Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 13(2); 2022 > Article
-
Original Article
COVID-19 outbreak response at a nursing hospital in South Korea in the post-vaccination era, including an estimation of the effectiveness of the first shot of the Oxford-AstraZeneca COVID-19 vaccine (ChAdOx1-S) -
Chanhee Kim1
 , Geon Kang1
, Geon Kang1 , Sun Gu Kang1
, Sun Gu Kang1 , Heeyoung Lee2
, Heeyoung Lee2
-
Osong Public Health and Research Perspectives 2022;13(2):114-122.
DOI: https://doi.org/10.24171/j.phrp.2021.0262
Published online: April 26, 2022
1Infectious Disease Control Center, Gyeonggi Provincial Government, Suwon, Korea
2Center for Preventive Medicine and Public Health, Seoul National University Bundang Hospital, Seongnam, Korea
- Corresponding author: Heeyoung Lee Center for Preventive Medicine and Public Health, Seoul National University Bundang Hospital, 82 Gumi-ro 173beon-gil, Bundang-gu, Seongnam 13620, Korea E-mail: wanderingstone@gmail.com
© 2022 Korea Disease Control and Prevention Agency.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Abstract
-
Objectives
- We descriptively reviewed a coronavirus disease 2019 (COVID-19) outbreak at a nursing hospital in Gyeonggi Province (South Korea) and assessed the effectiveness of the first dose of the Oxford-AstraZeneca vaccine in a real-world population.
-
Methods
- The general process of the epidemiological investigation included a public health intervention. The relative risk (RR) of vaccinated and unvaccinated groups was calculated and compared to confirm the risk of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection, and vaccine effectiveness was evaluated based on the calculated RR.
-
Results
- The population at risk was confined to ward E among 8 wards of Hospital X, where the outbreak occurred. This population comprised 55 people, including 39 patients, 12 nurses, and 4 caregivers, and 19 cases were identified. The RR between the vaccinated and unvaccinated groups was 0.04, resulting in a vaccine effectiveness of 95.3%. The vaccination rate of the non-patients in ward E was the lowest in the entire hospital, whereas the overall vaccination rate of the combined patient and non-patient groups in ward E was the third lowest.
-
Conclusion
- The first dose of the Oxford-AstraZeneca vaccine (ChAdOx1-S) was effective in preventing SARS-CoV-2 infection. To prevent COVID-19 outbreaks in medical facilities, it is important to prioritize the vaccination of healthcare providers.
- Since the first case of coronavirus disease 2019 (COVID-19) was reported in China in December 2019, the world has been experiencing an unprecedented highly infectious global pandemic [1−3]. In South Korea, after the first COVID-19 case was reported on January 20, 2020, the epidemic has continued to spread mainly in metropolitan areas, except for the unusual cluster of infections in Daegu and Gyeongbuk Province in February and March 2020, respectively [4−6].
- In December 2020, the American pharmaceutical companies, Pfizer and BioNTech, received emergency approval for the use of vaccines in the United Kingdom, and the response to the COVID-19 pandemic entered a new phase [7,8]. In February 2021, the administration of COVID-19 vaccines to workers and residents of nursing homes, and other healthcare workers, was initiated in South Korea. Since June 2021, the target vaccinated population has been gradually expanding [9−11]. The older population in long-term care facilities in South Korea was prioritized for vaccination due to their high fatality rates from severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection [11,12].
- Our study introduces the response to a COVID-19 outbreak among the staff and residents of long-term care hospital, (i.e., one of the first vaccinated populations in South Korea). Using real-world data from this outbreak, we also analyzed the effectiveness of the COVID-19 vaccine among this partially vaccinated population. Although the efficacy of vaccines can be confirmed using data published by the pharmaceutical companies in restricted laboratory environments, vaccine effectiveness (VE) is difficult to confirm unless data are obtained from actual populations in real clinical settings [13,14]. Hence, COVID-19 outbreaks in long-term care facilities provide a valuable opportunity to investigate VE in a real-world population.
Introduction
- Hospital X
- Hospital X (a nursing hospital located in Seongnam) is a single building with a total of 8 floors. This hospital specializes in rehabilitation treatment and operates various treatment programs such as physical therapy, manual therapy, and occupational therapy. At the time of the outbreak, 180 of the 204 hospital rooms were actually used, and there were 4 inpatient wards, which were operated across 6 floors. The hospital had a total of 172 employees, consisting of doctors, nurses, therapists, caregivers, pharmacists, nutritionists, administrators, and cleaners.
