that there was a spatial and temporal correlation in the malarial transmission. Incidence was very low or negligible in areas distant from the demilitarized zone between Republic of Korea and Democratic People’s Republic of Korea (North Korea) if the 20–29-year-old male group was omitted in the diseases map.
Conclusion
Malarial transmission in a region in Korea was influenced by the incidence in adjacent regions in recent years. Since malaria in Korea mainly originates from mosquitoes from North Korea, there will be continuous decrease if there is no further outbreak in North Korea. -
Citations
Citations to this article as recorded by- Source separation in municipal solid waste management: Practical means to its success in Asian cities
Premakumara Jagath Dickella Gamaralalage, Sadhan Kumar Ghosh, Kazunobu Onogawa
Waste Management & Research: The Journal for a Sus.2022; 40(3): 360. CrossRef - Spatial connectivity in mosquito-borne disease models: a systematic review of methods and assumptions
Sophie A. Lee, Christopher I. Jarvis, W. John Edmunds, Theodoros Economou, Rachel Lowe
Journal of The Royal Society Interface.2021; 18(178): 20210096. CrossRef - Effects of climate change on Plasmodium vivax malaria transmission dynamics: A mathematical modeling approach
Jung Eun Kim, Yongin Choi, Chang Hyeong Lee
Applied Mathematics and Computation.2019; 347: 616. CrossRef - Spatially Filtered Multilevel Analysis on Spatial Determinants for Malaria Occurrence in Korea
Sehyeong Kim, Youngho Kim
International Journal of Environmental Research an.2019; 16(7): 1250. CrossRef - Is it necessary to take anthelmintics every year in Korea?
Sun Huh
Journal of the Korean Medical Association.2018; 61(3): 198. CrossRef - Research on Factors Influencing Municipal Household Solid Waste Separate Collection: Bayesian Belief Networks
Zhujie Chu, Wenna Wang, Bairong Wang, Jun Zhuang
Sustainability.2016; 8(2): 152. CrossRef - Chemotherapeutic drugs for common parasitic diseases in Korea
Sun Huh
Journal of the Korean Medical Association.2013; 56(6): 513. CrossRef - Are There Spatial and Temporal Correlations in the Incidence Distribution of Scrub Typhus in Korea?
Maengseok Noh, Youngjo Lee, Chaeshin Chu, Jin Gwack, Seung-Ki Youn, Sun Huh
Osong Public Health and Research Perspectives.2013; 4(1): 39. CrossRef - Years of Epidemics (2009–2011): Pandemic Influenza and Foot-and-Mouth Disease Epidemic in Korea
Hae-Wol Cho, Chaeshin Chu
Osong Public Health and Research Perspectives.2013; 4(3): 125. CrossRef - A New Statistical Approach to Analyze Plasmodium vivax Malaria Endemic in Korea
Hae-Wol Cho, Chaeshin Chu
Osong Public Health and Research Perspectives.2012; 3(4): 191. CrossRef
- Source separation in municipal solid waste management: Practical means to its success in Asian cities



 First
First Prev
Prev


