Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Forthcoming articles > Article
-
Original Article
Factors associated with the timely diagnosis of malaria and the utilization of types of healthcare facilities: a retrospective study in the Republic of Korea -
HyunJung Kim1
 , Sangwoo Tak2
, Sangwoo Tak2 , So-dam Lee1
, So-dam Lee1 , Seongwoo Park1
, Seongwoo Park1 , Kyungwon Hwang1
, Kyungwon Hwang1
-
DOI: https://doi.org/10.24171/j.phrp.2023.0349
Published online: April 16, 2024
1Division of Control for Zoonotic and Vector Borne Disease, Bureau of Infectious Disease Policy, Korea Disease Control and Prevention Agency, Cheongju, Republic of Korea
2Division of Risk Assessment, Bureau of Public Health Emergency Preparedness, Korea Disease Control and Prevention Agency, Cheongju, Republic of Korea
- Corresponding author: Kyungwon Hwang Division of Control for Zoonotic and Vector Borne Disease, Bureau of Infectious Disease Policy, Korea Disease Control and Prevention Agency, Cheongju, 187 OsongSaengmyeong 2-ro, Osong-eup, Heungdeok-gu, Cheongju 28159, Republic of Korea E-mail: kirk99@korea.kr
© 2024 Korea Disease Control and Prevention Agency.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
- 285 Views
- 8 Download
Abstract
-
Objectives
- This study aimed to analyze trends in the timely diagnosis of malaria cases over the past 10 years in relation to the utilization of different types of healthcare facilities.
-
Methods
- The study included 3,697 confirmed and suspected cases of malaria reported between January 1, 2013, and December 31, 2022, in the national integrative disease and healthcare management system. Some cases lacking a case report or with information missing from the case report were excluded from the analysis. A generalized linear model with a Poisson distribution was constructed to estimate risk ratios and 95% confidence intervals adjusted for other variables, such as distance.
-
Results
- When cases involving diagnosis >5 days after symptom onset in confirmed patients (5DD) were examined according to the type of healthcare facility, the risk ratio of 5DD cases was found to be higher for tertiary hospitals than for public health facilities. Specifically, the risk ratio was higher when the diagnosis was established at a tertiary hospital, even after a participant had visited primary or secondary hospitals. In an analysis adjusted for the distance to each participant’s healthcare facility, the results did not differ substantially from the results of the crude analysis.
-
Conclusion
- It is imperative to improve the diagnostic capabilities of public facilities and raise awareness of malaria at primary healthcare facilities for effective prevention and control.
- Malaria is a representative mosquito-borne infectious disease, caused by protozoan parasites transmitted by female mosquitoes of the Anopheles genus [1]. The disease may be caused by any of 5 species of protozoa in the genus Plasmodium: Plasmodium vivax (PV), Plasmodium ovale (PO), Plasmodium malariae (PM), Plasmodium falciparum (PF), and Plasmodium knowlesi (PK). Among these, PF and PV pose the greatest threat to humans globally [2]. PF is mainly prevalent in Africa, while PV is commonly found in other regions [3].
- In 1979, the World Health Organization declared the Republic of Korea malaria-free [4–6]. However, cases have been reported since 1993, when a soldier experienced a confirmed infection while stationed in Paju, Gyeonggi Province, an area bordering North Korea. By 2000, the annually reported cases had reached 4,000. Due to persistent efforts to eliminate malaria, in recent years the number has fallen to 400 to 500 cases annually [7–9].
- The most common symptoms of malaria are fever, chills, and headache. For PV, which is typically found in the Republic of Korea, fever occurs in 48-hour cycles with latency periods that vary from a week to 2 years. This means that symptoms may not develop immediately after transmission via mosquito and that their onset may occur in the following year [10].
- In the Republic of Korea, malaria cases occur primarily in regions that border North Korea, such as Incheon, Gyeonggi Province, and northern Gangwon Province. Cases are reported yearly, primarily between May and October, when the vector mosquito is most active. Very few cases are reported during the winter [11–14]. Malaria incidence also differs significantly by sex. In 2022, 420 indigenous malaria cases were reported, with 359 cases (approximately 85%) occurring in men. This trend has remained relatively constant, since approximately 80% of all cases occurred in men both before the COVID-19 pandemic (in 2019) and after it had begun (in 2020). Regarding age, the largest percentage of cases occurs in individuals in their 20s, accounting for more than 30% of cases when the ages of confirmed patients have been categorized as a group aged ≤19 years followed by groups in increments of 10 years [7–9,11,14].
- Previous studies have focused primarily on identifying how the infection spreads or on developing diagnostic methods, with little emphasis on understanding how malaria patients use healthcare facilities or the symptoms they experience [4–9,15–17].
- To eliminate malaria, it is crucial to interrupt the spread of infection by promptly diagnosing suspected cases [14]. In the Republic of Korea, malaria is classified as a class 3 statutory infectious disease, and all confirmed cases must be reported [14]. Furthermore, the government is actively working towards the eradication of malaria by the year 2030 to align with the World Health Organization’s framework and objectives for malaria elimination [18].
- To achieve the goal of eradication, managing the vector through mosquito control alone is not sufficient. A strategy is needed to proactively block the transmission pathway by diagnosing suspected malaria patients early while reducing the spread of malaria [19]. Thus, the role of healthcare facilities is crucial because they are at the forefront of both diagnosis and treatment. This study aimed to analyze trends regarding the timely diagnosis of malaria cases over the past 10 years, along with factors related to the utilization of different types of healthcare facilities.