- Since the inpatients and employees of nursing hospitals were one of the first populations to be vaccinated in South Korea, most of the inpatients and employees of Hospital X were recommended to be vaccinated. However, employees who had a medical history or vaccination hesitancy and inpatients whose families disagreed with vaccination refused to be vaccinated. Those who agreed to be vaccinated received the vaccines between February 26 and March 29, 2021. Thus, the period from the first vaccination to the identification of the index case ranged from 40 to 71 days.
- Other than vaccination, the institution’s policies to prevent the influx of COVID-19 included regular reverse-transcription polymerase chain reaction (RT-PCR) tests for employees twice a week, prohibition of family visiting, and only allowing patients to leave for regular check-ups or medical requests to a higher-level hospital. At nursing hospitals, there is no mandatory regulation that requires dedicated personnel for infection control; therefore, at Hospital X, the head of the nursing department managed these hospital policies while acting as an infection control officer. In the process of the epidemiological investigation, the head of the nursing department also played a major role in delivering measures to block transmission or communicating data requests for epidemiological investigation.
- Data Collection
- On May 8, 2021, when the index case was reported at Hospital X in Seongnam, an in-facility risk assessment was carried out at the nursing hospital to determine whether there was a need to moderate the degree of existing measures, as cases were increasing. Individual, in-depth epidemiological investigations were carried out for the cases, the contacts were investigated, and the route of infection was determined based on transfer history, medical records, and outgoing history. The observation period was from May 5, 2021 (2 days before the sample collection date of the index case: i.e., May 7, 2021), when the index patient was assumed to have been infectious, to 2 weeks after the last case was identified, considering that the known longest incubation period of COVID-19 is 2 weeks [15−17].
- This study reviewed the reports of the epidemiological investigations conducted. Data on the dates of symptom onset and sample collection, age, occupation, sex, vaccination status, vaccine type, and vaccination date were analyzed. The distribution of cases within the hospital identified during the epidemiological investigations and public health measures was determined.
- Study Design
- We introduced measures implemented to prevent further transmission along with the overall epidemiological investigation process during the COVID-19 outbreak in the nursing hospital. We also estimated VE using the data collected from the entire investigation process. Since the outbreak was confined to ward E among 8 wards of Hospital X, we compared the relative risk (RR) of vaccinated and unvaccinated groups in ward E using the data collected by epidemiological investigation. As Hospital X targeted elderly people, ward E was also composed of aged patients
- Case Definition
- Based on the COVID-19 guidelines of the Korea Disease Control and Prevention Agency (KDCA), a confirmed case was defined as an individual who was confirmed to be positive for SARS-CoV-2, according to the diagnostic test standards, regardless of clinical features, from May 5, 2021 to June 8, 2021 [15]. As of May 8, 2021, when the index patient was reported, none of the staff and patients at the nursing hospital had received a second dose of the vaccine, and those who had been vaccinated had only received the first dose of the Oxford-AstraZeneca vaccine (ChAdOx1-S). Therefore, we defined vaccinated individuals as those who had received the first dose of the Oxford-AstraZeneca vaccine before the COVID-19 outbreak on May 7, 2021.
- Among 341 people who belonged to Hospital X, including staff and patients, those who were admitted to or worked at ward E, where the outbreak occurred, were defined as the population at risk. A patient was defined as a person admitted to ward E of Hospital X from May 5 to June 8, 2021, while staff referred to people who worked in ward E of Hospital X during the same period. Among the several job categories at Hospital X, only nurses and caregivers were included as the population at risk since confirmed cases were not reported from other job categories. As a result, 55 people were defined as the population at risk, including 39 patients, 12 nurses, and 4 caregivers.
- Laboratory Tests
- After the identification of the index case, upper respiratory tract specimens collected from nasopharyngeal and/or oropharyngeal swabs of the at-risk population were analyzed for the presence of SARS-CoV-2 using RT-PCR [18]. Data on the vaccination history of the at-risk population were collected. The RT-PCR assays were performed by private institutions in South Korea, including Seegene, Green Cross Laboratories, Lab Genomics, and Seoul Clinical Laboratories. Next-generation sequencing (NGS) was also performed by the Division of Emerging Infectious Diseases of the KDCA to identify the strain of the virus.
