Search
- Page Path
- HOME > Search
- A case-control study of acute hepatitis A in South Korea, 2019
- Jung Hee Hyun, Ju Young Yoon, Sang Hyuk Lee
- Osong Public Health Res Perspect. 2022;13(5):352-359. Published online October 12, 2022
- DOI: https://doi.org/10.24171/j.phrp.2022.0141
- 2,909 View
- 117 Download
- 1 Web of Science
- 4 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 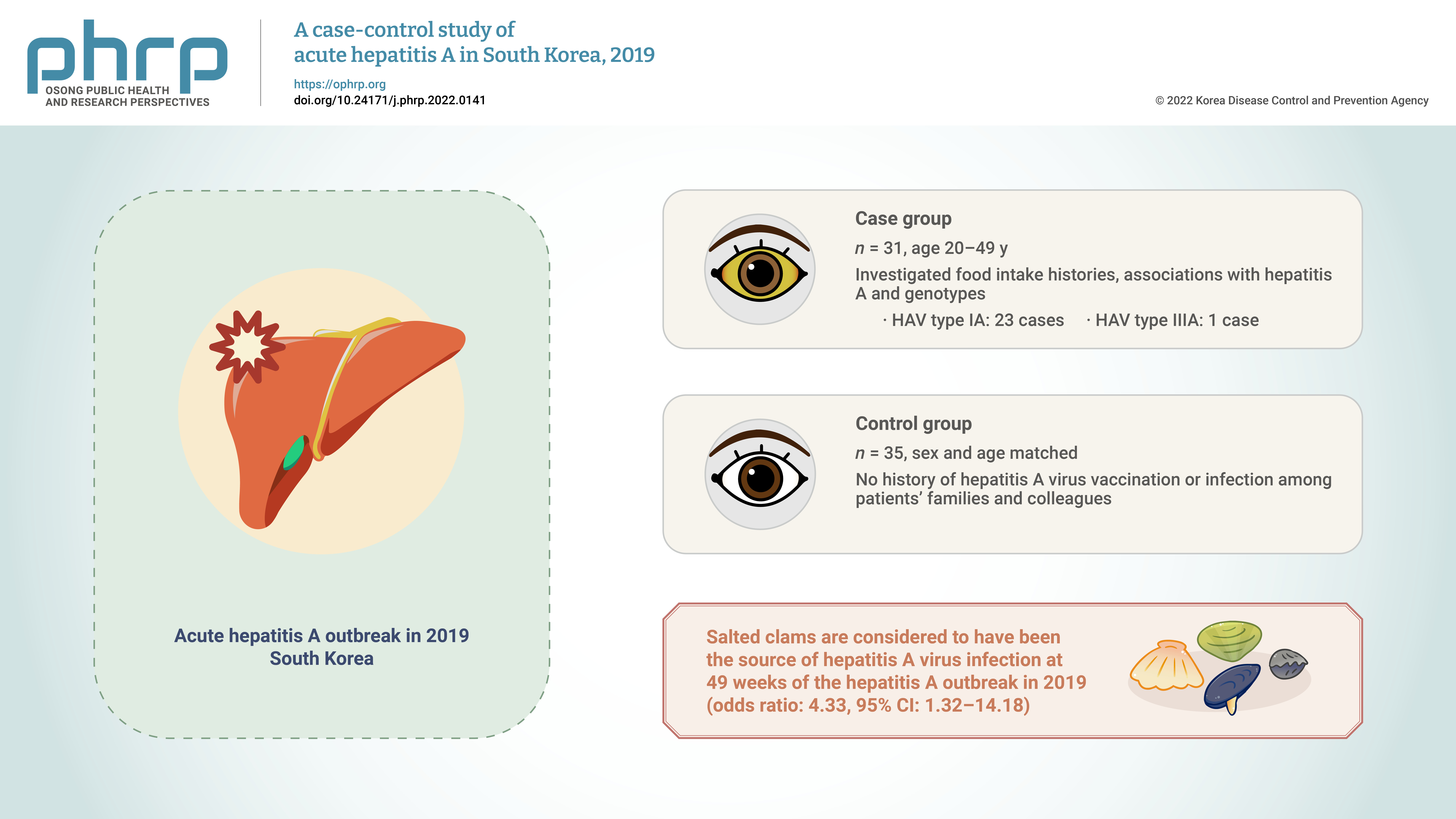
- Objectives
We aimed to reconfirm the source of hepatitis A virus (HAV) infection through epidemiological and genotype investigations of individual cases in a 2019 outbreak in South Korea. Methods: We investigated food intake histories, associations with hepatitis A, and genotypes of HAV in 31 patients with hepatitis aged 20 to 49 years registered in the integrated disease and health management system during December 1–7, 2019 (case group) and in 35 sex- and agematched people without a history of HAV vaccination or infection among patients’ families and colleagues (control group). Results: The consumption of salted clams was a significant factor (odds ratio, 4.33; 95% confidence interval, 1.32–14.18) in the risk factor analysis of food intake history. HAV genotypes were analyzed in 24 of 31 patients. Type IA and type IIIA were found in 23 and 1 cases, respectively. Conclusion: Salted clams are considered to have been the source of HAV infection at 49 weeks of the HAV outbreak in 2019; this result was consistent with that of a previous epidemiological investigation conducted by the Korea Disease Control and Prevention Agency in September 2019. Therefore, monitoring of the production and distribution of salted clams needs to be continued. -
Citations
Citations to this article as recorded by- Monitoring viruses and beta-lactam resistance genes through wastewater surveillance during a COVID-19 surge in Suwon, South Korea
Rajendra Singh, Jaewon Ryu, Sung Soo Park, Sungpyo Kim, Keugtae Kim
Science of The Total Environment.2024; 922: 171223. CrossRef - Prevalence of foodborne viruses and influenza A virus from poultry processing plants to retailed chickens
Daseul Yeo, Mengxiao Song, Md. Iqbal Hossain, Soontag Jung, Zhaoqi Wang, Dong Joo Seo, Min Suk Rhee, Changsun Choi
Frontiers in Sustainable Food Systems.2023;[Epub] CrossRef - A Study on the Detection Rate of Hepatitis A from Gastroenteritis Patients and the Genotype Analysis of Hepatitis A Virus in Busan
Sun Hee Park, Chanhee Kim, Summi Lee, Jihye Jeong, Junghye Choi, Seung Ju Lee
Journal of Bacteriology and Virology.2023; 53(2): 74. CrossRef - A Study on the Detection Rate of Hepatitis A from Gastroenteritis Patients and the Genotype Analysis of Hepatitis A Virus in Busan
Sun Hee Park, Chanhee Kim, Summi Lee, Jihye Jeong, Junghye Choi, Seung Ju Lee
Journal of Bacteriology and Virology.2023; 53(2): 74. CrossRef
- Monitoring viruses and beta-lactam resistance genes through wastewater surveillance during a COVID-19 surge in Suwon, South Korea
- Behavioral therapy and pharmacotherapy for relapse prevention in abstinent smokers: a rapid review and meta-analysis for the Korea Preventive Service Task Force
- Naae Lee, Eon Sook Lee, Jae Moon Yun, Cheol Min Lee, Seung-Won Oh, Younglee Choi, Belong Cho
- Osong Public Health Res Perspect. 2021;12(4):244-253. Published online July 6, 2021
- DOI: https://doi.org/10.24171/j.phrp.2021.0017
- 5,956 View
- 94 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Objectives
This study aimed to assess the effectiveness of relapse prevention interventions involving behavioral and pharmacological treatment among abstinent smokers.
