Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 14(2); 2023 > Article
-
Original Article
Risk factors for deaths associated with COVID-19 according to the cause of death classification in Republic of Korea -
Na-Young Kim
 , Seong-Sun Kim
, Seong-Sun Kim , Hyun Ju Lee
, Hyun Ju Lee , Dong Hwi Kim
, Dong Hwi Kim , Boyeong Ryu
, Boyeong Ryu , Eunjeong Shin
, Eunjeong Shin , Donghyok Kwon
, Donghyok Kwon
-
Osong Public Health and Research Perspectives 2023;14(2):89-99.
DOI: https://doi.org/10.24171/j.phrp.2022.0312
Published online: April 18, 2023
Central Disease Control Headquarters, Korea Disease Control and Prevention Agency, Cheongju, Republic of Korea
- Corresponding author: Donghyok Kwon Central Disease Control Headquarters, Korea Disease Control and Prevention Agency, 187 Osongsaengmyeong 2-ro, Osong-eup, Heungdeok-gu, Cheongju 28159, Republic of Korea E-mail: vethyok@korea.kr
© 2023 Korea Disease Control and Prevention Agency.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
- 1,432 Views
- 93 Download
Abstract
-
Objectives
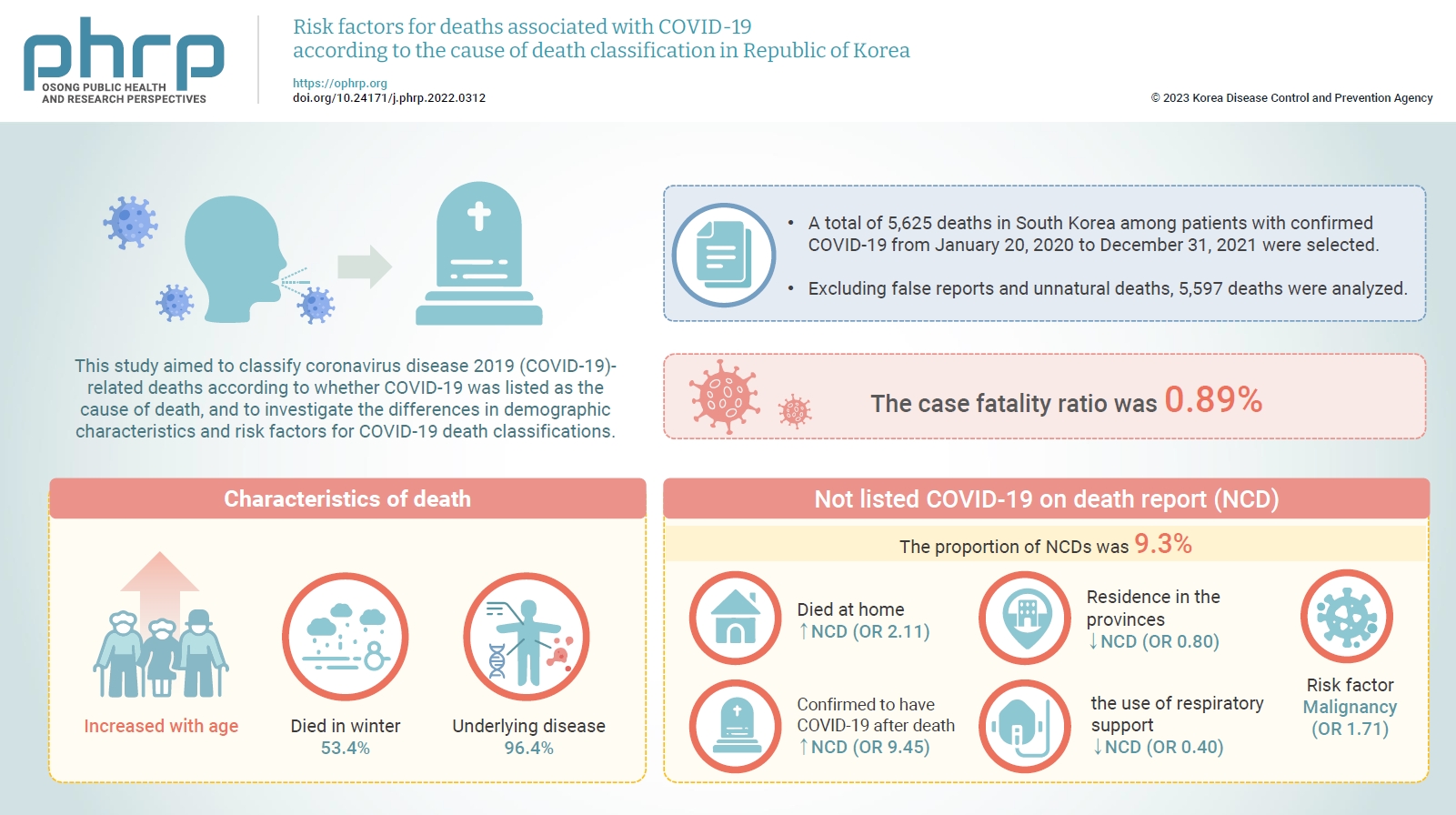
- This study aimed to classify coronavirus disease 2019 (COVID-19)-related deaths according to whether COVID-19 was listed as the cause of death, and to investigate the differences in demographic characteristics and risk factors for COVID-19 death classifications.
-
Methods
- A total of 5,625 deaths in South Korea among patients with confirmed COVID-19 from January 20, 2020 to December 31, 2021 were selected. Excluding false reports and unnatural deaths, 5,597 deaths were analyzed. Based on death report data, deaths were classified according to whether the cause of death was listed as COVID-19 (CD) or not (NCD). The epidemiological characteristics and causes of deaths were investigated using descriptive, univariate, and multivariate statistical analyses. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated to analyze the risk factors.
-
Results
- The case fatality ratio was 0.89% and increased with age. Additionally, 96.4% of the subjects had an underlying disease, and 53.4% died in winter. The proportion of NCDs was 9.3%, of whom 19.1% died at home and 39.0% were confirmed to have COVID-19 after death. Malignant neoplasms (102/416 vs. 637/4,442; OR, 1.71; 95% CI, 1.36−2.16; p<0.001) were significantly associated with NCD.
-
Conclusion
- This is the first study to analyze risk factors by cause of death using COVID-19 death report data in South Korea. These results are expected to be used as evidence for establishing a death monitoring system that can collect timely information in a new infectious disease pandemic.
- Since the first case of coronavirus disease 2019 (COVID-19) was confirmed in December 2019, 627 million confirmed cases of COVID-19 have been reported and 6.5 million deaths have occurred worldwide as of October 30, 2022 [1]. In South Korea, 25,538,799 cases have been confirmed and 29,158 deaths have been reported [2].