Introduction
- This cross-sectional study used diagnosis more than 5 days after symptom onset in confirmed patients (5DD) as the dependent variable. Some quantitative variables, such as age, were grouped a priori for ease of analysis and interpretation.
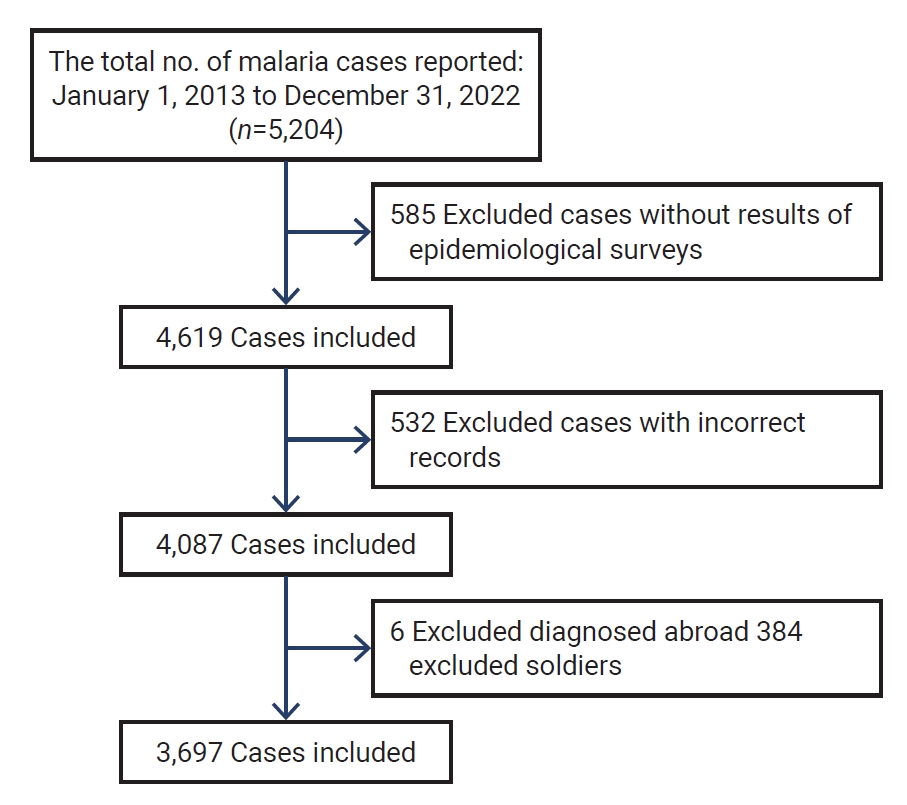
- A total of 5,204 malaria cases, reported between January 1, 2013, and December 31, 2022, were found in the national integrative disease and healthcare management system, which is a Korea Disease Control and Prevention Agency (KDCA) data platform used for reporting cases of infectious disease according to statutory regulation [20]. Among these cases, 585 of them had no case report, 532 case reports lacked some information, and 6 were diagnosed overseas; these were consequently excluded from the analysis. Additionally, 384 cases confirmed during military service were excluded because the relevant individuals were transferred to a military hospital for diagnosis and treatment, which prevented calculating the distance between their residence and healthcare facilities; addresses within military bases could not be identified. Therefore, the final total included in the study was 3,697 cases (Figure 1).
- Individuals were grouped into the following age ranges for analysis: ≤19 years, 20 to 29 years, 30 to 39 years, 40 to 49 years, 50 to 59 years, and ≥60 years.
- The KDCA manages malaria risk by designating specific areas at risk due to their high numbers of malaria cases. We defined the risk areas based on 3 years of incidence data, from 2020 to 2022. Most areas were unchanged during that period. As of 2023, the high-risk areas included northern Gyeonggi Province, northern Gangwon Province, and Incheon, comprising a total of 30 municipalities. The moderate-risk areas encompassed 18 municipalities with at least 1 case in the prior 3 years situated close to high-risk areas. Excluding the 48 areas categorized as high or moderate-risk areas, the remaining areas were classified as no-risk areas.
- In general, 5 species of malaria parasites can infect people. These parasites are PV, PF, PO, PM, and PK. The only malaria parasite indigenous to the Republic of Korea is PV. For the current study, the infectious source was categorized as PV, PF, PO, or PM by type of protozoa, or as “unknown” when the protozoa was not identified.
- Healthcare facilities were categorized as clinics, hospitals, or general hospitals according to the Medical Service Act [21]. This classification included public health facilities responsible for monitoring infectious diseases and managing patients, and capable of diagnosing malaria. General hospitals were subcategorized as general or tertiary hospitals; the latter category was divided further into “tertiary hospital first” or tertiary-first if the diagnosis was confirmed there on a patient’s first visit since symptom onset, and “tertiary hospital second” or tertiary-second if a patient was diagnosed there after visiting other clinics or hospitals since symptom onset. In accordance with the above classification, the types of healthcare facilities considered for analysis were tertiary hospital second, tertiary hospital first, general hospital, hospital, clinic, and public health facility.