Methods
This rapid review was conducted using MEDLINE, Cochrane CENTRAL, CINAHL, Embase, KMbase, and KoreaMed to identify studies published until June 20, 2020. The participants were abstinent smokers who quit smoking on their own, due to pregnancy, hospitalization, or by participating in a smoking cessation program. We found a systematic review that fit the objective of this study and included 81 randomized controlled trials (RCTs). Studies that did not present information on smoking cessation status, had no control group, or used reward-based interventions were excluded. Random effect and fixed effect meta-analyses were used to estimate the relative risk (RR) and 95% confidence interval (CI). In subgroup analyses, differences between subgroups were verified based on the participant setting, characteristics, intervention type, and intensity.
Results
Following screening, 44 RCTs were included in the meta-analysis. The review reported no differences in the success rate of relapse prevention between the behavioral interventions. Pharmacotherapy interventions showed higher success rates (RR, 1.15; 95% CI, 1.05−1.26; I2=40.71%), depending on prior abstinence duration and the drug type. Conclusions: The results indicated that pharmacotherapy has a significant effect on preventing relapse among abstinent smokers. -
Citations
Citations to this article as recorded by- A Survey of the Clinical Practice of Korean Medicine for Smoking Cessation in Public Health Centers: A Web-Based Survey of Public Health Doctors of Korean Medicine
Gyoungeun Park, Jeong-Hyun Moon, Eun-Jung Kim, Byung-Kwan Seo, Yong-Hyeon Baek, Won-Suk Sung
Perspectives on Integrative Medicine.2024; 3(1): 45. CrossRef
- A Survey of the Clinical Practice of Korean Medicine for Smoking Cessation in Public Health Centers: A Web-Based Survey of Public Health Doctors of Korean Medicine
- Designing and Evaluating Educational Intervention to Improve Preventive Behavior Against Cutaneous Leishmaniasis in Endemic Areas in Iran
- Musalreza Ghodsi, Mina Maheri, Hamid Joveini, Mohammad Hassan Rakhshani, Ali Mehri
- Osong Public Health Res Perspect. 2019;10(4):253-262. Published online August 31, 2019
- DOI: https://doi.org/10.24171/j.phrp.2019.10.4.09
- 8,815 View
- 109 Download
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF Objectives Health education programs are one of the most important strategies for controlling cutaneous leishmaniasis (CL) in endemic areas such as Neshabur city. This study aimed to develop and evaluate a comprehensive health education program to improve preventive behaviors for CL.
Methods This was an interventional study conducted on 136 high school students in Neishabur city. Data collection instruments included a demographic questionnaire and a researcher-made questionnaire based on the “Health Belief Model” and “Beliefs, Attitudes, Subjective Norms and Enabling Factors Model” constructs. The control and intervention groups completed the questionnaires before and 2 months after the intervention. The intervention was conducted in 6, 1-hour educational sessions for the intervention group students and 2, 1-hour sessions for school administrators, teachers, and students’ parents.
Results There was no significant difference between the 2 groups in the pre-intervention phase. However, in the post-intervention phase, there were significant differences between the 2 groups for mean scores of knowledge, perceived susceptibility, perceived severity, perceived benefits, cues to action, self-efficacy, attitude, subjective norms, behavioral intention, enabling factors, and behavior associated with CL.
Conclusion Health education program based on the “Health Belief Model” and the “Beliefs, Attitudes, Subjective Norms and Enabling Factors Model” model constructs may be a comprehensive and effective educational program to improve preventive behaviors against CL in students.
