Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 7(1); 2016 > Article
-
Original Article
Impact of Community-Based Approach as Policy Tool: World Health Organization-Designated Safe Communities of Korea and Health Action Zones of the United Kingdom - Changhyun Kanga, Jihyung Shinb, Bob Matthewsc
-
Osong Public Health and Research Perspectives 2015;7(1):36-42.
DOI: https://doi.org/10.1016/j.phrp.2015.10.005
Published online: October 20, 2015
aDepartment of Public Administration (Health and Welfare), Dankook University, Cheonan, Korea
bICT Statistics Center, Korea Information Society Development Institute, Jincheon, Korea
cDepartment of Social Policy, Birmingham University, UK
- ∗Corresponding author. welchkang@empas.com
• Received: January 9, 2015 • Accepted: October 12, 2015
Copyright © 2015 Korea Centers for Disease Control and Prevention. Published by Elsevier Korea LLC.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
- 2,770 Views
- 19 Download
- 2 Crossref
Abstract
-
Objectives
- The aim of this study is to ascertain and identify the effectiveness of area-based initiatives as a policy tool mediated by societal and individual factors in the five World Health Organization (WHO)-designated Safe Communities of Korea and the Health Action Zones of the United Kingdom (UK).
-
Methods
- The Korean National Hospital discharge in-depth injury survey from the Korea Centers for Disease Control and Prevention and causes of death statistics by the Statistics Korea were used for all analyses. The trend and changes in injury rate and mortality by external causes were compared among the five WHO-designated Safe Communities in Korea.
-
Results
- The injury incident rates decreased at a greater level in the Safe Communities compared with the national average. Similar results were shown for the changes in unintentional injury incident rates. In comparison of changes in mortality rate by external causes between 2005 and 2011, the rate increase in Safe Communities was higher than the national average except for Jeju, where the mortality rate by external causes decreased.
-
Conclusion
- When the Healthy Action Zones of the UK and the WHO Safe Communities of Korea were examined, the outcomes were interpreted differently among the compared index, regions, and time periods. Therefore, qualitative outcomes, such as bringing the residents' attention to the safety of the communities and promoting participation and coordination of stakeholders, should also be considered as important impacts of the community-based initiatives.
- In the governance era, the policy tools or instruments have been more significant than program itself regarding its impact on the outcomes, and they are identifiable by being structured to address a public problem [1]. Of the policy tools, a community building such as area-based initiatives (ABIs) is characterized as a multiagency collaboration, long-term perspective, locality, and so on. In this context, the meaning of the community is different from simple collection of building or general public. It also holds territorial and relational concepts among the people. Mattessich and Monsey [2] found several definitions of community such as (1) “a location or interaction among individuals for mutual support with a common interest or tie” and (2) “people who live within a geographically defined area and who have social and psychological ties with each other and with the place where they live.” Similarly, Green and Haines [3] define community development as “planned effort to build assets that increase the capacity of residents to improve their quality of life.”
- Therefore, strengthening the community capacity for long-term outcomes is a fundamental factor rather than achieving short-term outcomes in the area-based community development such as the World Health Organization (WHO) Safe Communities and Healthy Action Zones (HAZs) in the United Kingdom (UK). These characteristics may serve as disadvantages as a community-based policy tool. Although Howlett and Ramesh [4] characterized the use of community as the weakest form of policy instrument, they also asserted that community-based policies are favored in many societies because of their cost-effectiveness, consistency with the cultural norms of individual freedoms, and support for family and community ties. Although many researchers have not paid attention to community-oriented governing techniques, community-based policies have key focal components of using local geographic areas as the communities; enhancing existing community-based services, community structure, or identity; building a stronger bond among the general citizens and nongovernment community organizations; and establishing decentralized policymaking [5]. As community-based policies are the ABIs, it is difficult to detect the effects of each program. However, they are a useful policy tool to capture and manage the changes in communities as a whole. The aim of this study is to ascertain and identify the effectiveness of ABIs as a policy tool mediated by societal and individual factors in the WHO-designated Safe Communities of Korea and the HAZs of the UK.