- Numerous studies have demonstrated that age and underlying diseases are major risk factors for death from COVID-19 [3–5]. In the United States (US), 80% of COVID-19 deaths at the beginning of the COVID-19 pandemic in 2020 occurred in people aged 65 years or older [5]. In Brazil, 75% of COVID-19 deaths in 2020 were among people aged 60 years or older [6]. In Italy, one of the countries with the highest COVID-19-related mortality since the beginning of the COVID-19 pandemic, more than 94% of COVID-19 deaths from February to September 2020 occurred in elderly people aged 60 years or older, and at least 70% had an underlying disease [7]. In South Korea, more than 90% of COVID-19 deaths took place in elderly people in their 60s or older [2].
- The higher proportions of confirmed cases and deaths among elderly people with underlying diseases can lead to another problem—namely, the capacity of national health systems could be temporarily exceeded. In addition, because it is difficult to accurately determine whether the direct cause of death is COVID-19 infection or the aggravation of underlying diseases due to COVID-19 [8–10], some countries have suggested that caution should be taken when interpreting COVID-19-related deaths [8,11].
- Epidemiological studies regarding the exact number of deaths are key measures that are widely used as surrogate variables to accurately identify the most vulnerable groups in a country and assess the severity of diseases [12]. In particular, mortality data play an essential role in public health decision-making or policy-making regarding the magnitude and duration of necessary interventions [13,14]. As proper reporting on deaths during the COVID-19 pandemic is very useful for effectively planning public health control measures [15,16], various countries have counted COVID-19 deaths for the purpose of infectious disease surveillance.
- The World Health Organization (WHO) recommends that a death in a probable or confirmed COVID-19 case be reported as a death due to COVID-19, unless there is a clear alternative cause of death that cannot be related to COVID-19 (e.g., unnatural deaths) [17]. According to the US Centers for Disease Control and Prevention, a death should be reported as related to COVID-19 when a confirmed COVID-19 infection results in death, or when a death in a suspected or presumed COVID-19 case without laboratory results is recorded as a death due to COVID-19 on the death certificate by a medical professional [18]. In the UK, deaths within 28 days of the confirmation of COVID-19 infection are counted as COVID-19-related deaths, and cases where the cause of death is clearly determined to be COVID-19 by a medical professional are also recommended to be counted as deaths due to COVID-19 [10]. The official global number of COVID-19 deaths (i.e., daily mortality) is provided by the WHO COVID-19 dashboard. However, it is not clear whether cases of COVID-19 that are confirmed after death are included in the count of COVID-19 deaths. In South Korea, the COVID-19 death counting criteria are generally similar to the WHO criteria, but COVID-19 cases confirmed through postmortem testing and cases where COVID-19 testing was performed before death but COVID-19 was confirmed after death are also included in the number of deaths due to COVID-19 [19].
- Despite the establishment of these death counting systems or criteria in each country, specific aspects of the COVID-19 pandemic have acted as a significant obstacle to accurately counting COVID-19 deaths [20]. Some deaths associated with COVID-19 in the US have not been classified as COVID-19 deaths [20]. In Brazil, it was difficult to accurately determine the number of deaths associated with COVID-19 due to the limited availability of diagnostic tests in the early stages of the pandemic [21,22]. In addition, issues related to the classification of deaths have been raised, as India lacks complete death certificates [23], and Indonesia is known to have under-reported deaths due to incomplete certification of deaths [24]. A study also identified many errors related to causes of death on death certificates in Iran [25]. Therefore, research emphasizing the importance of accurate death reporting according to an analysis of the underlying or direct cause of death is needed.
- This study aimed to classify deaths in individuals with COVID-19 according to whether COVID-19 was listed as the cause of death, using COVID-19-related death reporting data and epidemiological information in South Korea, and to analyze differences in the demographic characteristics of COVID-19 deaths and risk factors for whether a death was classified as being caused by COVID-19.
Introduction
- Subjects and Case Definition
- Among patients with confirmed COVID-19 between January 20, 2020 and December 31, 2021, a total of 5,625 deaths that were registered in the Korea Disease Control and Prevention Agency (KDCA) COVID-19 information management system were selected as the subjects of this study. In South Korea, the data of COVID-19 cases and deaths reported by healthcare institutions or local public health centers are registered in the KDCA COVID-19 information management system according to Article 11 of the Infectious Disease Control and Prevention Act.
- A patient with confirmed COVID-19 was defined as a person in whom, during the investigation period, severe acute respiratory syndrome coronavirus 2 viral genes in a specimen collected from the upper respiratory tract were detected using reverse-transcription polymerase chain reaction in accordance with the laboratory diagnostic criteria, regardless of clinical symptoms [19]. “Deceased” referred to people who had no alternative cause of death related to COVID-19, such as unnatural deaths, (1) people who were confirmed to be infected with COVID-19 and died during the isolation period, (2) people who were confirmed to be infected with COVID-19 after death, or (3) people who died after release from COVID-19-related isolation for whom a medical opinion was available regarding whether the death was related to COVID-19, and then confirmed the fact of death with the respective local government. Critically ill patients referred to those who were treated in isolation with respiratory support, such as non-invasive ventilation, high-flow oxygen therapy, invasive ventilation, extracorporeal membrane oxygenation, or continuous renal replacement therapy.
- The variables used in this study included epidemiological information (sex, age group, region, the presence or absence and type of underlying diseases, vaccination history, respiratory support history, place of death, date of COVID-19 confirmation, and date of death), and items regarding the cause of death (a) the direct cause of death, (b) causes of (a), (c) causes of (b), (d) causes of (c), and other physical conditions except for causes of death (a)–(d).
- The reported deaths were classified as those listed as being caused by COVID-19 (CD) and those not listed as being caused by COVID-19 in the death reports (NCD). A single author carried out the classification of deaths as CD or NCD.
- Age was categorized as under or older than 60 years, and regions were divided into metropolitan cities and provinces. Metropolitan cities included Seoul, Busan, Daegu, Incheon, Gwangju, Daejeon, Ulsan, Sejong, and Jeju, and the provinces included Gyeonggi-do, Gangwon-do, Chungcheongbuk-do, Chungcheongnam-do, Jeollabuk-do, Jeollanam-do, Gyeongsangbuk-do, and Gyeongsangnam-do.
- All analyses were performed based on the regions where COVID-19 tests were performed and cases were confirmed. Cases where a death report was requested to be withdrawn due to a false report by the local authority responsible for reporting deaths and cases that were confirmed as unnatural deaths were excluded from the analysis.