-
Citations
Citations to this article as recorded by- Antiparasitic activity of the iron-containing milk protein lactoferrin and its potential derivatives against human intestinal and blood parasites
Namrata Anand
Frontiers in Parasitology.2024;[Epub] CrossRef - Cutaneous leishmaniasis situation analysis in the Islamic Republic of Iran in preparation for an elimination plan
Iraj Sharifi, Ahmad Khosravi, Mohammad Reza Aflatoonian, Ehsan Salarkia, Mehdi Bamorovat, Ali Karamoozian, Mahmoud Nekoei Moghadam, Fatemeh Sharifi, Abbas Aghaei Afshar, Setareh Agha Kuchak Afshari, Faranak Gharachorloo, Mohammad Reza Shirzadi, Behzad Ami
Frontiers in Public Health.2023;[Epub] CrossRef - Mutual Role of Patients and the Healthcare System in the Control of Cutaneous Leishmaniasis
Mehdi Bamorovat, Iraj Sharifi, Setareh Agha Kuchak Afshari, Pooya Ghasemi Nejad Almani, Fedor Korennoy
Transboundary and Emerging Diseases.2023; 2023: 1. CrossRef - Knowledge, perceptions and practices of health students and professionals regarding leishmaniasis in Portugal: a cross-sectional study
Rafael Rocha, Cláudia Conceição, Luzia Gonçalves, Carla Maia
Parasites & Vectors.2023;[Epub] CrossRef - Investigating Iranians’ Attitude, Practice, and Perceived Self-Efficacy towards COVID-19 Preventive Behaviors
Hamid Joveini, Zahra Zare, Masoumeh Hashemian, Ali Mehri, Reza Shahrabadi, Neda Mahdavifar, Hamideh Ebrahimi Aval
The Open Public Health Journal.2022;[Epub] CrossRef - Şark çıbanı vakalarında bilgi ve farkındalık düzeyini artırmaya yönelik müdahale çalışması: Şanlıurfa örneği
Burcu BEYAZGÜL, İbrahim KORUK, Rüstem KUZAN, Şule ALLAHVERDİ
Mersin Üniversitesi Sağlık Bilimleri Dergisi.2022; 15(2): 188. CrossRef - Congregational Worshiping and Implementation of the COVID-19 Preventive Behavioral Measures During the Re-opening Phase of Worship Places Among Indonesian Muslims
Mochamad Iqbal Nurmansyah, Sarah Handayani, Deni Wahyudi Kurniawan, Emma Rachmawati, Hidayati, Ahmad Muttaqin Alim
Journal of Religion and Health.2022; 61(5): 4169. CrossRef - Development and psychometric assessment of cutaneous leishmaniasis prevention behaviors questionnaire in adolescent female students: Application of integration of cultural model and extended parallel process model
Masoumeh Alidosti, Hossein Shahnazi, Zahra Heidari, Fereshteh Zamani-Alavijeh, Mona Dür
PLOS ONE.2022; 17(8): e0273400. CrossRef - Community-Based Interventions for the Prevention and Control of Cutaneous Leishmaniasis: A Systematic Review
Kay Polidano, Brianne Wenning, Alejandra Ruiz-Cadavid, Baheya Dawaishan, Jay Panchal, Sonali Gunasekara, Haftom Abebe, Marciglei Morais, Helen Price, Lisa Dikomitis
Social Sciences.2022; 11(10): 490. CrossRef - Design and evaluation of two educational media in the form of animation and games to promote the cutaneous leishmaniasis prevention behaviors in adolescent female
Masoumeh Alidosti, Hossein Shahnazi, Zahra Heidari, Fereshteh Zamani-Alavijeh
BMC Public Health.2022;[Epub] CrossRef - Knowledge, attitude, and practice toward Zika virus among staff of comprehensive health services centers affiliated with Tehran University of Medical Sciences in 2020
Hamidreza Farrokh‐Eslamlou, Mina Maheri
Journal of Obstetrics and Gynaecology Research.2021; 47(6): 2204. CrossRef - Behaviors and Perceptions Related to Cutaneous Leishmaniasis in Endemic Areas of the World: A Review
Masoumeh Alidosti, Zahra Heidari, Hossein Shahnazi, Fereshteh Zamani-Alavijeh
Acta Tropica.2021; 223: 106090. CrossRef - Application of BASNEF model in students training regarding cutaneous leishmaniasis prevention behaviors: a school-based quasi experimental study
Gholamreza Alizadeh, Hossein Shahnazi, Akbar Hassanzadeh
BMC Infectious Diseases.2021;[Epub] CrossRef - Predicting the Preventive Behaviors of Cutaneous Leishmaniasis in families with Children Under 10 Years, Applied the Precede Model
Hosein Jajarmi, Mahdi Gholian-Aval, Asma pourtaheri, Habibollah Esmaily, Hamid Hosseini, Rezvan Rajabzadeh, Hadi Tehrani
ranian Journal of Health Education and Health Prom.2021; 9(4): 360. CrossRef - Effects of an Educational Intervention on Male Students’ Intention to Quit Water Pipe Smoking: an Application of the Theory of Planned Behavior (TPB) and Health Action Process Approach (HAPA)
Hamid Joveini, Tahereh Dehdari, Masoumeh Hashemian, Mina Maheri, Reza Shahrabadi, Alireza Rohban, Ali Mehri, Hasan Eftekhar Ardebili
Journal of Education and Community Health.2020; 7(2): 73. CrossRef
- Antiparasitic activity of the iron-containing milk protein lactoferrin and its potential derivatives against human intestinal and blood parasites
- Army Soldiers’ Knowledge of, Attitude Towards, and Preventive Behavior Towards Tuberculosis in Korea
- Yun Choi, Geum Hee Jeong
- Osong Public Health Res Perspect. 2018;9(5):269-277. Published online October 31, 2018
- DOI: https://doi.org/10.24171/j.phrp.2018.9.5.09
- 6,348 View
- 150 Download
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF Objectives The aim of this study was to gather information about Korean Army soldiers’ attitude towards tuberculosis to enable the development of an informed educational program and potential intervention plans.
Methods There were 500 male soldiers serving in the Korean Army who responded to questionnaires regarding knowledge of, attitudes towards, and preventive behavior towards tuberculosis. The questionnaires were collected between September 10 until October 1, 2014. Participants’ characteristic that influenced differences in knowledge, attitudes, and preventive behavior towards tuberculosis were compared by
t test. Variables that influenced preventive behavior were identified by multiple regression analysis.Results The mean scores assessing knowledge of, attitude, and preventive behavior towards tuberculosis were 11.64 (± 4.03) out of 20 points, 3.21 (± 0.38) out of 4 points, and 2.88 (± 0.42) out of 4 points, respectively. Non-smokers were more knowledgeable about tuberculosis than smokers. Participants who had family or friends with tuberculosis had better knowledge and a more productive attitude to tuberculosis. Participants who were educated or obtained information about tuberculosis, received better scores in all areas of knowledge, attitude and preventive behavior compared to other participants. Non-smoking, family or friends who have had tuberculosis, obtaining information about tuberculosis, and positive attitudes towards treatment and preventive education had an explanatory power of 24.6% with regard to preventive behavior against tuberculosis.