Introduction
- 2.1 HAZs of the UK and the evaluation
- In the late 20th century, improving specific geographic area was a popularized approach as a government-programmed policy tool [6]. However, in the UK, ABIs have been deployed to ameliorate the problems in distressed areas owing to the inadequate responses of both the market and the state [7]. HAZs have been established as vehicles for change since 1997 in the UK. The aim was to explore mechanisms for breaking through current organizational boundaries to tackle inequalities, and deliver better services and better health care, building upon and encouraging cooperation across the National Health Service. Twenty-six zones were selected with a range of projects designed to be developed over a 7-year period because of their high levels of ill health and disadvantages. However, HAZs need to be assessed in detail according to the following items by index: (1) improving health and reducing health inequalities, (2) tackling the root cause of ill health, (3) empowering local communities, (4) reshaping health and social care, (5) becoming learning organizations, and (6) developing effective partnerships.
- To evaluate HAZs, the theory of change has been introduced in analyzing the outcomes. The “Theories of Change” was designed by the Aspen Institute to evaluate U.S. social policy programs 8, 9. The theory of change evaluation is a hybrid of both process and outcome analyses that can be used without any comparison groups with perspectives of all stakeholders involved, and it provides a strategic perspective on the policy interventions that are dynamic and complex 10, 11, 12. However, the use of the theory of change as an evaluation tool should be based on a solid understanding of the outcome measure of the impact of policy as well as sufficient development of evaluation theory and method itself [7]. Indeed, central to a theory of change evaluation can be surfacing the implicit theory of policy instrument and outcome relation [13]. Even with the proper quantitative measure of both outputs and outcomes of ABIs, there are limitations in data analyses such as geographical coverage of survey data and noticeable changes slowly taking places [14]. For example, in the evaluation of HAZs, Sullivan et al [6] focused on four key areas: detection and examination of changes, study of collaborative capacity, and assessment of health inequalities. As an outcome, Bauld et al [15] compared the Mortality of HAZ with non-HAZ area to explore population level impact based on the theory of change. The results show that mortality from CHD decreased between 1997 and 2001. The mortality rate from suicide increased in deprived non-HAZ local authority areas and in second wave HAZs between 1997 and 2002. The greatest decrease was observed in first wave HAZ areas. Mortality from accidental falls in nondeprived local authorities is the lowest, although it increased in all four groups. The greatest decrease in mortality from accidents is in second wave HAZs [15]. A mixed picture emerges from this brief analysis. HAZs appear to have outperformed other areas in relation to a number of indicators that are related to their programs and national policy priorities. However, the findings are not consistent among the indicators.
- 2.2 WHO-designated Safe Communities in Korea
- The Safe Community movement was launched by the WHO Collaborating Centre on Community Safety Promotion at the Karolinska Institutet, Solna, Sweden. This center guides and certifies cities that want to be classified as a Safe Community. A total of 213 cities have been designated as Safe Communities around the world by May 2011. The six indicators for international Safe Communities are as follows: (1) an infrastructure based on partnership and collaborations, governed by a cross-sectional group that is responsible for safety promotion in their community; (2) long-term, sustainable programs covering both sexes and all ages, environments, and situations; (3) programs targeting high-risk groups and environments, and programs that promote safety for vulnerable groups; (4) programs documenting the frequency and causes of injuries; (5) evaluation measures assessing their programs and processes and the effects of change; and (6) ongoing participation in national and international Safe Communities networks [16].
- Change in the injury rate is not required for the designation of Safe Community by the WHO Safe Community network. The six indicators for international Safe Communities are ultimately intended for prevention and reduction of injuries. Moreover, the designated communities can keep their accreditation by maintaining and adhering to the standards described in the six indicators. WHO defines safety as a state in which hazards and conditions leading to physical injury, and psychological or material harm are controlled in order to preserve the health and well-being of individuals and the community.