- The distance variable measured the distance between each participant’s residence in their case report and the healthcare facility where malaria was diagnosed. Residential addresses were converted into latitude and longitude coordinates using Google’s geocoding service. Coordinates for healthcare facilities were determined using the nationwide directory of hospitals, clinics, and pharmacies available on the Health Insurance Review and Assessment Service website as of October 2023 [22]. After the coordinates of each confirmed patient’s residence and their healthcare facility were identified, the straight-line distance between these 2 points was calculated using QGIS (https://qgis.org/en/site/)’s distance matrix function.
- In the United States, medically vulnerable areas are determined based on physical accessibility by converting a 30-minute travel time to the primary hospital into a distance of 10 km [23]. A study utilizing the Korean medical panel confirmed that the majority of individuals had visited healthcare facilities within 5 km when measuring the distance between the residence of major disease patients and their primary healthcare facilities [24]. Consequently, this study classified the distance between a confirmed patient’s residence and the healthcare facility where they were diagnosed into <5 km, 5 to 10 km, 10 to 20 km, 20 to 30 km, and >30 km.
- Due to the non-specific nature of malaria symptoms, diagnosing patients based solely on clinical symptoms is very challenging. Clinical symptoms such as fever may manifest from 7 days to up to 2 years after initial infection by mosquito; such broad variation in latency period can delay diagnosis. Past research has confirmed that patients typically seek treatment by visiting a healthcare facility within an average of 4 days after symptom onset [25]. Consequently, as a performance indicator of the malaria eradication project, the KDCA recommends using treatment initiation within 5 days of symptom onset. Recent analysis has revealed that the time to diagnose malaria over the past 5 years averaged 4.6 days (standard deviation=13.0) [26].
- Statistical Analysis
- In this study, since 5DD was used as a dependent variable and a Poisson distribution was assumed, a generalized linear model with a Poisson distribution was constructed to estimate risk ratios and 95% confidence intervals adjusted for other variables, such as distance. All statistical analyses were performed using IBM SPSS Statistics ver. 22.0 (IBM Corp.), and a p-value of <0.05 was considered to indicate statistical significance.
- Ethics Statement
- The study protocol was approved by the Institutional Review Board (IRB) of the KDCA (no: KDCA-2023-10-08). Informed consent was waived by the IRB.
Materials and Methods
- Table 1 shows the characteristics of confirmed malaria cases that were reported from January 2013 to December 2022. Of the 3,697 total cases analyzed, 2,909 subjects (78.7%) were male and 788 subjects (21.3%) were female. Regarding age groups, the largest percentage was the group in their 20s with 1,001 subjects (27.1%), followed by those in their 40s and 50s with 703 subjects (19.0%) and 687 subjects (18.6%), respectively.
- In the classification by the species of malaria protozoa, the majority of infections (3,238 cases, 87.6%) were caused by PV of domestic origin, while the number of cases imported from overseas was 324 cases (8.8%) by PF, 18 cases (0.5%) by PO, and 10 cases (0.3%) by PM. In addition to these, 107 cases (2.9%) were of unknown type, in which the type of protozoa could not be identified since blood could not be collected.
- As for the incidence according to the malaria risk areas classified by the KDCA, 2,173 cases (58.8%) were from high-risk areas, 422 cases (12.0%) were from moderate-risk areas, and 1,082 cases (29.3%) were from no-risk areas.
- When the distance was measured from each confirmed patient’s residential address to the healthcare facility that confirmed their diagnosis, the facility was located within 5 km in 1,808 cases (48.9%), within 5 to 10 km in 723 cases (19.6%), within 10 to 20 km in 594 cases (16.1), within 20 to 30 km in 196 cases (5.3%), and 30 km away or farther in 376 cases (10.2%).
- When classified according to the type of healthcare facility where malaria was finally diagnosed, 998 cases (27.0%) were diagnosed at a tertiary hospital and 2,128 cases (57.6%) were diagnosed at a general hospital, accounting for the majority. The final diagnosis occurred at a hospital or clinic in 265 cases (7.2%) and 126 cases (3.4%), respectively, and 180 cases (4.9%) were diagnosed at public health facilities.
- From symptom onset to final diagnosis, 53.2% of the cases that occurred in men were 5DD, while 48.4% of the cases in women were 5DD. By age group, 62.8% of the cases occurring in subjects in their 20s were 5DD, while 55.1% of cases occurring in subjects aged ≤19 years were 5DD; in subjects aged ≥60 years, only 36.5% of cases were 5DD.
- By the type of protozoa, malaria caused by PV accounted for 87.6% of all cases, and 54.0% of them were 5DD. By risk area, 42.8% of the cases occurring in high-risk areas were 5DD, while 64.5% and 66.0% of the cases occurring in moderate-risk and no-risk areas were 5DD, respectively.
- As for the time to diagnosis according to distance, 53.8% of the cases diagnosed in a healthcare facility within 5 km were 5DD, whereas 51.0% of the cases diagnosed at a healthcare facility within 5 to 10 km were 5DD. The diagnosis was 5DD in 46.8%, 58.0%, and 46.9% of cases diagnosed at healthcare facilities within 10 to 20 km, within 20 to 30 km, and 30 km or farther from the participant’s residence, respectively.