Conclusion More relatable, systemized education should be provided regularly to improve soldiers’ knowledge of, attitudes towards, and prevention against tuberculosis in the Republic of Korea Army.
-
Citations
Citations to this article as recorded by- Tingkat Pengetahuan Keluarga Tinggal Serumah Tentang Pencegahan Penularan Pasien Tuberkulosis Paru
Komang Yuliani, I Dewa Agung Ketut Sudarsana
Journal Nursing Research Publication Media (NURSEP.2023; 2(1): 47. CrossRef - Knowledge, Attitudes, and Preventative Behavior Toward Tuberculosis in University Students in Indonesia
Irma Melyani Puspitasari, Rano Kurnia Sinuraya, Arini Nurhaqiqi Aminudin, Rika Rahmi Kamilah
Infection and Drug Resistance.2022; Volume 15: 4721. CrossRef - The Relationship between Health Literacy and Preventive Behaviors of Soldiers
Javad Azimzadeh, Maryam Nezamzadeh, Fatemeh Kalroozi, Seyyed Amir Hossein Pishgooie
Military Caring Sciences.2021; 8(2): 109. CrossRef - Factors Affecting Preventive Behavior related to Tuberculosis among University Students in Korea: Focused on Knowledge, Attitude and Optimistic Bias related to Tuberculosis
Myung Soon Kwon, Yun Choi
Journal of Korean Academy of Fundamentals of Nursi.2020; 27(3): 236. CrossRef - Assessment of knowledge, attitude and practice on tuberculosis among teacher trainees of Samtse College of Education, Bhutan
Thinley Dorji, Tandin Tshering, Kinley Wangdi, Ritesh G. Menezes
PLOS ONE.2020; 15(11): e0241923. CrossRef - The Infectivity of Pulmonary Tuberculosis in Korean Army Units: Evidence from Outbreak Investigations
Chang-gyo Yoon, Dong Yoon Kang, Jaehun Jung, Soo Yon Oh, Jin Beom Lee, Mi-Hyun Kim, Younsuk Seo, Hee-Jin Kim
Tuberculosis and Respiratory Diseases.2019; 82(4): 298. CrossRef
- Tingkat Pengetahuan Keluarga Tinggal Serumah Tentang Pencegahan Penularan Pasien Tuberkulosis Paru
- Factors Affecting Smoking Cessation Success of Heavy Smokers Registered in the Intensive Care Smoking Cessation Camp (Data from the National Tobacco Control Center)
- Hansol Yeom, Hee-Sook Lim, Jihyun Min, Seoni Lee, Yoon-Hyung Park
- Osong Public Health Res Perspect. 2018;9(5):240-247. Published online October 31, 2018
- DOI: https://doi.org/10.24171/j.phrp.2018.9.5.05
- 8,942 View
- 125 Download
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF Objectives The purpose of this study was to investigate the factors involved in the success of smoking cessation in heavy smokers enrolled in an intensive care smoking cessation camp program.
Methods Heavy smokers enrolled in the program were classified into a success (
n = 69) or failure (n = 29) group, according to whether they maintained smoking cessation for 6 months after the end of the program. Demographics, smoking behaviors, and smoking cessation-related characteristics were analyzed.Results Statistically significantly more participants in the success group had a spouse (98.6%;
p = 0.008) compared with participants in the failure group (82.8%). However, multivariate logistic regression analysis indicated that having a spouse was not an independent factor in smoking cessation (p = 0.349). A significant difference in the frequency of counseling between the success and failure groups was observed (p = 0.001), with 72.5% of those who received counseling on 3–5 occasions for 6 months after the end of program successfully quit smoking, indicating that those who received more counseling had a higher likelihood of smoking cessation success. This was confirmed as an independent factor by multivariate logistic regression (p < 0.005). Furthermore, a graduate school level of education or higher, indicated a statistically greater success rate compared to those that were less well educated (p = 0.043). This was also observed as a significant independent factor using multivariate logistic regression (p = 0.046).Conclusion Education level, marital status, and the number of counseling sessions were significant factors contributing to smoking cessation success.