- Statistical Analysis
- The differences in the characteristics between the infected and uninfected groups were estimated using the chi-square test for categorical variables, and the 2-sample t-test for continuous variables. A p<0.05 was considered to indicate statistical significance. R ver. 4.1.0 (The R Foundation, Vienna, Austria; https://www.r-project.org/) was used to perform the statistical analysis. Regarding vaccination history, the RR of vaccinated and unvaccinated groups was calculated and compared to determine the risk of SARS-CoV-2 infection, and VE was evaluated based on the calculated RR reduction using the following formula [19]:
Materials and Methods
- Epidemiological Investigation
- The index case was a patient of Hospital X. On May 7, 2021, she underwent an RT-PCR test for COVID-19 to prepare for her transfer to a general hospital for spinal stenosis treatment, and tested positive the next day. Except for leaving the premises on April 25, 2021 for an outpatient visit to a general hospital, the patient had no known external movements and did not complain of any COVID-19-related symptoms at the time of diagnosis; therefore, the origin of the outbreak was unknown. In addition, South Korea implemented cyclic preemptive screening tests for facilities used by vulnerable groups, such as nursing hospitals, once a week. Consequently, every staff member was confirmed negative until May 7, 2021. Therefore, it would be difficult to conclude that the origin of the outbreak was the hospital staff.
- Following the identification of the index case, 2 more patients were confirmed positive. Both patients had gone out for outpatient visits to general hospitals on April 27, 2021. However, because they were diagnosed with asymptomatic SARS-CoV-2 infections, the route of infection could not be confirmed for these 3 patients, including the index case. The first case could not be identified because no additional confirmed cases were noted among the family members who accompanied all 3 patients when they left the hospital or when they visited patients in the hospital.