- Regarding the time to diagnosis according to the type of healthcare facility, only 32.2% of cases diagnosed at public health facilities were 5DD, whereas 49.2% and 37.4% of the cases diagnosed at clinics and hospitals, respectively, were 5DD. For general hospitals, 48.8% of the cases were 5DD. When subjects were diagnosed at a tertiary hospital, a distinction was made as to whether the initial diagnosis was made at the tertiary hospital (first) or after visiting primary or secondary hospitals (second). The diagnosis was 5DD in 61.1% of tertiary-first cases and 74.5% of tertiary-second cases.
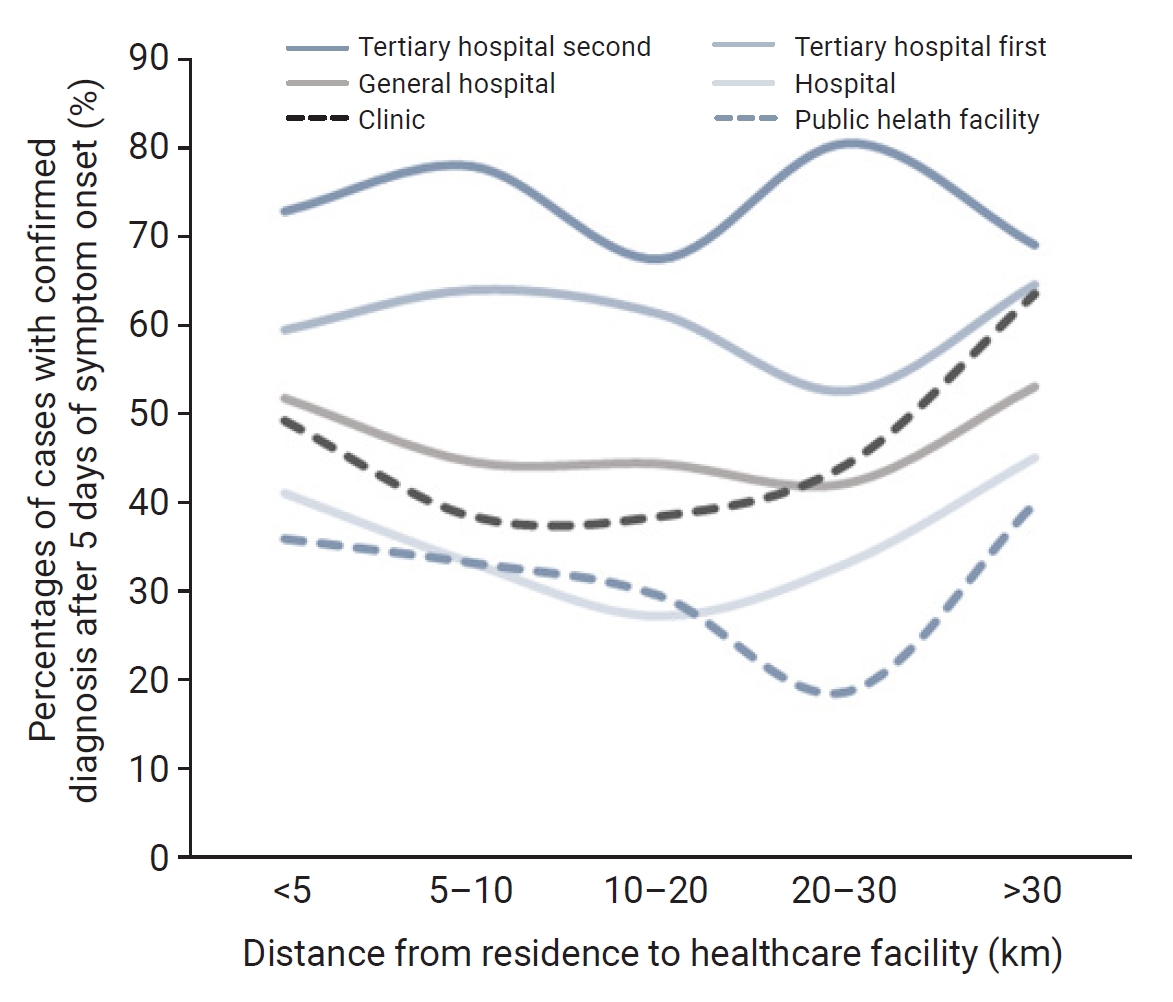
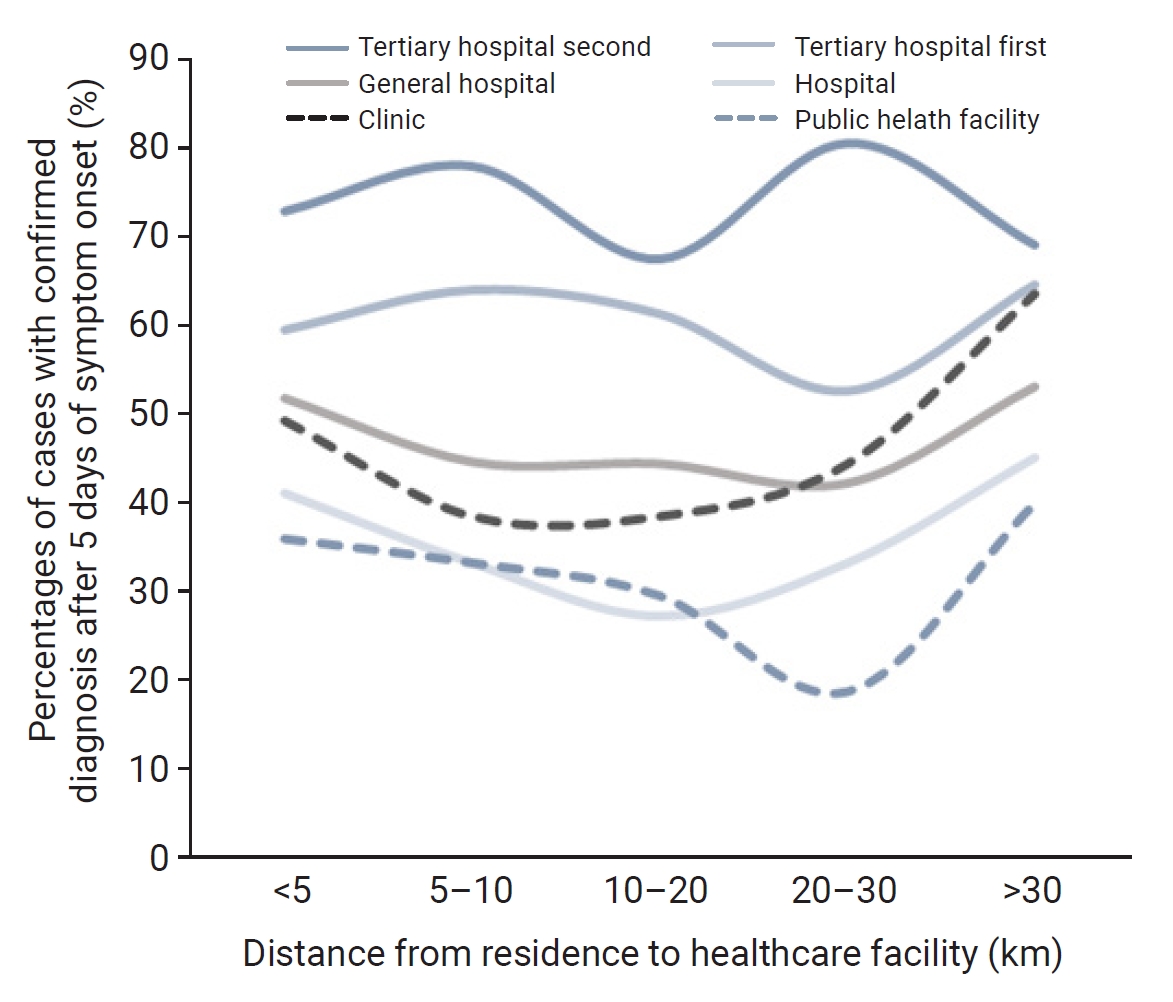
- When the trend in healthcare facilities was analyzed based on the time to diagnosis according to distance, it was confirmed that the percentage of time to diagnosis in more than 5 days was higher, based on the distance of 30 km, in cases where public health facilities, hospitals and clinics, general hospitals, or tertiary hospitals were visited first.
- Regarding the type of healthcare facility, when the diagnosis was confirmed at a public health facility, the ratio of exceeding 5 days decreased as the distance from a participant’s residence increased, then increased again once the distance reached 30 km. In contrast, when the diagnosis was confirmed tertiary-second, the ratio of cases diagnosed after 5 days increased as the distance increased up to 30 km, then decreased again once the distance reached 30 km (Figure 2).
- Table 2 shows the characteristics of confirmed malaria cases regarding time to diagnosis in more than 5 days. It was found that a diagnosis was confirmed later in men than women, but the finding was not statistically significant. Considering the group aged ≥60 years as reference, diagnoses were 1.122 times more likely to be confirmed after 5 days for those in their 20s. Though the ratio was found to be 1.127 times for those aged ≤19 years, 1.075 times for those in their 30s, 1.073 times for those in their 40s, and 1.075 times for those in their 50s, statistical significance was found only for the group in their 20s.