-
Citations
Citations to this article as recorded by- Evaluation of Smoking Cessation Intervention Effectiveness in Smoking Cessation Clinics — China, 2019–2021
Li Xie, Yongfu Yan, Yan Yang, Yi Nan, Lin Xiao
China CDC Weekly.2023; 5(21): 469. CrossRef - Factors Associated with Smokers Attending More Than One Smoking Cessation Clinic Visit
Oh Beom Kwon, Chihoon Jung, Auk Kim, Gihwan Byeon, Seung-Joon Lee, Woo Jin Kim
Journal of Clinical Medicine.2023; 12(23): 7222. CrossRef - Effects of a supportive workplace environment on the success rate for smoking cessation camp
Woojin Kim, A Ram Kim, Minsu Ock, Young-Jee Jeon, Heun Lee, Daehwan Kim, Minjun Kim, Cheolin Yoo
Annals of Occupational and Environmental Medicine.2023;[Epub] CrossRef - Sigara Bırakma Polikliniğine Başvuran Bireylerde Tedavi Başarısını Etkileyen Faktörler
Derya KOCAKAYA, Hatice ŞENOL, Sezer ASLAN, Ahmed Mahmud ÇIRAKOĞLU, Merve ÇAKIR, Hatice TELCİ, Mehmet ÇETİNKAYA, Sehnaz OLGUN, Ayşe Nilüfer ÖZAYDIN, Ceyhan BERRİN
Bağımlılık Dergisi.2022; 23(1): 69. CrossRef - Smoking cessation rates in elderly and nonelderly smokers after participating in an intensive care smoking cessation camp
Jae-Kyeong Lee, Yu-Il Kim, Sun-Seog Kweon, In-Jae Oh, Yong-Soo Kwon, Hong-Joon Shin, Yu-Ri Choe, Ha-Young Park, Young-Ok Na, Hwa-Kyung Park
Medicine.2022; 101(30): e29886. CrossRef - Patterns and predictors of smoking relapse among inpatient smoking intervention participants: a 1-year follow-up study in Korea
Seung Eun Lee, Chul-Woung Kim, Hyo-Bin Im, Myungwha Jang
Epidemiology and Health.2021; 43: e2021043. CrossRef - Factors affecting smoking initiation and cessation among
adult smokers in Fiji: A qualitative study
Masoud Mohammadnezhad, Mondha Kengganpanich
Tobacco Induced Diseases.2021; 19(December): 1. CrossRef - “STOP the PUFF! Tayo’y mag bagong BAGA, SIGARILYO ay ITIGIL”: A Pilot Community-based Tobacco Intervention Project in an Urban Settlement
Irene Salve D Joson-Vergara, Julie T Li-Yu
Journal of Medicine, University of Santo Tomas.2021; 5(1): 586. CrossRef - Smoking cessation correlates with a decrease in infection rates following total joint arthroplasty
Christina Herrero, Alex Tang, Amy Wasterlain, Scott Sherman, Joseph Bosco, Claudette Lajam, Ran Schwarzkopf, James Slover
Journal of Orthopaedics.2020; 21: 390. CrossRef
- Evaluation of Smoking Cessation Intervention Effectiveness in Smoking Cessation Clinics — China, 2019–2021
- Effects of Anti-Smoking Public Service Announcements on the Attitudes of Korean College Students toward Smoking
- Kyoung Won Cho, Jakyoung Lee, Ji-hye Ryu, Soo Jeong Kim
- Osong Public Health Res Perspect. 2017;8(6):397-404. Published online December 31, 2017
- DOI: https://doi.org/10.24171/j.phrp.2017.8.6.07
- 4,255 View
- 44 Download
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material Objectives This study aimed to identify the effects of anti-smoking public service announcements on the attitudes of Korean college students toward smoking.
Methods This study involved students via convenience sampling from seven universities who were randomly assigned to four groups. All groups completed a preliminary questionnaire, before being shown a public service announcement twice, and then completed a post viewing questionnaire.
Results For announcements with positive messages, the proportion of changes in beliefs and attitudes were 39.1% and 19.8%, respectively, whereas those with negative messages showed a greater proportion of changes in the beliefs (59.7%) and attitudes (40.3%). After adjusting for sex and change in belief, the message types and smoking status were identified as factors affecting the change in the participants attitudes. A negative message resulted in a greater change in attitudes (odds ratio [OR], 3.047; 95% confidence interval [CI], 1.847–5.053). Ever-smokers including current smokers showed a greater positive change in attitude than never-smokers (OR, 6.965; 95% CI, 4.107–11.812).
Conclusion This study found that positive anti-smoking public service announcements were more effective on attitude change than negative messages. Additionally these announcements were more effective among viewers who were current smokers or had a prior smoking experience.
-
Citations
Citations to this article as recorded by- Association between Community Violence, Disorder and School Environment with Bullying among School Adolescents in Sao Paulo – Brazil
Catarina Machado Azeredo, Emanuele Souza Marques, Letícia Martins Okada, Maria Fernanda Tourinho Peres
Journal of Interpersonal Violence.2023; 38(3-4): 2432. CrossRef - Public service announcements: A literature review and way forward
Bharadhwaj Sivakumaran, Harindranath R. M., Nachiketas Nandakumar, Ekta Srivastava
International Journal of Consumer Studies.2023; 47(6): 2451. CrossRef - Encouraging Firework Safety Through Public Service Announcements
Stefano Cardin, Rachel Faber, Daniel Miller, Mary Elizabeth Gibson, Brett Lewellyn
The Journal of Hand Surgery.2022; 47(6): 574. CrossRef - Maintenance of Tobacco Abstinence—Effect of Anti-Tobacco Propaganda (Media) Messages
Laxmi Kumari, Meenakshi Sood, Sandhya Gupta
Pertanika Journal of Social Sciences and Humanitie.2022;[Epub] CrossRef - Interaction Between Smoking Cigarettes and Alcohol Consumption on Sexual Experience in High School Students
Soo Jeong Kim, Kyoung Won Cho
Osong Public Health and Research Perspectives.2019; 10(5): 274. CrossRef
- Association between Community Violence, Disorder and School Environment with Bullying among School Adolescents in Sao Paulo – Brazil
- Activities of the Korean Institute of Tuberculosis
- Sungweon Ryoo, Hee Jin Kim
- Osong Public Health Res Perspect. 2014;5(Suppl):S43-S49. Published online December 31, 2014
- DOI: https://doi.org/10.1016/j.phrp.2014.10.007
- 2,954 View
- 21 Download
- 18 Crossref
-
 Abstract
Abstract
 PDF
PDF - The Korean National Tuberculosis Association (KNTA) set up the Korean Institute of Tuberculosis (KIT) in 1970 to foster research and technical activities pertaining to tuberculosis (TB). The KNTA/KIT had successfully conducted a countrywide TB prevalence survey from 1965 to 1995 at 5-year intervals. The survey results (decline in TB rates) established Korea as a country that had successfully implemented national control programs for TB. The KIT developed the Korea Tuberculosis Surveillance System and the Laboratory Management Information System, both of which were transferred to the Korea Centers for Disease Control and Prevention after its establishment. The KIT functions as a central and supranational reference TB laboratory for microbiological and epidemiological research and provides training and education for health-care workers and medical practitioners. Recently, the KIT has expanded its activities to countries such as Ethiopia, Laos, and Timor-Leste to support TB control and prevention. The KIT will continue to support research activities and provide technical assistance in diagnosing the infection until it is completely eliminated in Korea.