- Classification of the Cause of Death
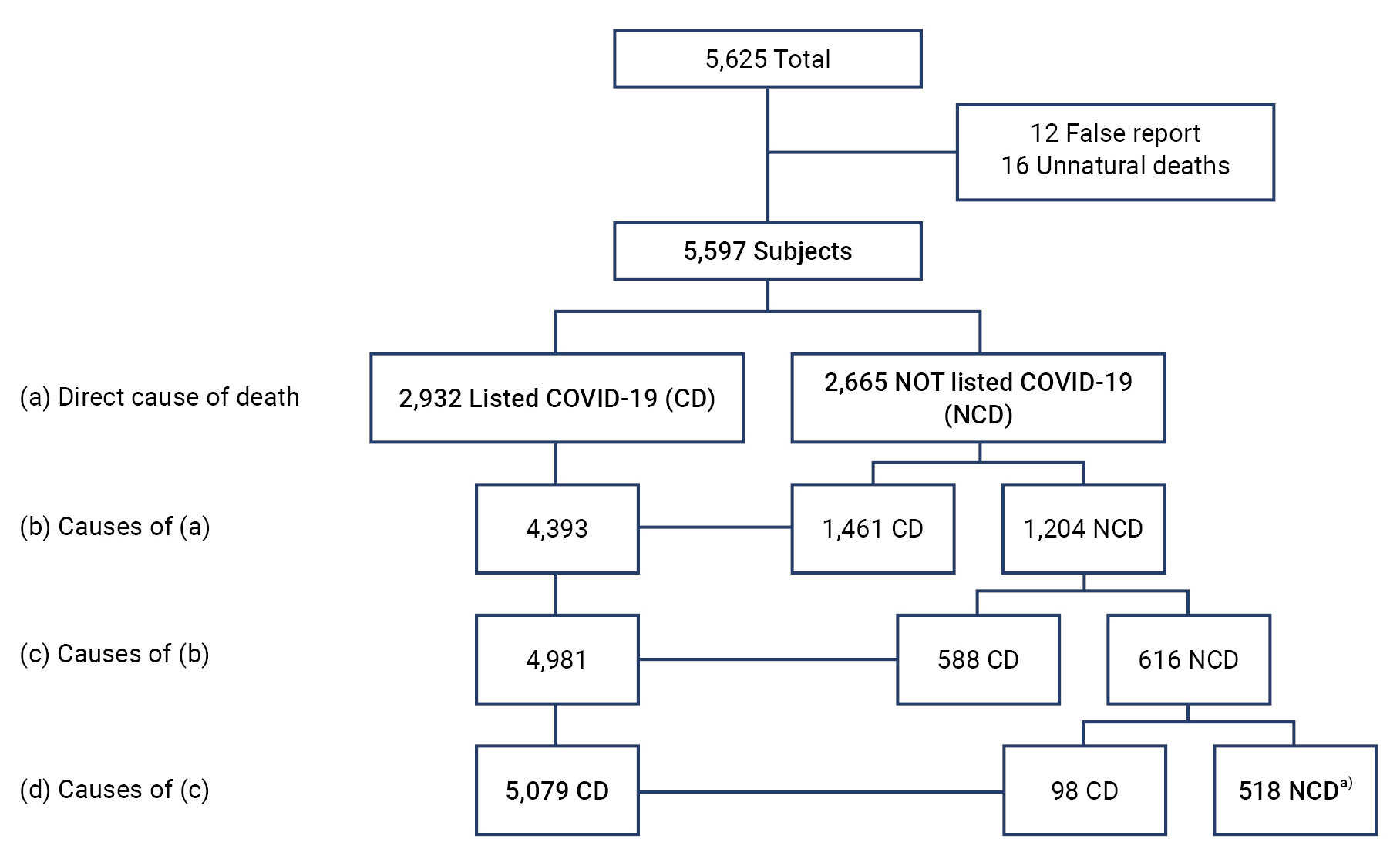
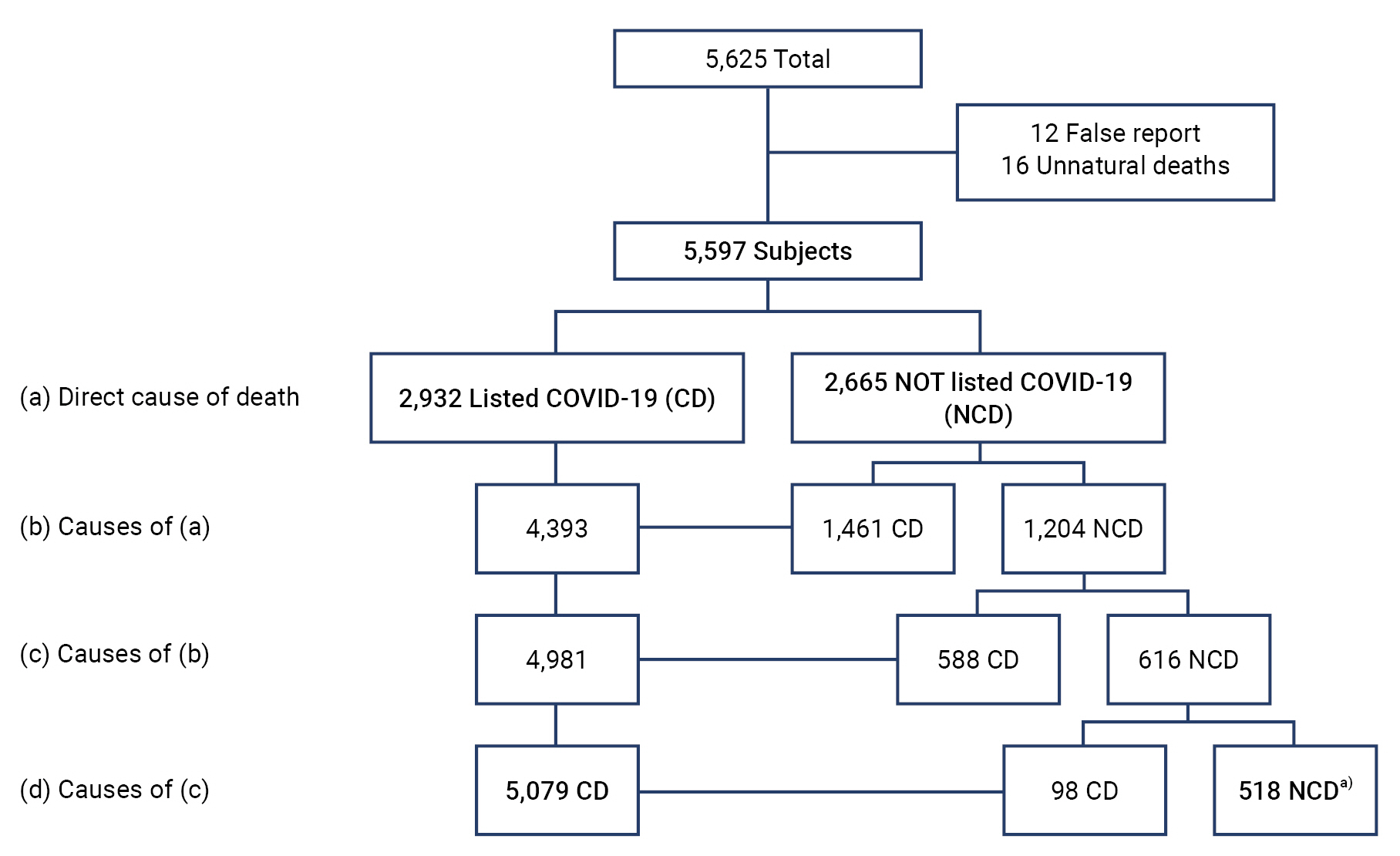
- From the 5,625 reported deaths, 5,597 were finally selected for analysis, excluding 12 false reports and 16 confirmed unnatural deaths.