- Although the government, other organizations, and the population are responsible for the safety of the community, its promotion should closely be linked to all participants. From structuring the objectives to planning the execution of the solutions, each and every involved organization and population need to be linked to every sector of the activities [17].
- In Korea, the WHO Safe Community project has been accomplished by local governments through their own efforts without national government policy. Suwon, Jeju, Songpa, Cheonan, and Wonju have participated in this program as designated WHO Safe Communities (Table 1). Other communities are also making preparations to become a member of the international Safe Community network. The project has been started and managed by bureaucratic initiatives such as general, fire, or health administration, and each community established different implementation systems. Meanwhile, the national government has no interest both in the WHO Safe Community project and policy link with local governments. However, Cheonan is the only case in which the national policy fund has been involved among the designated WHO Safe Communities in 2009.
- We adopt the theory of change approach to evaluate the Safe Community programs in Korea, which fits well with the key features of this policy instrument. In measuring the impact of ABIs on health and safety in Korea and the UK, this study closely follows the methodology introduced in the study of Bauld et al [15]. The external assessments of overall impact involve a review of routinely available health data to identify the differences between HAZ and non-HAZ areas, designated Safe Communities, and control communities in relation to key outcomes. Previously, Nilsen et al [18] evaluated the area-based effectiveness of the WHO Safe Communities network in terms of the injury prevention based on long-term injury rate, changes, and trend. In determining the effectiveness of the WHO Safe Communities model for the prevention of injuries in whole populations, the change measures in injury levels of both morbidity and mortality were used. Changes in injury rates between before and after the policy interventions were compared among the targeted communities [19]. In the evaluation of ABIs, the size of the community can also affect the outcome measures. To control the community size effect, 19 areas with a population size ranging between 500,000 and 1,000,000 were selected as control communities, and their average injury rates and mortality level by external causes were compared with those of the designated WHO Safe Communities. The following communities were chosen as control communities: Seoul (Nowon, Eunpyung, Gangseo, Gwanak, and Gangnam), Daegu (Dalseo), Incheon (Namdong and Bupyeong), Gyeonggi (Seongnam, Anyang, Bucheon, Ansan, Goyang, Namyangju, Yongin, and Hwaseong), Cheongju, Jeonju, and Pohang.
- 2.3 Data
- No household survey was conducted for the measurement of improvement of population health or reduction of health inequalities in HAZs for the evaluation of ABIs. Rather, in the Compendium of Clinical and Health Indicators, which is produced by the National Center for Health Outcomes Development, the routinely collected data are used to examine the impact of HAZs [15]. Likewise, for the statistical evaluation in WHO Safe Communities in Korea, the authors used the Korean national hospital discharge in-depth injury survey from the Korea Centers for Disease Control and Prevention and causes of death statistics by the Statistics Korea.
Materials and methods
- 3.1 Trends and changes
- The designation of the WHO Safe Communities requires the initiation of programs described in the six indicators for international Safe Communities. First, we examined if there has been any reduction of injury level in between the preparation point when such program for the WHO Safe Communities designation begun and the designation point.
- The mortality rate by external causes in Korea was about 60 persons per population of 100,000 persons in 2005, and then increased to 65 persons per population of 100,000 persons in 2009 without any significant changes. In Suwon, after its redesignation as a WHO Safe Community in 2007, the morality rate by external causes keeps increasing. Among the WHO-designated Safe Communities in Korea, without any significant changes between 2005 (the preparation point) and 2007 (the designation point), Jeju maintained the highest level of mortality rate by external causes of about 75 persons per population of 100,000 persons. Although there had not been any remarkable changes in the level of mortality rate by external causes in Songpa, this rate kept increasing in Cheonan even after the designation. Inconsistent levels of mortality by external cause were observed among the five different Safe Communities in Korea. Jeju and Wonju have higher mortality levels by external causes than the national average, whereas Suwon and Songpa do not. In Cheonan, the mortality rate by external causes exceeded the national average in 2010 (Fig. 1).