-
Citations
Citations to this article as recorded by- A Review of Recent Advances in Deep Learning Models for Chest Disease Detection Using Radiography
Adnane Ait Nasser, Moulay A. Akhloufi
Diagnostics.2023; 13(1): 159. CrossRef - AI-based radiodiagnosis using chest X-rays: A review
Yasmeena Akhter, Richa Singh, Mayank Vatsa
Frontiers in Big Data.2023;[Epub] CrossRef - Deep Learning for Pneumonia Classification in Chest Radiography Images using Wavelet Transform
Amal Azeroual, Benayad Nsiri, Taoufiq Belhoussine Drissi, Amine El Ammari, Abdessamad Charrafi, Ittimade Nassar, Brahim Benaji
WSEAS TRANSACTIONS ON INFORMATION SCIENCE AND APPL.2023; 20: 245. CrossRef - The response to COVID-19 in Timor-Leste: lessons learnt
Joshua R Francis, Rui Maria de Araujo, Odete da Silva Viegas, Sergio Lobo, Danina Coelho, Arvind Mathur, Vinay Bothra, Dongbao Yu, Anthony D K Draper, Jennifer Yan, Nelson Martins
BMJ Global Health.2023; 8(10): e013573. CrossRef - Review on Pneumonia Image Detection: A Machine Learning Approach
Amer Kareem, Haiming Liu, Paul Sant
Human-Centric Intelligent Systems.2022; 2(1-2): 31. CrossRef - Database and AI Diagnostic Tools Improve Understanding of Lung Damage, Correlation of Pulmonary Disease and Brain Damage in COVID-19
Ilona Karpiel, Ana Starcevic, Mirella Urzeniczok
Sensors.2022; 22(16): 6312. CrossRef - MS-CheXNet: An Explainable and Lightweight Multi-Scale Dilated Network with Depthwise Separable Convolution for Prediction of Pulmonary Abnormalities in Chest Radiographs
Shashank Shetty, Ananthanarayana V S., Ajit Mahale
Mathematics.2022; 10(19): 3646. CrossRef - An incremental learning approach to automatically recognize pulmonary diseases from the multi-vendor chest radiographs
Mehreen Sirshar, Taimur Hassan, Muhammad Usman Akram, Shoab Ahmed Khan
Computers in Biology and Medicine.2021; 134: 104435. CrossRef - Deep learning applied to automatic disease detection using chest X‐rays
Daniel A. Moses
Journal of Medical Imaging and Radiation Oncology.2021; 65(5): 498. CrossRef - Intelligent Pneumonia Identification From Chest X-Rays: A Systematic Literature Review
Wasif Khan, Nazar Zaki, Luqman Ali
IEEE Access.2021; 9: 51747. CrossRef - Incidence rate of active tuberculosis in solid organ transplant recipients: Data from a nationwide population cohort in a high‐endemic country
Da Eun Kwon, Sang Hoon Han, Kyung Do Han, Yeonju La, Kyoung Hwa Lee
Transplant Infectious Disease.2021;[Epub] CrossRef - Deep learning, reusable and problem-based architectures for detection of consolidation on chest X-ray images
Hamed Behzadi-khormouji, Habib Rostami, Sana Salehi, Touba Derakhshande-Rishehri, Marzieh Masoumi, Siavash Salemi, Ahmad Keshavarz, Ali Gholamrezanezhad, Majid Assadi, Ali Batouli
Computer Methods and Programs in Biomedicine.2020; 185: 105162. CrossRef - Deep learning applications in pulmonary medical imaging: recent updates and insights on COVID-19
Hanan Farhat, George E. Sakr, Rima Kilany
Machine Vision and Applications.2020;[Epub] CrossRef - PadChest: A large chest x-ray image dataset with multi-label annotated reports
Aurelia Bustos, Antonio Pertusa, Jose-Maria Salinas, Maria de la Iglesia-Vayá
Medical Image Analysis.2020; 66: 101797. CrossRef - Utilizing Knowledge Distillation in Deep Learning for Classification of Chest X-Ray Abnormalities
Thi Kieu Khanh Ho, Jeonghwan Gwak
IEEE Access.2020; 8: 160749. CrossRef - Computer-aided detection in chest radiography based on artificial intelligence: a survey
Chunli Qin, Demin Yao, Yonghong Shi, Zhijian Song
BioMedical Engineering OnLine.2018;[Epub] CrossRef - The Relationship between Illness Perception and Health Behaviors among Patients with Tuberculosis: Mediating Effects of Self-efficacy and Family Support
Hye-jin Kim, Myung Kyung Lee
Korean Journal of Adult Nursing.2017; 29(6): 626. CrossRef - Is Tuberculosis Still the Number One Infectious Disease in Korea?
Hae-Wol Cho, Chaeshin Chu
Osong Public Health and Research Perspectives.2014; 5: S1. CrossRef
- A Review of Recent Advances in Deep Learning Models for Chest Disease Detection Using Radiography
- Incubation Period of Ebola Hemorrhagic Virus Subtype Zaire
- Martin Eichner, Scott F. Dowell, Nina Firese
- Osong Public Health Res Perspect. 2011;2(1):3-7. Published online June 30, 2011
- DOI: https://doi.org/10.1016/j.phrp.2011.04.001
- 4,138 View
- 16 Download
- 46 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
Ebola hemorrhagic fever has killed over 1300 people, mostly in equatorial Africa. There is still uncertainty about the natural reservoir of the virus and about some of the factors involved in disease transmission. Until now, a maximum incubation period of 21 days has been assumed.
Methods
We analyzed data collected during the Ebola outbreak (subtype Zaire) in Kikwit, Democratic Republic of the Congo, in 1995 using maximum likelihood inference and assuming a log-normally distributed incubation period.
Results
The mean incubation period was estimated to be 12.7 days (standard deviation 4.31 days), indicating that about 4.1% of patients may have incubation periods longer than 21 days.