- Deaths were categorized into 2 groups based on the information in the death reporting data according to the algorithm presented in Figure 1: CD (if the cause of death was listed as COVID-19 in the respective death report) or NCD (if the cause of death was not listed as COVID-19). The NCD group included cases with unknown and missing causes of death in the COVID-19 death reporting data.
- Statistical Analysis
- A descriptive statistical analysis was performed to investigate the epidemiological characteristics and causes of death of the deceased people, and the distribution of deaths according to sex, age group, area, and underlying diseases was analyzed. Univariate analysis of the relationships between each epidemiological variable and the CD and NCD groups was conducted. Multivariate logistic regression analysis was carried out using statistically significant variables from the univariate analysis. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated to analyze risk factors for the classification of the causes of death (significance level: p<0.05). All analyses were performed using Microsoft Excel 2018 and IBM SPSS ver. 23.0 for Windows (IBM Corp.).
- Ethics Statement
- This study was approved by the Institutional Review Board of KDCA (IRB No: 2022-11-05-PE-A).
Materials and Methods
- Epidemiological Characteristics
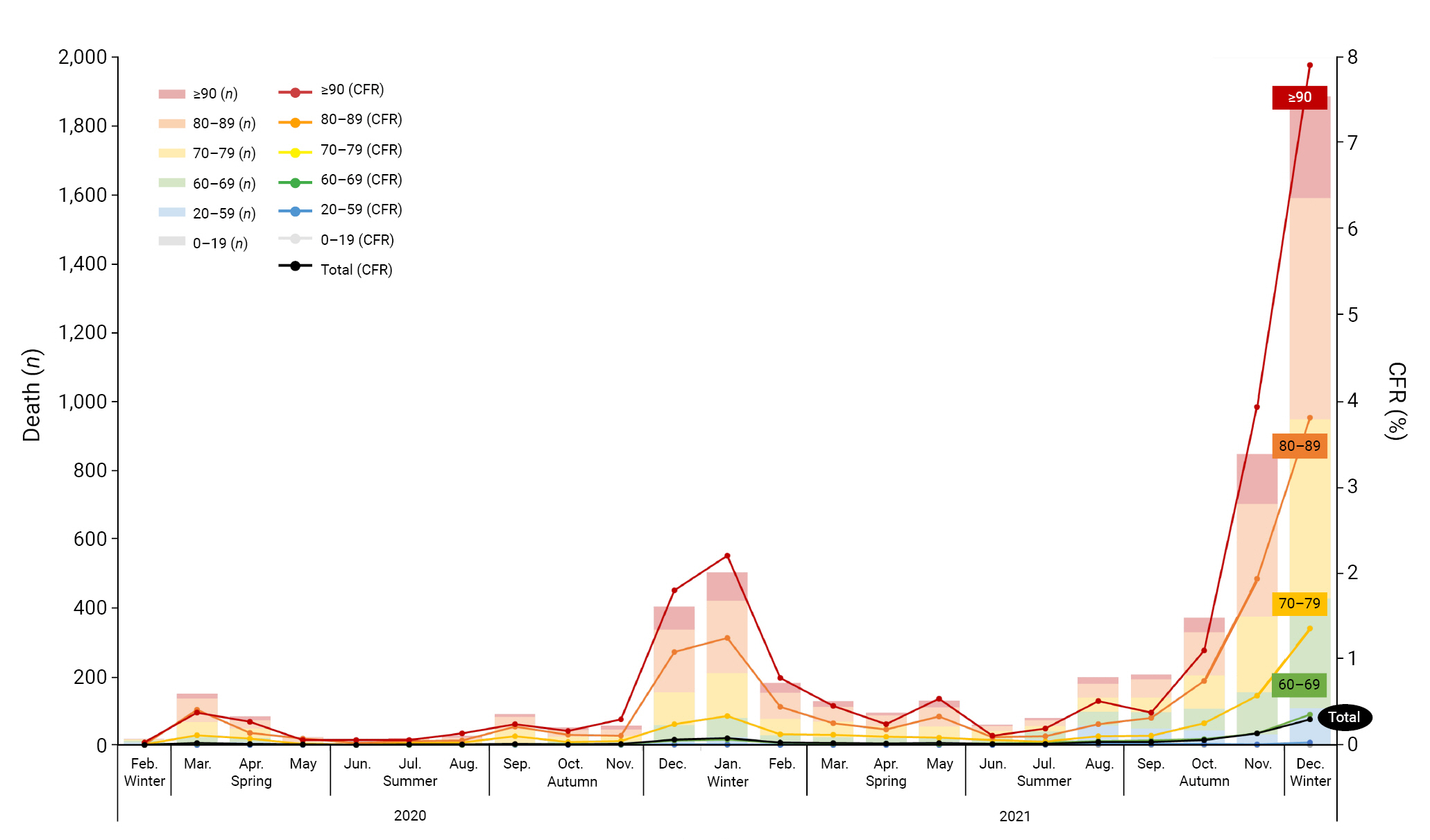
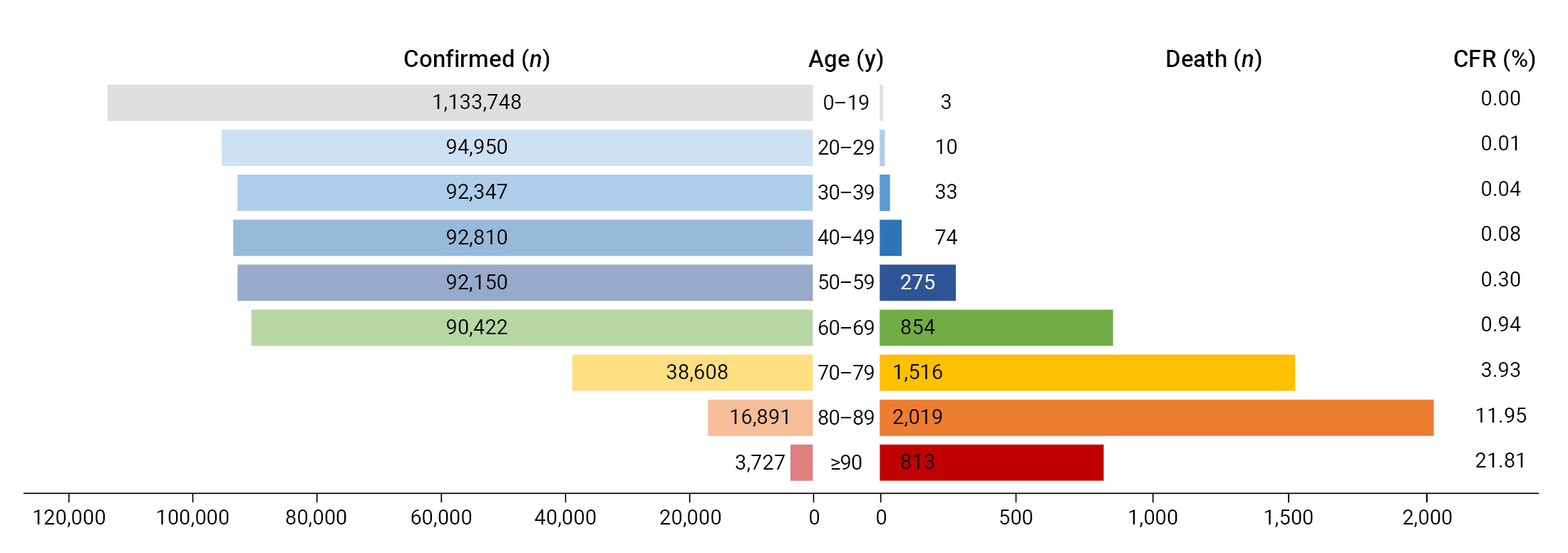
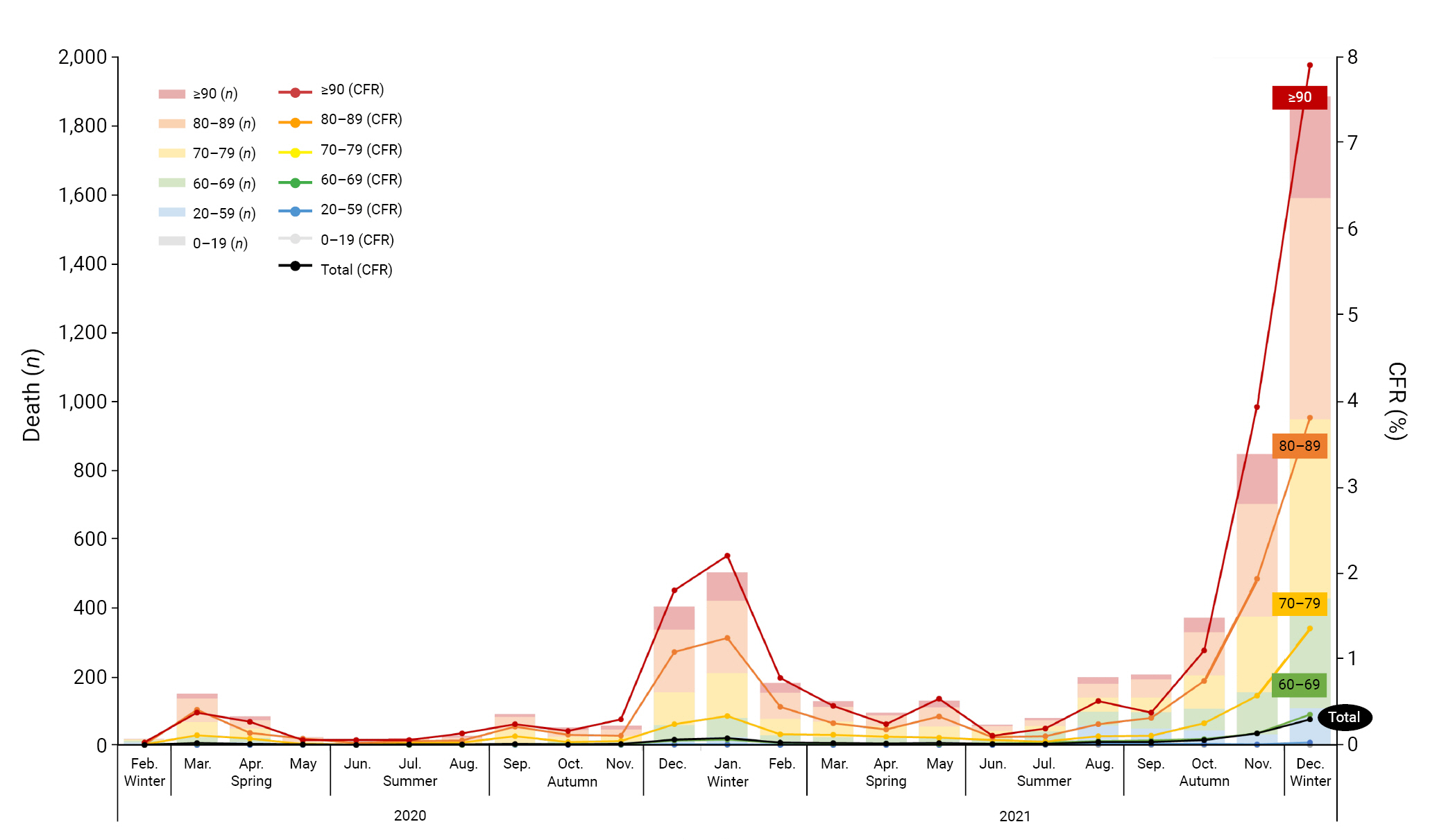