- When the healthcare facility was within 5 km of the participant’s residence, cases were 0.985 times less likely to be 5DD compared to when subjects lived more than 30 km away. For those living within 5 to 10 km of healthcare facilities, the ratio was 0.974 times, followed by 0.961 times for those living within 10 to 20 km, and 0.952 times for those living within 20–30 km.
- Those living in high-risk areas were 0.909 times less likely to be diagnosed after 5 days than those living in no-risk areas, whereas those living in moderate-risk areas were 1.008 times more likely to be diagnosed after 5 days.
- When the ratio of 5DD cases was examined according to the type of healthcare facility, with public health facilities considered as reference, it was found that the ratio of cases diagnosed after 5 days increased in the order of hospital, general hospital, clinic, and tertiary hospital. Specifically, it was confirmed that the ratio was higher when the diagnosis was made at a tertiary hospital, even after the participant had visited a primary or secondary hospital, although the results of analysis adjusted by the distance to healthcare facilities did not differ greatly from the results of the crude analysis (Table 2).
Results
- This study analyzed the utilization of healthcare facilities among malaria patients in the Republic of Korea and examined the impact of the distance between their residences and healthcare facilities, as well as the types of facilities they visited, to understand how to prevent the further spread of malaria infection and improve the time to diagnosis and treatment.
- Whereas previous studies on malaria cases focused mainly on the distribution of cases, the influence of vector mosquitoes, and methods for timely diagnosis, the current study emphasized patients’ utilization of healthcare facilities and the time elapsed from symptom onset to diagnosis.