Conclusion
If the risk of new cases is to be reduced to 1% then 25 days should be used when investigating the source of an outbreak, when determining the duration of surveillance for contacts, and when declaring the end of an outbreak. -
Citations
Citations to this article as recorded by- Prevention and post-exposure management of occupational exposure to Ebola virus
Michael A Moso, Chuan K Lim, Eloise Williams, Caroline Marshall, James McCarthy, Deborah A Williamson
The Lancet Infectious Diseases.2024; 24(2): e93. CrossRef - Systems immunology of transcriptional responses to viral infection identifies conserved antiviral pathways across macaques and humans
Kalani Ratnasiri, Hong Zheng, Jiaying Toh, Zhiyuan Yao, Veronica Duran, Michele Donato, Mario Roederer, Megha Kamath, John-Paul M. Todd, Matthew Gagne, Kathryn E. Foulds, Joseph R. Francica, Kizzmekia S. Corbett, Daniel C. Douek, Robert A. Seder, Shirit E
Cell Reports.2024; 43(2): 113706. CrossRef - Isothermal nucleic acid amplification technology for rapid detection of virus
Zhenting Wei, Xiaowen Wang, Huhu Feng, Fanpu Ji, Dan Bai, Xiaoping Dong, Wei Huang
Critical Reviews in Biotechnology.2023; 43(3): 415. CrossRef - Predicting the combined effects of case isolation, safe funeral practices, and contact tracing during Ebola virus disease outbreaks
Aliou Bouba, Kristina Barbara Helle, Kristan Alexander Schneider, Jan Rychtář
PLOS ONE.2023; 18(1): e0276351. CrossRef - Stability analysis of an SIR epidemic model with homestead-isolation on the susceptible and infectious, immunity, relapse and general incidence rate
Amine Bernoussi
International Journal of Biomathematics.2023;[Epub] CrossRef - Path analysis method in an epidemic model and stability analysis
Yong Zhou, Yiming Ding, Minrui Guo
Frontiers in Physics.2023;[Epub] CrossRef - Tradeoff between speed and reproductive number in pathogen evolution
Andreas Eilersen, Bjarke Frost Nielsen, Kim Sneppen
Physical Review Research.2023;[Epub] CrossRef - A Reinforcement Learning Based Decision Support Tool for Epidemic Control: Validation Study for COVID-19
Mohamed-Amine Chadi, Hajar Mousannif
Applied Artificial Intelligence.2022;[Epub] CrossRef - Spatially-heterogeneous embedded stochastic SEIR models for the 2014–2016 Ebola outbreak in West Africa
Kaitlyn Martinez, Grant Brown, Stephen Pankavich
Spatial and Spatio-temporal Epidemiology.2022; 41: 100505. CrossRef - Staff Scheduling During a Pandemic: The Case of Radiation Therapy Department
Hossein Abouee Mehrizi, Arian Aminoleslami, Johnson Darko, Ernest Osei, Houra Mahmoudzadeh
SSRN Electronic Journal .2022;[Epub] CrossRef - Review of Ebola virus disease in children – how far have we come?
Devika Dixit, Kasereka Masumbuko Claude, Lindsey Kjaldgaard, Michael T. Hawkes
Paediatrics and International Child Health.2021; 41(1): 12. CrossRef - Multi-population stochastic modeling of Ebola in Sierra Leone: Investigation of spatial heterogeneity
Rachid Muleia, Marc Aerts, Christel Faes, Maria Vittoria Barbarossa
PLOS ONE.2021; 16(5): e0250765. CrossRef - Detecting Pathogen Exposure During the Non-symptomatic Incubation Period Using Physiological Data: Proof of Concept in Non-human Primates
Shakti Davis, Lauren Milechin, Tejash Patel, Mark Hernandez, Greg Ciccarelli, Siddharth Samsi, Lisa Hensley, Arthur Goff, John Trefry, Sara Johnston, Bret Purcell, Catherine Cabrera, Jack Fleischman, Albert Reuther, Kajal Claypool, Franco Rossi, Anna Honk
Frontiers in Physiology.2021;[Epub] CrossRef - Advances and insights in the diagnosis of viral infections
Julija Dronina, Urte Samukaite-Bubniene, Arunas Ramanavicius
Journal of Nanobiotechnology.2021;[Epub] CrossRef - Treatment of Ebola-related critical illness
Peter Kiiza, S. Mullin, K. Teo, N. K. J. Adhikari, R. A. Fowler
Intensive Care Medicine.2020; 46(2): 285. CrossRef - AAV Vectored Immunoprophylaxis for Filovirus Infections
Amira D. Rghei, Laura P. van Lieshout, Lisa A. Santry, Matthew M. Guilleman, Sylvia P. Thomas, Leonardo Susta, Khalil Karimi, Byram W. Bridle, Sarah K. Wootton
Tropical Medicine and Infectious Disease.2020; 5(4): 169. CrossRef - Vaccination strategies to control Ebola epidemics in the context of variable household inaccessibility levels
Gerardo Chowell, Amna Tariq, Maria Kiskowski, Benjamin Althouse
PLOS Neglected Tropical Diseases.2019; 13(11): e0007814. CrossRef - Application of the CDC EbolaResponse Modeling tool to disease predictions
Robert H. Gaffey, Cécile Viboud
Epidemics.2018; 22: 22. CrossRef - A mathematical model with isolation for the dynamics of Ebola virus
Amira Rachah
Journal of Physics: Conference Series.2018; 1132: 012058. CrossRef - Multiscale model for pedestrian and infection dynamics during air travel
Sirish Namilae, Pierrot Derjany, Anuj Mubayi, Mathew Scotch, Ashok Srinivasan
Physical Review E.2017;[Epub] CrossRef - Modeling ebola virus disease transmissions with reservoir in a complex virus life ecology
Tsanou Berge, Samuel Bowong, Jean Lubuma, Martin Luther Mann Manyombe