- The total number of confirmed cases during the investigation period was 635,253, from which 5,625 deaths were reported. The case fatality ratio (CFR) was 0.89%. Individuals in their 60s or older accounted for 5,202 of the 5,597 deaths (92.9%) investigated, and the proportion of those in their 80s was the highest (n=2,019, 36.1%). The CFR increased with age, and the mortality rates of those in their 60s, 70s, 80s, and 90s or older were 0.94%, 3.93%, 11.95%, and 21.81%, respectively (Table 1, Figure 2).
- In addition, 96.4% of deaths (n=5,395) occurred in people with an underlying disease, the most common of which was cardiovascular disease (n=3,739, 69.3%). Furthermore, 95.6% of deaths (n=5,351) took place in medical institutions. There were 367 cases (6.6%) in which COVID-19 was confirmed after death, 2,971 patients received critical care before death (53.1%) (Table 1), and 53.4% (n=2,987) died in the winter, between December and February (Figure 3).
- Characteristics of COVID-19 Deaths According to the Classification
- The number of those whose cause of death was listed as COVID-19 (i.e., the CD group) was 5,079 (90.7%), whereas the number of those whose cause of death was not listed as COVID-19 (i.e., the NCD group) was 518 (9.3%). In the NCD group, 122 people (2.2%) had an unknown cause of death and the cause of death was left blank, with no details related to the cause of death, for 8 people (0.1%) (Table 1, Figure 1).