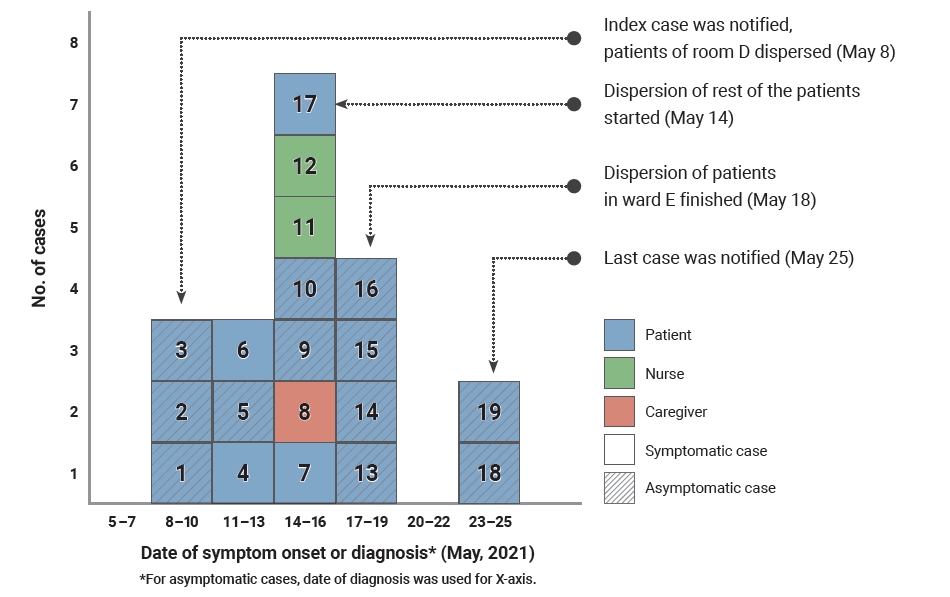
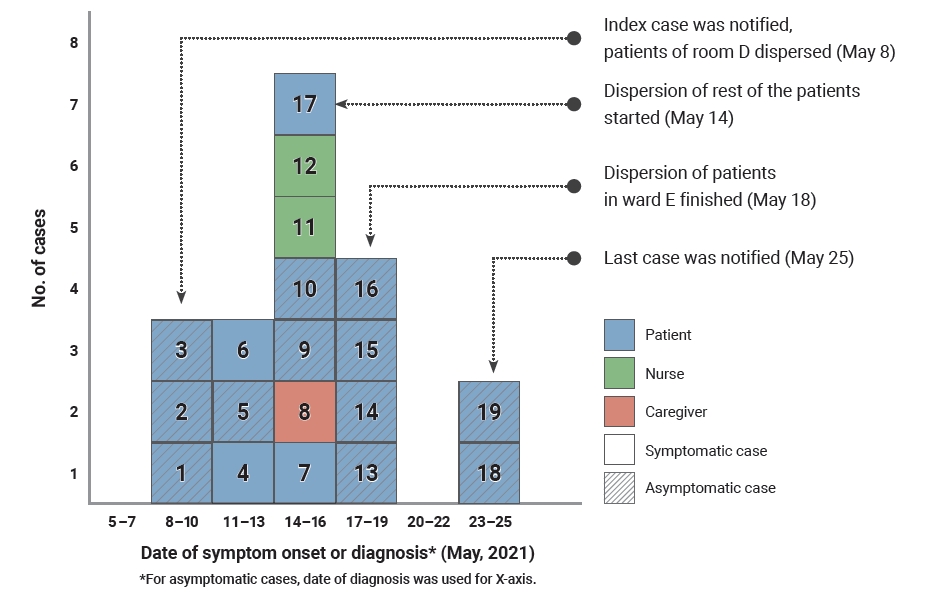
- Based on the instructions of the epidemiological investigator of the Gyeonggi Provincial Government, the nursing hospital conducted complete examinations thrice weekly, and those who showed clinical symptoms were immediately tested. An additional 16 cases were identified. After May 25, 2021, when the nineteenth case was confirmed, monitoring continued for 2 more weeks, and no additional cases were reported; therefore, monitoring was terminated (Figure 1). The 19 cases consisted of 16 inpatients, 2 nurses, and 1 caregiver.
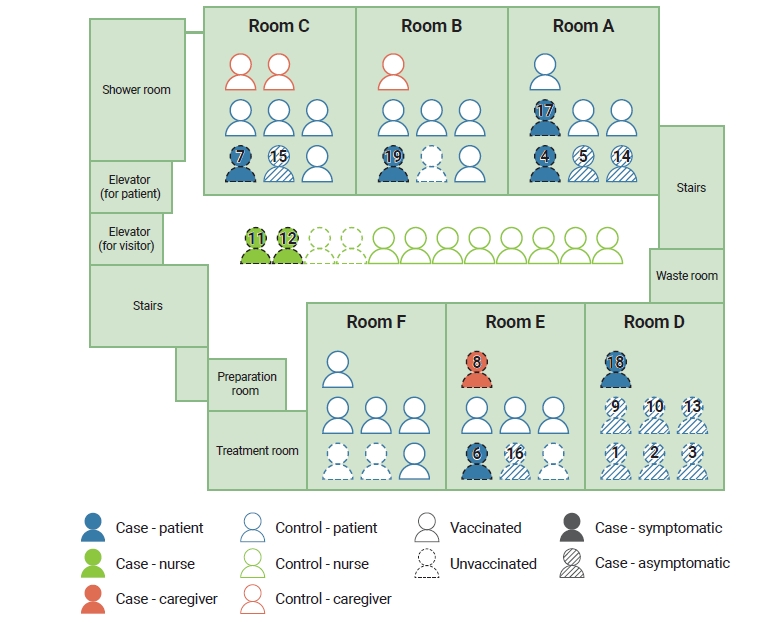
- All cases were distributed in ward E, and Figure 2 shows the distribution of the location of cases in ward E. In the room of the index patient, all patients were confirmed to be positive for COVID-19, and cases were reported in almost every room. Some cases were observed in patients receiving physical therapy; however, there were no confirmed cases in other occupational groups, such as therapists and doctors, in other wards or facilities in the hospital.
- Public Health Intervention
- As more cases were identified, the measures taken by the epidemiological investigators were also upgraded step-by-step. As the first 3 patients were staying in the same room, the initial measures involved the quarantine of staff and patients who entered the room. However, on May 13 and 14, as cases were identified in 2 more rooms, the entire ward E was sealed and was established as a contaminated zone. Cohort isolation was implemented for all staff members in ward E. However, as more cases were reported, most of the staff and caregivers self-quarantined, and the remaining patients who had to continue treatment were distributed to other nursing hospitals equipped with isolation beds.