- In Suwon, after its redesignation as a WHO Safe Community, the injury rate has significantly increased. In Jeju, the injury rate also increased between 2005 and 2007, but the rate decreased right after it was designated as a WHO Safe Community, then began to increase again in 2008. The injury rate in Songpa decreased in 2005 and 2008 and maintained this level after the designation in 2008. During the preparation period (from 2005 and 2009), the injury rate decreased in Wonju; the rate was also maintained at this level after the designation. In between the beginning of programs and designation, the injury rate was increasing in Cheonan; after the designation, the injury rate kept decreasing. Overall, the injury rates of accredited WHO Safe Communities in Korea are higher than the national average, and these rates have been fluctuating wildly compared to those of control communities. This implies that the implemented programs had both a positive and negative influence in the communities. Only Wonju and Songpa had lower injury rates than the control communities after 2008 (Fig. 2).
- In comparison of changes in mortality rate by external causes between 2005 and 2011, the rate increase in Safe Communities was higher than the national average except in Jeju, where the mortality rate by external cause was decreased. Among the external causes of mortality, the national average mortality rate by transport accidents decreased by 22%; that of Suwon and Cheonan decreased by slightly more, whereas the rate in Wonju increased by 31%. Although the national mortality rate caused by falls decreased by 33%, the changes in rates in all Safe Communities in Korea were not any better than the national average with increases in rates in Suwon and Jeju. However, the nationwide changes in mortality caused by drowning were decreased by 27%, with a dramatic reduction in Cheonan and Suwon and a slight increase in Wonju and Jeju. By contrast, the suicide rate has significantly increased with even higher rates in Safe Communities than the national average except for Jeju (Table 2).
- 3.2 Comparative analysis
- The changes in injury incident rates between 2005 and 2010 in the Safe Communities were higher than the national average and those in control communities. It is notable that the injury incident rates decreased more in Safe Communities when compared with the national average. Similar results were shown for the changes in unintentional injury incident rates.
- For those who are older than 65 years, the national rates of intentional self-injury incident increased, whereas the rates in both the Safe Communities and control communities decreased (Table 3).
- The changes in injury incidents were different by injury mechanism (Table 4). Injuries caused by transport accidents has been markedly decreased in Songpa (62.32%) and Wonju (−32.82%), whereas those were increased among individuals who were 15–64 years old in Suwon and Jeju, and 65 years and older in Cheonan. Cheonan was the only community with decreased changes in injury rates caused by falls and slip down in all age groups. Among other communities, the rates were increased with the worst changes in Jeju. In Songpa and Wonju, decreases in injury rates caused by falls or slip down were observed whereas increases in these rates were observed in other areas. The injuries attributed to stab wounds or cuts in all and control communities were reduced, as in Songpa and Wonju. Accidental drug abuse or poisonings were decreased more in Songpa and Suwon compared to the decreases in control communities. However, the number of incidents increased in Wonju and Jeju.
Results
- The interpretation of findings should be done carefully with caution. Bauld et al [15] noted three major reasons for this: the changes in population health should be related as long-term outcomes, the regional difference in comparison of grouped areas should be considered, and secondary data analyses of the observed data does not guarantee causal effects. Community-based policy interventions, such as Safe Communities or Health Action Zones, have several limitations when evaluating the outcomes: (1) various causal factors are applied to the program; (2) stakeholders are linked in a complex form; (3) there are contextual differences among the regions/communities; (4) long-term follow-up and evaluations are required.
- When the HAZs of the UK and the WHO-designated Safe Communities of Korea were examined by multiple measurable indices, the outcomes were interpreted differently among the compared index, regions, and time periods. It is difficult and complicated to set specified quantitative measures as the ultimate goals of these ABIs. Although it is necessary to compare different types of indicators, it is difficult to interpret inconsistent results depending on the methods used for public policy analyses and evaluations. Therefore, intangible outcomes, such as bringing the residents' attention to the safety of the communities and promoting participation and coordination of stakeholders, should also be considered as important changes in addition to tangible outcomes that can be measured quantitatively. Also, in an assessment of the HAZ programs, although it was challenging to understand the outcomes of the policy instruments by examining the quantitative measures, a wider range of stakeholders defined individual projects, and processes were real successes. In addition, a growing awareness of Safe Community and establishing budget structure regardless of local political transformation can also be considered as positive effects of the community-based programs.