- The characteristics of malaria cases confirmed in this study were similar to those from earlier studies [9,13]. Indigenous malaria cases, whose vector is PV, occur at a relatively high rate in men in their 20s serving at military bases in the northern part of Gyeonggi Province, near the border with North Korea [4,7,8,13,19,27,28]. Even after excluding the occurrences in military personnel, which is the major characteristic of indigenous cases, the largest percentage of cases (78.7%) by age group and sex occurred in men in their 20s, and the high-risk area bordering North Korea had the largest percentage of occurrences (58.8%) by region. In terms of the utilization of healthcare facilities, 48.9% of all confirmed cases reported as malaria were diagnosed at a healthcare facility within 5 km of the participant’s residence, while 57.6% of the cases were diagnosed at general hospitals, 27% of which were tertiary hospitals. Those who had visited public health facilities accounted for 4.9%, similar to the 3.4% of subjects who had visited clinics.
- It is challenging to diagnose malaria based merely on symptoms at primary healthcare facilities, such as hospitals and clinics, because the clinical symptoms of malaria are non-specific and may easily be mistaken for another disease. In addition, because the national incidence rate in the Republic of Korea is very low, less than 1 case per 100,000 residents, malaria is often diagnosed at general or tertiary hospitals instead of hospitals or clinics.
- As a result, patients suspected of having malaria have the shortest time to diagnosis when diagnosed at public health facilities; the time to diagnosis increases for tertiary hospitals. Since malaria is under regulatory supervision in the Republic of Korea and physicians working at public health facilities are required to receive regular training, the physicians at such facilities tend to be more aware of malaria than physicians elsewhere.
- In laboratories, malaria is diagnosed using different techniques: conventional microscopic diagnosis from staining thin and thick peripheral blood smears, molecular diagnostic methods such as polymerase chain reaction, and antigen-based rapid diagnostic tests. However, laboratory methods have some disadvantages for prompt diagnosis. Microscopic diagnosis requires trained healthcare workers with considerable expertise, and molecular diagnostic methods are time-consuming [29–32].
- Several previous studies have proposed malaria antigen and antibody tests on febrile patients as a strategy for prompt diagnosis [32–34]. The cost of diagnostic tests for malaria has been included in the medical benefits coverage at primary healthcare facilities in the Republic of Korea. However, as mentioned above, it is not easy to make a differential diagnosis of malaria patients at a primary healthcare facility, and keeping antigen and antibody test kit supplies in stock can be difficult for clinics and hospitals due to the small number of cases.
- This study has limitations in that it only reflected information identified in the case reports, and it analyzed the straight-line distance, not the travel distance, between residences and healthcare facilities. However, factors associated with accessibility related to the utilization of healthcare services, such as availability, mutual acceptability, ability to pay, and convenience, seem to have minimal influence on how long malaria diagnosis may take [35]. Malaria diagnosis is covered by health insurance in the Republic of Korea and is available at low cost through public health facilities, such as the Public Health and Environment Research Institute. Therefore, the impact of these related factors is also expected to be minimal.
- In addition, the current study did not investigate whether the subjects visited multiple healthcare facilities before receiving a diagnosis, since the available case reports did not include their medical history. Further studies should identify the impact of misclassified facility visit data on the relationship between a delay in diagnosis and the potential spread of community infection.
- In addition, although military personnel account for a high proportion of indigenous malaria cases, they were excluded from this study since their exact location of residence could not be identified for security reasons. Considering that the military has its own healthcare system, further research is necessary for analyzing the factors related to timely diagnosis among military personnel.
- According to the findings of this study, it is crucial to identify malaria patients promptly by improving the diagnostic capabilities for malaria at public health facilities. However, patients rarely visit public health facilities when experiencing symptoms like fever or chills, and these facilities are less accessible physically than hospitals and clinics.
- Therefore, it becomes imperative for primary and secondary hospitals, including clinics, to adopt the malaria diagnostic methods conducted at public health facilities as well as to support patients who present with fever symptoms, thus ensuring timely diagnosis of malaria. A policy advocating for simplified malaria tests at clinics and hospitals should be established, particularly for patients who experience fever between May and October, when the prevalence of malaria is high. Additionally, it is crucial for public health facilities to test potentially exposed individuals, such as the family members and colleagues of confirmed patients.
Discussion
- In conclusion, this study has shown that the highest proportion of malaria diagnoses within 5 days occurred at public health facilities, while tertiary hospitals exhibited the longest time to diagnosis. While it may be expected for tertiary hospitals to have a longer time to diagnosis due to the need for referral from primary or secondary hospitals, the analysis indicated that the ratio of cases diagnosed after 5 days of symptom onset increased for tertiary hospitals, even for tertiary-first cases. In other words, when compared to public health facilities, hospitals, general hospitals, clinics, and tertiary hospitals showed an increasing order in the ratio of cases diagnosed after 5 days. This pattern persisted even when considering the distance between residence and healthcare facilities in the model.
- Given that malaria, an infectious disease caused by a vector mosquito, requires blocking the cycle of infection by preventing the spread of infection via the human host as well as managing vector transmission, the timely diagnosis of confirmed cases becomes crucial. It is imperative to enhance the diagnostic capabilities of public health facilities and raise awareness about malaria at primary healthcare facilities for effective prevention and control.
Conclusion
- • To prevent the spread of malaria, the chain of infection can be broken by early detection and initiation treatment of patients. This study aims to analyze the trend of malaria diagnosis.