- The number of men was higher than women in both groups (51.3% vs. 54.1%), and there was no significant difference in age between the groups (median, 80 vs. 80 years; mean, 77.9 vs. 76.9 years; interquartile range [IQR], 71−86 years vs. 69−86 years), and the number of those in their 80s was the highest. By region, the number of deaths was highest in Seoul and Gyeonggi-do (32.2% vs. 31.7% and 33.5% vs. 24.1% in the CD and NCD groups, respectively). At least 1 underlying disease was recorded in 5,395 deaths, and the proportion of those with 4 or more underlying diseases was 19.2% in the CD group and 16.6% in the NCD group. The most common underlying disease was cardiovascular disease, as 67.7% of people in the CD group and 58.5% of those in the NCD group had this condition. The proportion of those who had received no vaccination or only 1 dose of vaccination was 74.6% in the CD group and 74.5% in the NCD group, with no significant difference between the groups. The most common place of death was medical institutions (97.3% in the CD group and 78.6% in the NCD group).
- Of the deceased, 53.1% received critical care (56.3% in the CD group and 21.6% in the NCD group). Meanwhile, 367 individuals (6.6%) were confirmed to have COVID-19 after death. Of those cases, 165 (3.2%) were in the CD group and 202 (39.0%) were in the NCD group, indicating that a postmortem diagnosis of death was more common in the NCD group than in the CD group.
- The average time interval from the date of COVID-19 confirmation to the date of death in 5,230 deaths, excluding the 367 deaths where COVID-19 infection was confirmed after death, was 16.2 days, with 16.5 days in the CD group and 11.9 days in the NCD group (median, 13 days vs. 8 days; IQR, 7−21 vs. 2−16 days).
- Comparison of Epidemiological Variables for COVID-19-Related Deaths
- Univariate and multivariate analyses were conducted to evaluate the relationships between epidemiological variables and COVID-19-related deaths. Statistically significant relationships were found for region, place of death, respiratory support, and COVID-19 confirmation after death. In terms of region, Busan (OR, 1.59; 95% CI, 1.09–2.32; p=0.021), Incheon (OR, 1.53; 95% CI, 1.04–2.26; p=0.041), Daejeon (OR, 2.72; 95% CI, 1.82–4.07; p<0.001), Chungcheongbuk-do (OR, 1.84; 95% CI, 1.07–3.17; p=0.038), and Jeju (OR, 8.56; 95% CI, 2.84–25.76; p<0.001) showed significant relationships with the NCD group. Gyeonggi-do (OR, 0.73; 95% CI, 0.57–0.93; p=0.014) was significantly associated with the CD group. NCD cases were more likely to die at home (OR, 9.85; 95% CI, 7.42–13.09; p<0.001) but less likely to receive respiratory support (OR, 0.21; 95% CI, 0.17–0.27; p<0.001) than CD cases. COVID-19 confirmation after death was also more common in the NCD group (OR, 19.0; 95% CI, 15.05–24.08; p<0.001) (Table 2).
- Multivariate analysis was performed using the variables that were statistically significant in the univariate analysis. The NCD group showed a significantly higher risk of death at home (OR, 2.11; 95% CI, 1.49–3.00; p<0.001) and COVID-19 confirmation after death (OR, 9.45; 95% CI, 7.20–12.40; p<0.001) than the CD group. Residence in the provinces (OR, 0.80; 95% CI, 0.65–0.98; p=0.029) and the use of respiratory support (OR, 0.40; 95% CI, 0.32–0.51; p<0.001) were significantly less common in NCD cases than in CD cases (Table 3).
- Comparison of Underlying Diseases as Risk Factors for the Classification of COVID-19 Deaths
- In a further analysis, cardiovascular disease (303/215 vs. 3,436/1,643; OR, 0.67; 95% CI, 0.56–0.81; p<0.001) and endocrine disease (184/334 vs. 2,100/2,979; OR, 0.78; 95% CI, 0.65–0.94; p=0.012) were more common in the CD group than in the NCD group, while malignant neoplasms (102/416 vs. 637/4,442; OR, 1.71; 95% CI, 1.36–2.16; p<0.001) showed a significant association with the NCD group (Table 4).
Results
- Since the WHO declared the COVID-19 outbreak as a public health emergency of international concern in January 2020 [26] and a pandemic in March 2020, COVID-19 has spread around the world. COVID-19 is a life-threatening infectious disease that has had major effects on people’s lives [27]. In 2020, when the COVID-19 outbreak began, COVID-19 was the top cause of death in Brazil [6], and it was the third leading cause of death in the US [28]. Although COVID-19 did not rank high as a cause of death in South Korea, it was announced that the number of deaths due to COVID-19 increased by 429.5% from 2020 to 2021 [29].
- Studies regarding deaths due to COVID-19 have focused mainly on hospitalized patients, and several risk factors for death due to COVID-19 have been identified [6,30–32]. However, the presence of at least 1 risk factor did not meaningfully distinguish between the CD and NCD groups. The major risk factors for COVID-19-related death are age and underlying diseases, which is why the CD group predominantly contained elderly patients with underlying diseases. In Germany, more than 40% of those who died from COVID-19 had at least 1 underlying disease, and there was no significant difference in risk factors between the CD and NCD groups [8].
- In South Korea, 96.4% of COVID-19 deaths occurred in those who had an underlying disease. However, no previous studies have investigated the causes of death in deceased COVID-19 patients in South Korea. To address that knowledge gap, this study analyzed the epidemiological characteristics of COVID-19-related deaths and explored underlying diseases as risk factors by classifying all COVID-19-related deaths between 2020 and 2021 according to whether or not the cause of death was listed as COVID-19. The CFR in COVID-19 cases increased with age in Europe and the US [5,7,8]. Similarly, the number of deaths among elderly people with COVID-19 was high in South Korea, and the CFR also increased with age. Therefore, it is necessary to continue to implement COVID-19 prevention and control measures for elderly people who are more vulnerable to disease transmission and are at a high risk of death. In particular, it is necessary to prepare the public health response for the winter, when many deaths occur. According to previous studies, symptoms such as dyspnea, pneumonia, and cough at COVID-19 diagnosis were significantly associated with COVID-19 being reported as the cause of death, indicating that these symptoms served as predictors of disease severity and death [8]. Although information on the definite diagnosis of the deceased and the symptoms at the time of death could not be identified, pneumonia was listed as the case of death for 52.5% of the deceased. However, we could not confirm whether their symptoms were directly caused by COVID-19 infection or due to aggravation of other underlying diseases.