- Recently, in South Korea, under the Park Geun-hye administration as part of the central government restructuring, the Ministry of Public Administration and Security was changed to the Ministry of Security and Public Administration to reinforce safety as part of the national agenda and to eradicate the “Four Major Social Evils”: sexual violence, domestic violence, school violence, and unsafe food. Local governments created the departments for community safety, and it is projected that the grant programs for Safe Communities will be expanded. At the same time, the WHO Safe Community program such as ABIs became eligible for receiving grants because it corresponds well with the central government policy. Among the WHO Safe Communities in Korea, only Cheonan was able to obtain accreditation both as a WHO Safe Community and a Korean safe city. This serves as the background for mandating the establishment of Social Safety Network Center in 2013 without any doubts from local politicians and bureaucrats.
Discussion
-
Acknowledgements
- This study was supported by the National Research Foundation of Korea Grant funded by the Korean Government (NRF-2010-013-B00047).
Acknowledgments
- 1. Salamon L.M.. The tools of government: a guide to the new governance. 2002. Oxford University Press; New York: p 19.
- 2. Mattessich P., Monsey M.. Community building: what makes it work. 2004. Wilder Foundation; St. Paul, MN: p 56.
- 3. Green G.P., Haines A.. Asset building and community development. 2nd ed.2007. Sage Publications; Thousand Oaks, CA: p 7.
- 4. Howlett M., Ramesh M.. Studying public policy: policy cycles and policy subsystems. 1995. Oxford University Press; Toronto: p 83.
- 5. Rochefort D.A., Rosenberg M., White D.. Community as a policy instrument: a comparative analysis. Policy Stud J 26(3). 1998;548−568.Article
- 6. Sullivan H., Barnes M., Matka E.. Collaborative capacity and strategies in area-based initiatives. Public Admin 84(2). 2006;289−310.Article
- 7. Rhodes J., Tyler P., Brennan A.. Assessing the effect of area based initiatives on local area outcomes: some thoughts based on the national evaluation of the single regeneration budget in England. Urban Stud 42(11). 2005;1919−1946.Article
- 8. The Aspen Institute . Voices from the field: learning from the early work of comprehensive community initiatives. 1997. Aspen Institute; Washington, DC.
- 9. Judge K., Bauld L.. Strong theory, flexible methods: evaluating complex community-based initiatives. Crit Public Health 11:2001;19−38.Article
- 10. Kooiman J.. Modern governance: new government–society interactions. 1993. Sage; Thousand Oaks, CA: p 35.
- 11. Connell J.P., Kubisch A.C.. Applying a theory of change approach to the evaluation of comprehensive community initiatives: progress, prospects and problems. Theory, measurement, and analysis. 1998. Aspen Institute; Washington, DC: pp 15−44.
- 12. Blamey A., Mackenzie M.. Theories of change and realistic peas in a pod or apples and oranges? Evaluation 13:2007;439−455.Article
- 13. Sullivan H., Gillanders G., Goss S.. Developing a ‘theory of change’ to evaluate local public service agreements (No. 5163&l). Working Paper, National evaluation of LPSAs. ODPM. 2004. p 4
- 14. Noble M., Wright G., Smith G.. Growing together or growing apart? 2002. Policy Press.
- 15. Bauld L., Sullivan H., Judge K.. Assessing the impact of Health Action Zones. Edited by Barnes M., Bauld L., Benzeval M., Judge K., Mackenzie M., Sullivan H.: Health Action Zones: Partnerships for Health Equity. 2005. Routledge; London (UK): p 162.
- 16. http://www.ki.se/csp/who_safe_communities_indicators_en.htm.