- In the at-risk population, screening tests were performed thrice weekly. The first screening was conducted on May 8, when the index case was identified, which resulted in the identification of 2 more cases. Subsequently, periodic screening was performed every 2 to 3 days, so that additional cases could be rapidly detected. Among inpatients, 12 of 16 cases were detected before the onset of symptoms.
- Since the first 3 confirmed cases were found in the same room (Figure 2, Room D), dispersion was not considered. Instead, patients staying in Room D were classified for cohort isolation. However, as more confirmed cases were identified, it was decided to transfer the rest of the patients (i.e., to disperse the ward). Three nursing hospitals, 2 located in Seoul and 1 located in Gyeonggi Province, helped disperse the rest of the patients. Among 19 confirmed cases, 16 cases were patients and 9 of them were diagnosed with COVID-19 after dispersion. The positive conversion of these cases seemed to have been due to exposure before dispersion except for 1 case. This is because the hospital where the contacts were isolated provided a single or double room for each patient to prevent further transmission of the disease after dispersion. Double rooms were arranged for contacts who had shared the same room in Hospital X before dispersion.
- Vaccine Effectiveness
- Among all wards, Ward F showed the lowest vaccination rate (28.6%), and ward E, where the outbreak originated, had the third-lowest vaccination rate (54.5%) (Table 1). The vaccination rate of the patient group was 43.6%, and that of the non-patient group was 77.5%. The vaccination rate of patients in ward E was similar to those of wards B and C, and was higher than those of wards A and D. The vaccination rate of non-patients in ward E (62.5%) was the lowest in the entire hospital. Given the estimated RR of 0.04, the VE was calculated as 95.3% (Table 2). However, as the size of the population was relatively low, the confidence interval of the VE was wide, from 67.7% to 99.3%.
- Epidemiological and Clinical Characteristics
- A total of 181 patients had been admitted to the hospital since May 5, 2021, when the index patient was estimated to have started being infectious, and 16 of them were confirmed as positive for COVID-19. Among the 156 staff members, including doctors, nurses, nursing assistants, therapists, caregivers, and other hospital staff members, 3 were confirmed as positive for COVID-19. Among several characteristics, the vaccination rate showed a statistically significant difference between the infected and non-infected groups (Table 3). Among cases (the infected group), only 1 case was vaccinated, whereas 52.8% of the non-infected group were vaccinated.
- As the outbreak occurred in a nursing hospital, most confirmed cases were inpatients; hence, they were transferred to general or nursing hospitals for isolation and treatment because of their old age-related issues and underlying diseases (Table 4). The 2 patients assigned to the residential treatment center were a caregiver and a nurse. All inpatients were assigned to either general hospitals (including tertiary hospitals) or nursing hospitals. At the end of the monitoring period, 3 deaths were reported, resulting in a fatality rate of 15.8%.
- NGS Results
- Although 18 of 19 confirmed cases were not vaccinated, 1 case was a person who had received the first dose of the Oxford-AstraZeneca vaccine. NGS revealed that there were 6 cases, including 1 vaccinated case, of the B.1.1.7. (Alpha) variant in this outbreak, which was first identified in the United Kingdom [20].
- According to the KDCA guidelines for the management of patients with variants of COVID-19, the abovementioned 6 cases were classified as confirmed cases of variants [21]. The remaining 13 cases were classified as epidemiologically related cases, and were managed in a similar way to confirmed variant cases, because their contact history involved no other sources of infection.
Results
- This study described the process and results of an epidemiological investigation of a COVID-19 outbreak at a nursing hospital in Gyeonggi Province and estimated the VE by calculating the RR of the infected and uninfected groups according to their COVID-19 vaccination history. We confirmed that the first dose of the Oxford-AstraZeneca vaccine was effective in preventing SARS-CoV-2 infection. In addition, the vaccination rate of patients in ward E was similar to or higher than that of other wards. However, the vaccination rate of the non-patient group was the lowest in the entire hospital, suggesting the importance of vaccinating healthcare providers.
- Considering the high number of long-term and bedridden patients in most nursing hospitals, we speculate that the outbreak originated from a staff member or visitor who could move around freely. However, even if the disease was introduced through another route, the staff were likely to have played a key role in the transmission of the disease (e.g., through contact with caregivers or healthcare providers) [22]. Therefore, our results suggest that it is necessary to encourage vaccination among staff.