Mathematical Biosciences and Engineering.2017; 15(1): 21. CrossRef - Application of a quantitative entry assessment model to compare the relative risk of incursion of zoonotic bat-borne viruses into European Union Member States
Verity Horigan, Paul Gale, Rowena D. Kosmider, Christopher Minnis, Emma L. Snary, Andrew C. Breed, Robin R.L. Simons
Microbial Risk Analysis.2017; 7: 8. CrossRef - Multigroup deterministic and stochasticSEIRIepidemic models with nonlinear incidence rates and distributed delays: A stability analysis
Hong Zhang, Juan Xia, Paul Georgescu
Mathematical Methods in the Applied Sciences.2017; 40(18): 6254. CrossRef - Modeling spatial invasion of Ebola in West Africa
Jeremy P. D’Silva, Marisa C. Eisenberg
Journal of Theoretical Biology.2017; 428: 65. CrossRef - The potential impact of a prophylactic vaccine for Ebola in Sierra Leone
Erin N. Bodine, Connor Cook, Mikayla Shorten
Mathematical Biosciences and Engineering.2017; 15(2): 337. CrossRef - Ebola virus – from neglected threat to global emergency state
Daniela Alexandra de Meneses Rocha Aguiar Pacheco, Acácio Agostinho Gonçalves Rodrigues, Carmen Maria Lisboa da Silva
Revista da Associação Médica Brasileira.2016; 62(5): 458. CrossRef - Neglected filoviruses
Robin Burk, Laura Bollinger, Joshua C. Johnson, Jiro Wada, Sheli R. Radoshitzky, Gustavo Palacios, Sina Bavari, Peter B. Jahrling, Jens H. Kuhn, Urs Greber
FEMS Microbiology Reviews.2016; 40(4): 494. CrossRef - Treatment–donation-stockpile dynamics in ebola convalescent blood transfusion therapy
Xi Huo, Xiaodan Sun, Kunquan Lan, Jianhong Wu
Journal of Theoretical Biology.2016; 392: 53. CrossRef - Ebola virus disease in nonendemic countries
Samson Sai-Yin Wong, Sally Cheuk-Ying Wong
Journal of the Formosan Medical Association.2015; 114(5): 384. CrossRef - Ebola Hemorrhagic Fever
Maryam Keshtkar Jahromi, Batool Sharifi Mood
International Journal of Infection.2015;[Epub] CrossRef - Tactics and Strategies for Managing Ebola Outbreaks and the Salience of Immunization
Wayne M. Getz, Jean-Paul Gonzalez, Richard Salter, James Bangura, Colin Carlson, Moinya Coomber, Eric Dougherty, David Kargbo, Nathan D. Wolfe, Nadia Wauquier
Computational and Mathematical Methods in Medicine.2015; 2015: 1. CrossRef - What is Ebola?
R. A. Stein
International Journal of Clinical Practice.2015; 69(1): 49. CrossRef - Ebola virus disease outbreak in Nigeria: Transmission dynamics and rapid control
C.L. Althaus, N. Low, E.O. Musa, F. Shuaib, S. Gsteiger
Epidemics.2015; 11: 80. CrossRef - A review of epidemiological parameters from Ebola outbreaks to inform early public health decision-making
Maria D. Van Kerkhove, Ana I. Bento, Harriet L. Mills, Neil M. Ferguson, Christl A. Donnelly
Scientific Data.2015;[Epub] CrossRef - Modeling Post-death Transmission of Ebola: Challenges for Inference and Opportunities for Control
Joshua S. Weitz, Jonathan Dushoff
Scientific Reports.2015;[Epub] CrossRef - Transmission Models of Historical Ebola Outbreaks
John M. Drake, Iurii Bakach, Matthew R. Just, Suzanne M. O’Regan, Manoj Gambhir, Isaac Chun-Hai Fung
Emerging Infectious Diseases.2015; 21(8): 1447. CrossRef - Theoretical perspectives on the infectiousness of Ebola virus disease
Hiroshi Nishiura, Gerardo Chowell
Theoretical Biology and Medical Modelling.2015;[Epub] CrossRef - Effect of Ebola Progression on Transmission and Control in Liberia
Dan Yamin, Shai Gertler, Martial L. Ndeffo-Mbah, Laura A. Skrip, Mosoka Fallah, Tolbert G. Nyenswah, Frederick L. Altice, Alison P. Galvani
Annals of Internal Medicine.2015; 162(1): 11. CrossRef - Transmission dynamics and control of Ebola virus disease (EVD): a review
Gerardo Chowell, Hiroshi Nishiura
BMC Medicine.2014;[Epub] CrossRef - Analysis of Ebolavirus with Decision Tree and Apriori algorithm
Eunby Go, Seungmin Lee, Taeseon Yoon
International Journal of Machine Learning and Comp.2014; 4(6): 543. CrossRef - Calculation of incubation period and serial interval from multiple outbreaks of Marburg virus disease
Boris I Pavlin
BMC Research Notes.2014; 7(1): 906. CrossRef - Outbreaks of Ebola virus disease in Africa: the beginnings of a tragic saga
Jean-Philippe Chippaux
Journal of Venomous Animals and Toxins including T.2014; 20(1): 44. CrossRef - Association between temperature, humidity and ebolavirus disease outbreaks in Africa, 1976 to 2014
S Ng, B J Cowling
Eurosurveillance.2014;[Epub] CrossRef - Early transmission dynamics of Ebola virus disease (EVD), West Africa, March to August 2014
H Nishiura, G Chowell
Eurosurveillance.2014;[Epub] CrossRef - Transmission dynamics and control of Ebola virus disease outbreak in Nigeria, July to September 2014
F O Fasina, A Shittu, D Lazarus, O Tomori, L Simonsen, C Viboud, G Chowell
Eurosurveillance.2014;[Epub] CrossRef - The Road Less Traveled
Chaeshin Chu
Osong Public Health and Research Perspectives.2011; 2(1): 1. CrossRef
- Prevention and post-exposure management of occupational exposure to Ebola virus



 First
First Prev
Prev