- 17. Maurice P., Lavoie M., Chapdelaine A.. Safety and safety promotion: conceptual and operational aspects. 1998. WHO Collaborating Centre on Community Safety Promotion.
- 18. Nilsen P., Ekman R., Ekman D.S.. Effectiveness of community-based injury prevention: long-term injury rate levels, changes, and trends for 14 Swedish WHO-designated Safe Communities. Accid Anal Prev 39(2). 2007;267−273. PMID: 17027531.ArticlePubMed
- 19. Spinks A., Turner C., Nixon J.. The ‘WHO Safe Communities’ model for the prevention of injury in whole populations. Cochrane Library (3). 2009;CD004445.Article
References
Figure 1Mortality by external causes per population of 100,000 persons, 2005–2011. Note. From “Cause of death statistics” in Statistics Korea.
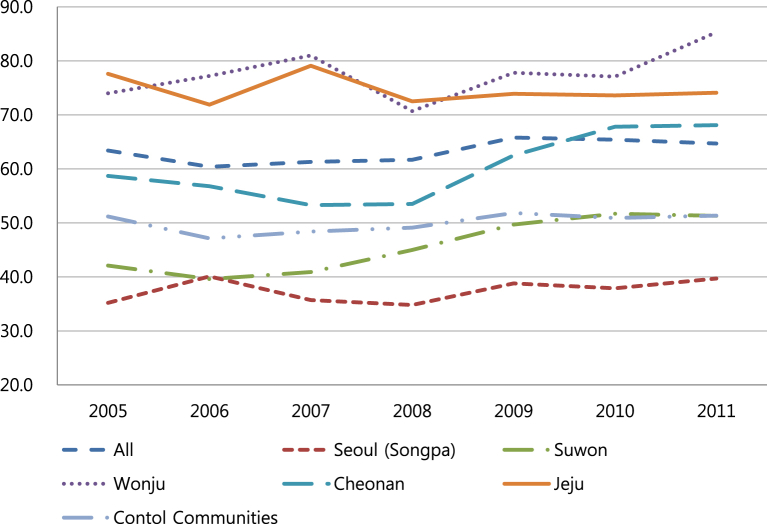
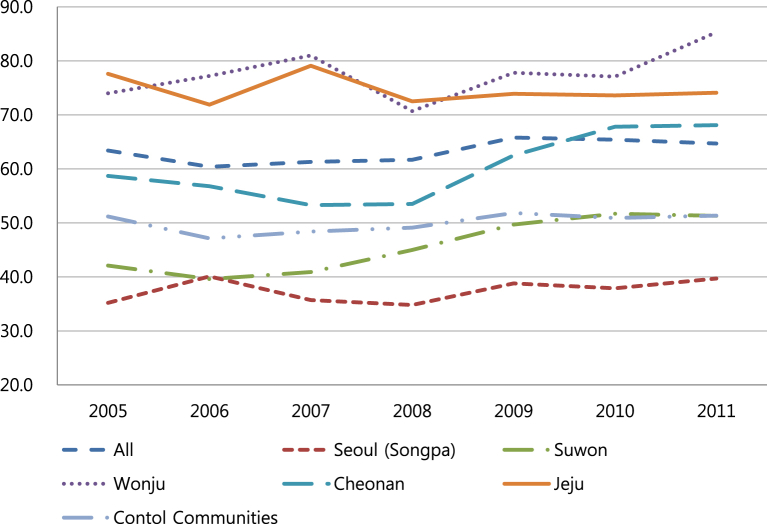
Figure 2Injury rate per 100,000 persons in 2005–2010. Note. From “Korean National Hospital discharge in-depth injury survey” by Korea Centers for Disease Control and Prevention.