- Previous studies have reported that regardless of the origin of the outbreak, staff members continued the chain of infection during infectious disease outbreaks at nursing facilities [23−25]. This is also evident from the fact that healthcare-associated infections have become a standard categorization used when classifying infectious diseases. To prevent the spread of infectious diseases transmitted through contacts, the chain of infection must be broken at the level of healthcare workers. This can be achieved through various interventions, such as hand hygiene and mask-wearing. However, for infectious diseases that are preventable by vaccination, such as COVID-19, vaccination can be one of the most effective interventions to break the chain of infection.
- In addition, conducting periodic screening tests for COVID-19 at high-risk facilities among a wider range of people could have reduced the scale of the epidemic. Since South Korea’s periodic screening tests for COVID-19 at high-risk facilities only targeted employees of the facilities, asymptomatic infections in patients of Hospital X were not quickly recognized. Considering that an asymptomatic infection originating from employees could infect patients, and vulnerable patients demonstrate faster onset of symptoms, screening of patients or residents of high-risk facilities would have helped reduce the size of the outbreak.
- Another implication that can be derived from this study is that nursing hospitals also need a systematic infection control program. The importance of infection control is emerging due to the historically unprecedented COVID-19 pandemic. The COVID-19 pandemic situation revealed that more thorough infection control is needed in nursing hospitals because they are facilities where a large number of vulnerable people are in close proximity. Currently, in Korea, it is not mandatory to designate a person in charge of infection control in nursing hospitals; therefore, improvements in this area are needed.
- The efficacy of the Oxford-AstraZeneca vaccine has already been demonstrated in clinical trials [7,26,27] and in studies based in the United Kingdom, the first country in the world to start vaccinating its citizens. According to a VE study conducted among British healthcare workers, COVID-19 vaccination had a preventive effect against the Alpha variant [28]. Another study in the United Kingdom, on patients aged ≥80 years, reported that COVID-19 vaccination reduced the risks of both infection and serious disease progression [29]. Therefore, to reduce the burden of the COVID-19 pandemic, more extensive vaccination should be performed, and the active vaccination of healthcare workers is essential to protect the residents and patients of medical facilities.
- However, the VE of our study is higher than reported in previous studies. According to a cohort study conducted in England, which involved 750 participants aged 50 to 89 years, the VE in participants who were not previously infected and were vaccinated with the first dose of the AstraZeneca vaccine ranged from 43% to 55% [30]. Another study conducted in England showed a 78% reduction in risk in the vaccinated population [31]. The difference in VE between previous studies and our study may have been because the sample size of our study was insufficient to calculate a stable RR, as shown by the wide confidence interval (Table 3). The lack of an appropriate sample size may have led to an overestimation of the VE.
- This study had some limitations. First, the source of the infection could not be identified during the epidemiological investigation; thus, the exact origin of the outbreak could not be established. Since most of the cases were asymptomatic, it was difficult to determine the relationship between cases, and the high proportion of inpatients among cases hindered the ability to obtain accurate information on symptoms. The other limitation of our study is the likelihood that VE was overestimated, which may have been due to the small sample size of our study (n=19). The level of exposure or severity of inpatient cases may have also resulted in overestimation. However, the level of exposure of inpatients was estimated by indirect measures, such as the testimony of medical staff and caregivers, since most inpatients were not able to explain their own status or experience. Furthermore, the underlying diseases and severity of the inpatients in ward E were not fully collected since the investigation of the medical information of people who were not confirmed as COVID-19 cases was limited.
- Nevertheless, our study provided meaningful results on the effectiveness of the Oxford-AstraZeneca vaccine, as most previous studies have focused on the Pfizer vaccine. This is also the first study in South Korea to evaluate VE based on the results of an on-site epidemiological investigation. When more vaccination-related data become available in the future, future studies on VE can be conducted on larger populations in South Korea and in other countries where vaccinations have been administered [32,33].
Discussion
-
Ethics Approval
This study was approved by the Institutional Review Board of Seoul National University Bundang Hospital (No. X-2108-700-902) and performed in accordance with the principles of the Declaration of Helsinki. The requirement for informed consent was waived because of the retrospective nature of this study.
-
Conflicts of Interest
The authors have no conflicts of interest to declare.
-
Funding
None.