- • When the ratio of cases of diagnosis after 5 days of symptom onset were examined according to the type of healthcare facility, it was found that the risk ratio of diagnosis after 5 days of symptom onset cases increased from public health facilities to tertiary hospitals.
- • It is imperative to enhance the diagnostic capabilities of public facilities and raise awareness about malaria at primary healthcare facilities for effective prevention and control.
HIGHLIGHTS
-
Ethics Approval
This study was approved by the Institutional Review Board of KDCA (no: KDCA-2023-10-08). The Board waived the requirement for informed consent.
-
Conflicts of Interest
The authors have no conflicts of interest to declare.
-
Funding
None.
-
Availability of Data
The datasets are not publicly available. If you have any questions regarding this study, contact the corresponding author (kirk99@korea.kr).
-
Authors’ Contributions
Conceptualization: HK, ST; Data curation: HK; Formal analysis: HK, ST; Investigation: SL, JL; Methodology: ST, HK; Resources: HK, SL, SP; Software: HK; Supervision: ST, KH; Writing–original draft: HK, ST; Writing–review & editing: all authors. All authors read and approved the final manuscript.
Article information
|
Crude RR |
Adjusted RR |
|||
|---|---|---|---|---|
| Exp(B) | 95% CI | Exp(B) | 95% CI | |
| (intercept) | 1.397* | 1.166–1.674 | 1.368* | 1.152–1.625 |
| Sex | ||||
| Male | 1.000 | 0.936–1.068 | 0.999 | 0.936–1.067 |
| Female | Ref. | Ref. | ||
| Age (y) | ||||
| ≤19 | 1.127 | 0.988–1.286 | 1.126 | 0.988–1.285 |
| 20‒29 | 1.122* | 1.022–1.232 | 1.122* | 1.022–1.232 |
| 30‒39 | 1.075 | 0.972–1.189 | 1.075 | 0.972–1.190 |
| 40‒49 | 1.073 | 0.974–1.182 | 1.072 | 0.973–1.181 |
| 50‒59 | 1.075 | 0.976–1.185 | 1.075 | 0.975–1.184 |
| ≥60 | Ref. | Ref. | ||
| Distance from residence to facility (km) | ||||
| <5 | 0.985 | 0.901–1.078 | NA | |
| 5‒10 | 0.974 | 0.880–1.077 | ||
| 10‒20 | 0.961 | 0.865–1.069 | ||
| 20‒30 | 0.952 | 0.826–1.096 | ||
| >30 | Ref. | |||
| KDCA risk area | ||||
| High risk | 0.909* | 0.851–0.972 | 0.907* | 0.849–0.969 |
| Moderate risk | 1.008 | 0.923–1.100 | 1.006 | 0.922–1.098 |
| No risk | Ref. | Ref. | ||
| Healthcare facility type | ||||
| Tertiary hospital second | 1.202* | 1.034–1.398 | 1.207* | 1.038–1.403 |
| Tertiary hospital first | 1.105 | 0.950–1.286 | 1.111 | 0.955–1.292 |
| General hospital | 1.072 | 0.938–1.226 | 1.077 | 0.942–1.231 |
| Hospital | 1.013 | 0.859–1.193 | 1.018 | 0.864–1.199 |
| Clinic | 1.081 | 0.891–1.311 | 1.089 | 0.899–1.320 |
| Public health facility | Ref. | Ref. | ||
- 1. Goher N, Khaliq FH, Yousaf MW. Prescribing trend of treating malaria patients by public and private healthcare facilities in Lahore. Bull Pharm Med Res 2022;1:22−30.Article
- 2. Hossain MS, Commons RJ, Douglas NM, et al. The risk of Plasmodium vivax parasitaemia after P. falciparum malaria: an individual patient data meta-analysis from the WorldWide Antimalarial Resistance Network. PLoS Med 2020;17:e1003393.PubMedPMC
- 3. World Health Organization (WHO). World malaria report 2022 [Internet]. WHO; 2022 [cited 2023 Dec 25]. Available from: https://www.who.int/teams/global-malaria-programme/reports/world-malaria-report-2022.
- 4. Chai JY. History and current status of malaria in Korea. Infect Chemother 2020;52:441−52.ArticlePubMedPMCPDF
- 5. Ree HI. Unstable vivax malaria in Korea. Korean J Parasitol 2000;38:119−38.ArticlePubMedPMC
- 6. Yeo I. A history of malaria in modern Korea 1876-1945. Uisahak 2011;20:53−82.PubMed
- 7. Kan H, Kwon J, Park S, et al. Characteristics of reported malaria cases, 2020. Public Health Wkly Rep 2021;14:1023−35. Korean.
- 8. Kho WG. Reemergence of malaria in Korea. J Korean Med Assoc 2007;50:959−66.Article
- 9. Kim H, Lee S, Shin NR, et al. Status of malaria and diagnosis rate in the Republic of Korea, 2018-2022. Public Health Wkly Rep 2023;16:852−66. Korean.
- 10. World Health Organization (WHO). Malaria symptoms [Internet]. WHO. 2023;[cited 2023 Oct 26]. Available from: https://www.who.int/health-topics/malaria#tab=tab_2.