- Through this study, we found that the NCD group had a higher likelihood of dying at home and having COVID-19 infection confirmed after death than the CD group. The information on the patients who died before COVID-19 results were available may not have been timely enough to determine the correct cause of death. Furthermore, malignant neoplasms as underlying diseases were more frequent in NCD cases than in CD cases, indicating that some of the NCD cases were likely due to the exacerbation of malignant neoplasms rather than COVID-19. In addition, we found that the CD cases were more likely to have received critical care and had a longer interval from the day of diagnosis to death. We suggest that underlying diseases such as neoplasms could aggravate COVID-19-related deaths, which was probably an important factor in NCD cases. COVID-19 testing may have been delayed in NCD patients because it was difficult to clinically distinguish between symptoms caused by aggravation of the underlying diseases and COVID-19. Furthermore, the NCD group was less likely than the CD group to show severe respiratory symptoms and might not have required treatment in a hospital, which could explain why they were more likely to die at home. However, it is likely that the results of this study were affected by limitations in reported death information; therefore, further research is needed to elucidate more information on this topic for COVID-19 decedents. Nevertheless, we suggest high risk groups with underlying diseases, such as cancer patients, should be promptly tested for COVID-19. Once COVID-19 is diagnosed, treatment should be administered at an early stage to reduce mortality.
- In this study, 8 cases had no description for any of the death report items. Furthermore, COVID-19 was not included in the death report for about 9.3% of deaths, and for 25.1% of them, the cause of death was not known at all. The rapid increase in the number of deaths in the special circumstances of the COVID-19 pandemic made it difficult to determine the cause of death at the right time when writing a death certificate. The information contained in the death report data varied in quality and did not support a definitive attribution of cause of death in all cases. Therefore, further analysis is needed to determine the quality of death certificates or death registration data.
- In many countries, death certificates are the main source of official death statistics [33]. Accurate death diagnosis and reporting are critical to maintaining accurate and reliable mortality data. Because the quality of death certificate data eventually determines the accuracy of public health mortality data [20], efforts to improve the quality of data regarding suspected causes of death (i.e., efforts to provide complete and logical causal relationships) should be made. In particular, it is necessary to thoroughly educate people (e.g., physicians) on the criteria or guidelines stating that people infected with COVID-19 can die from other underlying diseases or accidents, and such cases are not deaths due to COVID-19. Thus, they are not subject to reporting requirements for deaths related to COVID-19.
- In general, it is difficult to obtain characteristics of infected patients and clinical observations of patients at the population level in the early stages of a pandemic [34]. Thus, determining the exact cause of death is essential for planning prevention and control measures, especially during a pandemic that requires rapid public action [24]. In addition, high-quality death certificates containing correct information enable national health authorities to collect timely and accurate information to assist in the assessment and management of infectious diseases [20]. Therefore, it is necessary for public health agencies to make additional efforts to mitigate the spread of disease by quickly establishing a death counting system and guideline in the early stage of a pandemic or outbreak, and unified standards should be implemented to ensure the accuracy of death statistics and support analyses of those records.
- This study has several limitations. First, because our analysis was based on death report data, it might contain less information than was contained in the corresponding death certificates. Some of the data were incomplete because the information from death reports varied qualitatively and missing data sometimes existed. Second, underlying diseases and causes of death were not analyzed using Korean Classification of Diseases codes. We analyzed epidemic data and information on deaths from death reports in the KDCA COVID-19 information management system. Third, we did not adjust for potential confounding factors, such as COVID-19 variants and vaccine effectiveness. Furthermore, our study cannot provide a definitive explanation of how deaths can be attributed to COVID-19 after infection.
- This is the first study to analyze risk factors for the reported cause of death using COVID-19 death report data in South Korea. The results of this study reconfirm that domestic COVID-19 response strategies and COVID-19 patient management methods, such as COVID-19 diagnostic tests and bed allocations, monitoring of patients’ clinical status, and the provision of COVID-19 treatment, have been formulated based on scientific evidence. As the COVID-19 pandemic has continued for 3 years, COVID-19 variants continue to emerge. Hence, it is necessary to monitor COVID-19 deaths during COVID-19 variant outbreaks. Monitoring COVID-19 deaths can be used as a basis for strengthening COVID-19 prevention and control policies, which can minimize the damage caused by the disease, such as progression to severe illness or death. This study is also expected to be used as evidence for establishing a death counting system or criteria that can collect timely and accurate information in the event of a new infectious disease pandemic or outbreak.
Discussion
- • The number of deaths associated COVID-19 increased with age in South Korea. Therefore, it is necessary to prepare the public health response for elderly people who are at a high risk of death.
- • The group whose cause of death was not listed as COVID-19 in the reports had more deaths at home than in hospitals. And underlying diseases related to malignant neoplasms were frequent.
- • It is necessary for public health agencies to make accurate and timely death statistics and analysis through unified standards by quickly establishing a death counting system or guideline in the early stage of the pandemic.
HIGHLIGHTS
-
Ethics Approval
This study was approved by the Institutional Review Board of KDCA (IRB No: 2022-11-05-PE-A).
-
Conflicts of Interest
The authors have no conflicts of interest to declare.
-
Funding
None.
-
Availability of Data
The data used in this study are protected under the Personal Information Protection Act. The datasets are not publicly available but are available from the corresponding author upon reasonable request.
-
Authors’ Contributions
Conceptualization: NYK, DK; Data curation: NYK; Formal analysis: NYK, HJL, DK; Investigation: NYK, DK; Methodology: all authors; Project administration: DK; Resources: all authors; Software: all authors; Supervision: DK, NYK; Validation: all authors; Visualization: BR, ES; Writing–original draft: NYK; Writing–review & editing: all authors. All authors read and approved the final manuscript.
-
Additional Contributions
We thank the relevant ministries, including those at local and provincial levels (si/do and si/gun/gu), and staff in health centers and hospitals for their efforts in responding to COVID-19 deaths.
Article information
- 1. World Health Organization (WHO). COVID-19 weekly epidemiological update: 116 published 2 November 2022 [Internet]. WHO; 2022 [cited 2022 Nov 2]. Available from: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---2-November-2022.
- 2. Korea Disease Control and Prevention Agency (KDCA). Press release [Internet]. KDCA; 2022 [cited 2022 Dec 1]. Available from: https://kdca.go.kr/board/board.es?mid=a20501010000&bid=0015&list_no=721006&cg_code=&act=vivi&nPage=7. Korean.