-
Availability of Data
The datasets are not publicly available but are available from the corresponding author upon reasonable request.
-
Authors’ Contributions
Conceptualization: CK; Data curation: CK; Formal analysis: CK; Investigation: GK, SGK; Methodology: CK, HL; Visualization: CK; Writing–original draft: CK; Writing–review & editing: all authors.
-
Additional Contributions
Special thanks to Kunhee Park, head of the Gyeonggi Infectious Disease Control Center, for generous support and encouragement to infectious disease investigators.
Article information
Data are presented as vaccinated n/total n (%) or n (%).
Vaccinated, people who received the first dose of the Oxford-AstraZeneca coronavirus disease 2019 vaccine (ChAdOx1-S); patient, people who were admitted to ward E of Hospital X from May 5, 2021 to June 8, 2021; staff member, nurses and caregivers who worked at ward E of Hospital X from May 5, 2021 to June 8, 2021.
| Vaccination status |
Infection status |
Risk | Vaccine effectiveness (%) | p | |
|---|---|---|---|---|---|
| Infected (n=19) | Uninfected (n=36) | ||||
| Vaccinated | 1 | 29 | 0.03 | 95.3 (67.7–99.3)a) | <0.05 |
| Unvaccinated | 18 | 7 | 0.72 | - | - |
- 1. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497−506.ArticlePubMedPMC
- 2. World Health Organization (WHO). COVID-19-China [Internet]. Geneva: WHO; 2020 [cited 2022 Apr 4]. Available from: https://www.who.int/emergencies/disease-outbreak-news/item/2020-DON233.
- 3. Hamid S, Mir MY, Rohela GK. Novel coronavirus disease (COVID-19): a pandemic (epidemiology, pathogenesis and potential therapeutics). New Microbes New Infect 2020;35:100679. ArticlePubMedPMC
- 4. Dighe A, Cattarino L, Cuomo-Dannenburg G, et al. Response to COVID-19 in South Korea and implications for lifting stringent interventions. BMC Med 2020;18:321. ArticlePubMedPMC
- 5. Jo W, Chang D, You M, et al. A social network analysis of the spread of COVID-19 in South Korea and policy implications. Sci Rep 2021;11:8581. ArticlePubMedPMC
- 6. Shim E, Tariq A, Chowell G. Spatial variability in reproduction number and doubling time across two waves of the COVID-19 pandemic in South Korea, February to July, 2020. Int J Infect Dis 2021;102:1−9.ArticlePubMed
- 7. Knoll MD, Wonodi C. Oxford-AstraZeneca COVID-19 vaccine efficacy. Lancet 2021;397:72−4.ArticlePubMed
- 8. Baraniuk C. Covid-19: How the UK vaccine rollout delivered success, so far. BMJ 2021;372:n421. ArticlePubMed
- 9. Ministry of Health and Welfare (MOHW). Free vaccination for all citizens of COVID-19. Sejong: MOHW; 2021. Korean.
- 10. Choi Y, Kim JS, Kim JE, et al. Vaccination prioritization strategies for COVID-19 in Korea: a mathematical modeling approach. Int J Environ Res Public Health 2021;18:4240. ArticlePubMedPMC
- 11. Jung J. Preparing for the coronavirus disease (COVID-19) vaccination: evidence, plans, and implications. J Korean Med Sci 2021;36:e59.ArticlePubMedPMC
- 12. Kim T. Improving preparedness for and response to coronavirus disease 19 (COVID-19) in long-term care hospitals in Korea. Infect Chemother 2020;52:133−41.ArticlePubMedPMC
- 13. Olliaro P, Torreele E, Vaillant M. COVID-19 vaccine efficacy and effectiveness-the elephant (not) in the room. Lancet Microbe 2021;2:e279−80.ArticlePubMedPMC
- 14. Olliaro P. What does 95% COVID-19 vaccine efficacy really mean? Lancet Infect Dis 2021;21:769. Article
- 15. Korea Disease Control and Prevention Agency (KDCA). Guidelines for COVID-19 virus response. 10th ed. Cheongju: KDCA; 2021. Korean.