- 11. Korea Disease Control and prevention Agency (KDCA). 2023 Guidelines for Malaria management 2023. KDCA; 2023 [cited 2023 Dec 25]. Available from: https://www.kdca.go.kr/filepath/boardSyview.es?bid=0019&list_no=721868&seq=1. Korean.
- 12. Yeom JS. Diagnosis and treatment of vivax malaria. Korean J Med 2009;77:52−4.
- 13. Park JW, Hong JY, Yeom JS, et al. Evaluation of the current status of malaria elimination project in the Republic of Korea and suggestion for improvement of its efficacy. Infect Chemother 2009;41:42−53.Article
- 14. Korea Disease Control and prevention Agency (KDCA). Infectious disease homepage [Internet]. KDCA; 2023 [cited 2023 Oct 20]. Available from: https://npt.kdca.go.kr/pot/is/summary.do. Korean.
- 15. Shin DH, Seo M, Hong JH, et al. Paleopathological considerations on malaria infection in Korea before the 20th century. Biomed Res Int 2018;2018:8516785. ArticlePubMedPMCPDF
- 16. Khan MI, Qureshi H, Bae SJ, et al. Malaria prevalence in Pakistan: a systematic review and meta-analysis (2006-2021). Heliyon 2023;9:e15373.ArticlePubMedPMC
- 17. Sadoine ML, Smargiassi A, Ridde V, et al. The associations between malaria, interventions, and the environment: a systematic review and meta-analysis. Malar J 2018;17:73. ArticlePubMedPMCPDF
- 18. World Health Organization (WHO). Countries and territories certified malaria-free by WHO [Internet]. WHO; 2023 [cited 2023 Oct 26]. Available from: https://www.who.int/teams/global-malaria-programme/elimination/countries-and-territories-certified-malaria-free-by-who.
- 19. Landier J, Parker DM, Thu AM, et al. The role of early detection and treatment in malaria elimination. Malar J 2016;15:363. ArticlePubMedPMCPDF
- 20. Korea Disease Control and prevention Agency (KDCA). The disease health integrated management system [Internet]. KDCA; 2023 [cited 2023 Apr 1]. Available from: https://dportal.kdca.go.kr/pot/is/summary.do. Korean.
- 21. Korean Law Information Center. Medical service Act, Act No.19818 (May 1, 2024) [Internet]. Korean Law information Center; 2023 [cites 2023 Dec 25]. Available from: https://www.law.go.kr/LSW/eng/engLsSc.do?menuld=2§ion=lawNm&query=medical+law&x=0&y=0#liBgcolor15. Korean.
- 22. Health Insurance Review & Assessment Service (HIRA). Status of hospitals, clinics and pharmacies nationwide [Internet]. HIRA; 2023 [cited 2023 Sep 1]. Available from: https://opendata.hira.or.kr/op/opc/selectOpenData.do?sno=11925&publDataTpCd=&searchCnd=ttl&searchWrd=%EC%A0%84%EA%B5%AD&pageIndex=1. Korean.
- 23. Cromley EK, McLafferty SL. GIS and public health. 2nd ed. Guilford Press; 2012.
- 24. Shin HS, Lee SH. Factors affecting spatial distance to outpatient health services. Health Policy Manag 2011;21:23−43. Korean.Article
- 25. Chai IH, Lim GI, Yoon SN, et al. Occurrence of tertian malaria in a male patient who has never been abroad. Korean J Parasitol 1994;32:195−200.ArticlePubMed
- 26. Kim S, Kim Y. Analysis of spatial pattern changes and its human and environmental factors of the malaria risks in Korea. J Korean Cartogr Assoc 2017;17:71−85. Korean.Article
- 27. Kim T, Shin Y, Lee J, et al. Calculation of regional circuity factors using road network distance in South Korea. J Korea Plan Assoc 2013;48:319−29.
- 28. Kim YS, Lee DH, Chae HS, et al. Changing disease trends in the northern Gyeonggi-do province of South Korea from 2002 to 2013: a big data study using national health information database cohort. Osong Public Health Res Perspect 2018;9:248−54.ArticlePubMedPMCPDF
- 29. Hawkes M, Kain KC. Advances in malaria diagnosis. Expert Rev Anti Infect Ther 2007;5:485−95.ArticlePubMed
- 30. Zimmerman PA, Howes RE. Malaria diagnosis for malaria elimination. Curr Opin Infect Dis 2015;28:446−54.ArticlePubMed
- 31. Tangpukdee N, Duangdee C, Wilairatana P, et al. Malaria diagnosis: a brief review. Korean J Parasitol 2009;47:93−102.ArticlePubMedPMC
- 32. Baird KJ, Maguire JD, Price RN. Diagnosis and treatment of Plasmodium vivax malaria. Adv Parasitol 2012;80:203−70.ArticlePubMed
- 33. Park TS, Kim JH, Kang CI, et al. Diagnostic usefulness of SD malaria antigen and antibody kits for differential diagnosis of vivax malaria in patients with fever of unknown origin. Korean J Lab Med 2006;26:241−5.ArticlePubMed
- 34. Kang YH, Lim HS, Lee HM, et al. Evaluation of usefulness of the panel test composed of malaria non-specific tests as a surrogate marker. Korean J Lab Med 2008;28:332−8.ArticlePubMed
- 35. Penchansky R, Thomas JW. The concept of access: definition and relationship to consumer satisfaction. Med Care 1981;19:127−40.PubMed
References
Figure & Data
References
Citations



 Cite
Cite