- 3. Clift AK, Coupland CA, Keogh RH, et al. Living risk prediction algorithm (QCOVID) for risk of hospital admission and mortality from coronavirus 19 in adults: national derivation and validation cohort study. BMJ 2020;371:m3731. ArticlePubMedPMC
- 4. Williamson EJ, Walker AJ, Bhaskaran K, et al. OpenSAFELY: factors associated with COVID-19 death in 17 million patients. Nature 2020;584:430−6.ArticlePubMedPMCPDF
- 5. CDC COVID-19 Response Team. Severe outcomes among patients with coronavirus disease 2019 (COVID-19)-United States, February 12-March 16, 2020. MMWR Morb Mortal Wkly Rep 2020;69:343−6.ArticlePubMedPMC
- 6. Zimmermann IR, Sanchez MN, Alves LC, et al. COVID-19 as the leading cause of hospital deaths in the Brazilian public health system in 2020. Int J Infect Dis 2021;113:162−5.ArticlePubMedPMC
- 7. Grippo F, Grande E, Maraschini A, et al. Evolution of pathology patterns in persons who died from COVID-19 in Italy: a national study based on death certificates. Front Med (Lausanne) 2021;8:645543. ArticlePubMedPMC
- 8. Lampl BM, Lang M, Jochem C, et al. COVID or not COVID: attributing and reporting cause of death in a community cohort. Public Health 2022;205:157−63.ArticlePubMedPMC
- 9. Bhaskaran K, Bacon S, Evans SJ, et al. Factors associated with deaths due to COVID-19 versus other causes: population-based cohort analysis of UK primary care data and linked national death registrations within the OpenSAFELY platform. Lancet Reg Health Eur 2021;6:100109. ArticlePubMedPMC
- 10. Jefferson T, Dietrich M, Brassey J, et al. Understanding definitions and reporting of deaths attributed to COVID-19 in the UK: evidence from FOI requests [Preprint]. Posted 2022 Apr 29. medRxiv 2022.04.28.22274344. https://doi.org/10.1101/2022.04.28.22274344.
- 11. Weinberger DM, Chen J, Cohen T, et al. Estimation of excess deaths associated with the COVID-19 pandemic in the United States, March to May 2020. JAMA Intern Med 2020;180:1336−44.ArticlePubMedPMC
- 12. Reed C, Biggerstaff M, Finelli L, et al. Novel framework for assessing epidemiologic effects of influenza epidemics and pandemics. Emerg Infect Dis 2013;19:85−91.ArticlePubMedPMC
- 13. Mizumoto K, Chowell G. Estimating risk for death from coronavirus disease, China, January-February 2020. Emerg Infect Dis 2020;26:1251−6.ArticlePubMedPMC
- 14. Munayco C, Chowell G, Tariq A, et al. Risk of death by age and gender from CoVID-19 in Peru, March-May, 2020. Aging (Albany NY) 2020;12:13869−81.ArticlePubMedPMC
- 15. Gundlapalli AV, Lavery AM, Boehmer TK, et al. Death certificate-based ICD-10 diagnosis codes for COVID-19 mortality surveillance - United States, January-December 2020. MMWR Morb Mortal Wkly Rep 2021;70:523−7.ArticlePubMedPMC
- 16. Veeranna CH, Rani S. Cause of death certification in COVID-19 deaths. Indian J Crit Care Med 2020;24:863−7.ArticlePubMedPMC
- 17. World Health Organization (WHO). International guidelines for certification and classification (coding) of COVID-19 as cause of death [Internet]. WHO; 2020 [cited 2022 Dec 2]. Available from: https://www.who.int/publications/m/item/international-guidelines-for-certification-and-classification-%28coding%29-of-covid-19-as-cause-of-death.
- 18. National Center for Health Statistics. Guidance for certifying deaths due to coronavirus disease 2019 (COVID-19): expanded in February 2023 to include guidance for certifying deaths due to post-acute sequelae of COVID-19 [Internet]. Centers for Disease Control and Prevention; 2020 [cited 2023 Mar 28]. Available from: https://dx.doi.org/10.15620/cdc:124588.
- 19. Korea Disease Control and Prevention Agency. Coronavirus disease 2019 response and management guidelines for local governments in South Korea (10-2th ed). Central Disease Control Headquarters; 2021. Korean.
- 20. Gill JR, DeJoseph ME. The importance of proper death certification during the COVID-19 pandemic. JAMA 2020;324:27−8.ArticlePubMed
- 21. Messias KL, Bispo Junior JP, Pegado MF, et al. The quality of certification of deaths due to external causes in the city of Fortaleza in the State of Ceara, Brazil. Cien Saude Colet 2016;21:1255−67.PubMed
- 22. Magno L, Rossi TA, Mendonca-Lima FW, et al. Challenges and proposals for scaling up COVID-19 testing and diagnosis in Brazil. Cien Saude Colet 2020;25:3355−64.PubMed
- 23. Patil A, Singh NP. Death certification errors in medical certificates of cause of death related to COVID-19 disease. Int J Community Med Public Health 2022;9:3746−52.ArticlePDF
- 24. Meilia PD, Manela C, Yudy , et al. Characteristics of deceased and quality of death certificates for cases subjected to Indonesia's management of the dead protocol for bodies with COVID-19. Forensic Sci Med Pathol 2022;18:45−56.ArticlePubMedPMCPDF
- 25. Alipour J, Karimi A, Miri-Aliabad G, et al. Quality of death certificates completion for COVID-19 cases in the southeast of Iran: a cross-sectional study. Health Sci Rep 2022;5:e802.ArticlePubMedPMCPDF
- 26. World Health Organization (WHO). Rolling updates on coronavirus disease (COVID-19) [Internet]. WHO; 2020 [cited 2022 Dec 1]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen.
- 27. Lew AA, Cheer JM, Haywood M, et al. Visions of travel and tourism after the global COVID-19 transformation of 2020. Tour Geogr 2020;22:455−66.Article
- 28. Ahmad FB, Anderson RN. The leading causes of death in the US for 2020. JAMA 2021;325:1829−30.ArticlePubMedPMC
- 29. Statistics Korea. Causes of death statistics in 2021 [Internet]. Statistics Korea; 2022 [cited 2022 Dec 1]. Available from: https://kostat.go.kr/board.es?mid=a10301060200&bid=218&act=view&list_no=420715. Korean.
- 30. Slater TA, Straw S, Drozd M, et al. Dying 'due to' or 'with' COVID-19: a cause of death analysis in hospitalised patients. Clin Med (Lond) 2020;20:e189−90.ArticlePubMedPMC
- 31. Palmieri L, Palmer K, Lo Noce C, et al. Differences in the clinical characteristics of COVID-19 patients who died in hospital during different phases of the pandemic: national data from Italy. Aging Clin Exp Res 2021;33:193−9.ArticlePubMedPMCPDF
- 32. Her AY, Bhak Y, Jun EJ, et al. Sex-specific difference of in-hospital mortality from COVID-19 in South Korea. PLoS One 2022;17:e0262861.ArticlePubMedPMC
- 33. Bogdanovic M, Atanasijevic T, Popovic V, et al. Proper death certification in the time of the COVID-19 pandemic: forensic perspective. J Infect Dev Ctries 2022;16:966−8.ArticlePubMedPDF
- 34. Rao C. Medical certification of cause of death for COVID-19. Bull World Health Organ 2020;98:298−298A.ArticlePubMedPMC
References
Figure & Data
References
Citations

- Figure
- Related articles
-
- Risk factors for transmission in a COVID-19 cluster infection in a high school in the Republic of Korea
- Risk factors for COVID-19 outbreaks in livestock slaughtering and processing facilities in Republic of Korea
- Effectiveness of the COVID-19 vaccine in the Honam region of the Republic of Korea
- Preparedness for the next wave of COVID-19 in the Republic of Korea


 Cite
Cite