- 16. Dhouib W, Maatoug J, Ayouni I, et al. The incubation period during the pandemic of COVID-19: a systematic review and meta-analysis. Syst Rev 2021;10:101. ArticlePubMedPMC
- 17. Khalili M, Karamouzian M, Nasiri N, et al. Epidemiological characteristics of COVID-19: a systematic review and meta-analysis. Epidemiol Infect 2020;148:e130.ArticlePubMed
- 18. Hong KH, Lee SW, Kim TS, et al. Guidelines for laboratory diagnosis of coronavirus disease 2019 (COVID-19) in Korea. Ann Lab Med 2020;40:351−60.ArticlePubMedPMC
- 19. Pascucci D, Nurchis MC, Sapienza M, et al. Evaluation of the effectiveness and safety of the BNT162b2 COVID-19 vaccine in the vaccination campaign among the health workers of Fondazione Policlinico Universitario Agostino Gemelli IRCCS. Int J Environ Res Public Health 2021;18:11098. ArticlePubMedPMC
- 20. Lopez Bernal J, Andrews N, Gower C, et al. Effectiveness of covid-19 vaccines against the B.1.617.2 (Delta) variant. N Engl J Med 2021;385:585−94.ArticlePubMed
- 21. Korea Disease Control and Prevention Agency (KDCA). Guidelines for COVID-19 mutant starin patients management. Cheongju: KDCA; 2021. Korean.
- 22. Kim C, Choi G, Park SY, et al. Experience of a COVID-19 outbreak response in a general hospital in Gyeonggi Province, Korea. Epidemiol Health 2021;43:e2021083.ArticlePubMedPMC
- 23. Dooling KL, Crist MB, Nguyen DB, et al. Investigation of a prolonged Group A Streptococcal outbreak among residents of a skilled nursing facility, Georgia, 2009-2012. Clin Infect Dis 2013;57:1562−7.ArticlePubMed
- 24. Deutscher M, Schillie S, Gould C, et al. Investigation of a group a Streptococcal outbreak among residents of a long-term acute care hospital. Clin Infect Dis 2011;52:988−94.ArticlePubMed
- 25. Louie JK, Yagi S, Nelson FA, et al. Rhinovirus outbreak in a long term care facility for elderly persons associated with unusually high mortality. Clin Infect Dis 2005;41:262−65.ArticlePubMed
- 26. Halim A, Tjhin Y. COVID-19 vaccination efficacy and safety literature review. J Clin Med Res 2021;3:1−10.Article
- 27. Hung IFN, Poland GA. Single-dose Oxford-AstraZeneca COVID-19 vaccine followed by a 12-week booster. Lancet 2021;397:854−5.ArticlePubMedPMC
- 28. Hall VJ, Foulkes S, Saei A, et al. COVID-19 vaccine coverage in health-care workers in England and effectiveness of BNT162b2 mRNA vaccine against infection (SIREN): a prospective, multicentre, cohort study. Lancet 2021;397:1725−35.PubMedPMC
- 29. Lopez Bernal J, Andrews N, Gower C, et al. Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines on covid-19 related symptoms, hospital admissions, and mortality in older adults in England: test negative case-control study. BMJ 2021;373:n1088. ArticlePubMed
- 30. Amirthalingam G, Bernal JL, Andrews NJ, et al. Serological responses and vaccine effectiveness for extended COVID-19 vaccine schedules in England. Nat Commun 2021;12:7217. ArticlePubMedPMC
- 31. Glampson B, Brittain J, Kaura A, et al. Assessing COVID-19 vaccine uptake and effectiveness through the North West London vaccination program: retrospective cohort study. JMIR Public Health Surveill 2021;7:e30010.ArticlePubMedPMC
- 32. Vasileiou E, Simpson CR, Robertson C, et al. Effectiveness of first dose of COVID-19 vaccines against hospital admissions in Scotland: national prospective cohort study of 5.4 million people [Preprint]. Posted 2021 Feb 19. SSRN. https://dx.doi.org/10.2139/ssrn.3789264.
- 33. Dagan N, Barda N, Kepten E, et al. BNT162b2 mRNA covid-19 vaccine in a nationwide mass vaccination setting. N Engl J Med 2021;384:1412−23.ArticlePubMed
References
Figure & Data
References
Citations

- COVID-19 Vaccination in Korea: Past, Present, and the Way Forward
Eliel Nham, Joon Young Song, Ji Yun Noh, Hee Jin Cheong, Woo Joo Kim
Journal of Korean Medical Science.2022;[Epub] CrossRef


 PubReader
PubReader Cite
Cite