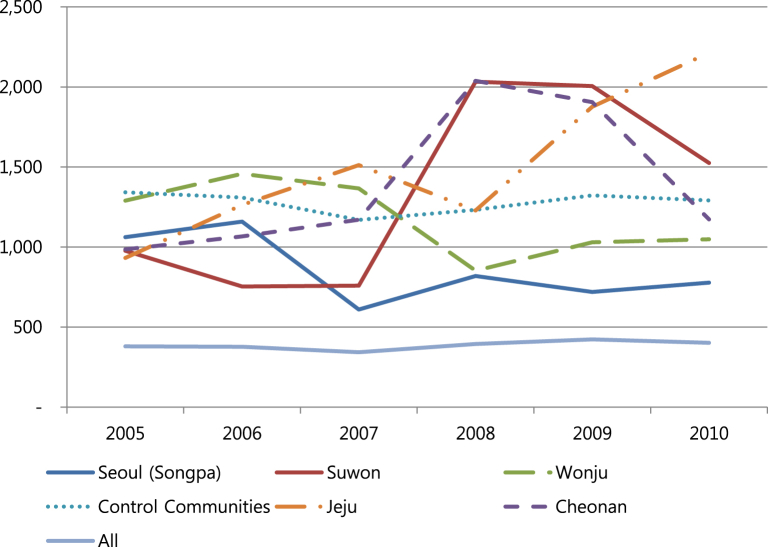
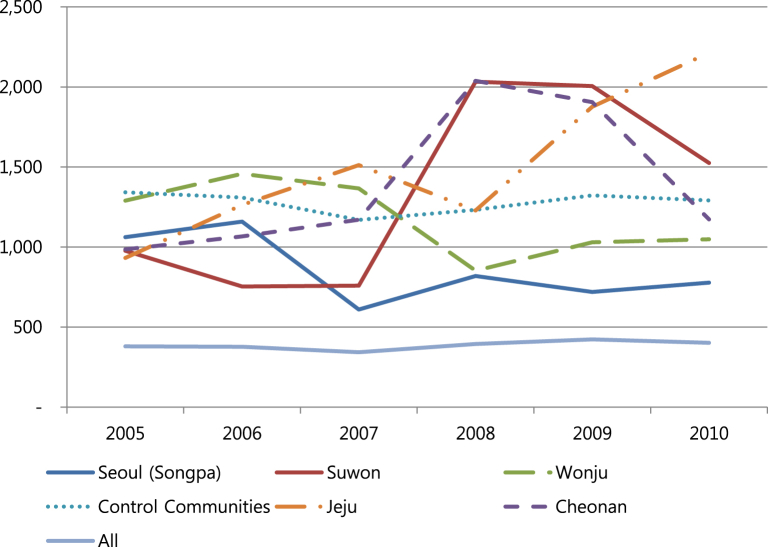
Table 1World Health Organization Safe Community in Korea.
| City | Department in Charge | Beginning | Designated | Inhabitantsa |
|---|---|---|---|---|
| Suwon | Disaster control | 1999 | 2002, 2007 | 1,141 |
| Jeju | Fire agency | 2005 | 2007, 2012 | 591 |
| Seoul (Songpa) | Health agency | 2005 | 2008, 2013 | 667 |
| Wonju | Planning & budgeting | 2005 | 2009 | 325 |
| Cheonan | Disaster control | 2007 | 2009 | 589 |
Table 2Changes in mortality by external causes 2005–2011.
Table 3Changes in injury incident 2005–2010.
Table 4Changes (%) in injury by mechanism 2005–2010.
Figure & Data
References
Citations
Citations to this article as recorded by 

- Working in partnership with communities to improve health and research outcomes. Comparisons and commonalities between the UK and South Africa
Patricia Wilson, Azwihangwisi Helen Mavhandu-Mudzusi
Primary Health Care Research & Development.2019;[Epub] CrossRef - THE SAFE COMMUNITY CONCEPT – A SUCCESSFUL TOOL FOR INJURY PREVENTION AND SAFETY PROMOTION
Birutė Strukčinskienė, Sabine Distl, Sigitas Griškonis
Visuomenės sveikata.2019; 28(7): 41. CrossRef


 PubReader
PubReader Cite
Cite
