Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 11(1); 2020 > Article
-
Original Article
Early Epidemiological and Clinical Characteristics of 28 Cases of Coronavirus Disease in South Korea -
Osong Public Health and Research Perspectives 2020;11(1):8-14.
DOI: https://doi.org/10.24171/j.phrp.2020.11.1.03
Published online: February 28, 2020
Korea Centers for Disease Control and Prevention, Cheongju, Korea
- *Corresponding author: COVID-19 National Emergency Response Center, Epidemiology and Case Management Team, Korea Centers for Disease Control and Prevention, Cheongju, Korea, E-mail: jeongek@korea.kr
- COVID-19 National Emergency Response Center, Epidemiology and Case Management Team. 2020.2.14. Center for Disease Prevention, KCDC Insik Kong, Youngjoon Park, Yeonhee Woo, Joosun Lee, Jeongok Cha, Junkil Choi, Youngman Kim, Jieun Kim, Shinyoung Park, Minwoo Yum, Taeyoung Kim, Joongho Jo. Center for Infectious Disease Control, KCDC Miyoung Kim, Donghan Lee, Jonghee Kim, Sookkyung Park, Hyunjung Bahk, Jeonghee Yu, Jeongran Kwon, Heesook Kim, Nari Shin, Sanghyuk Lee, Hyekyung In, Jangeun Jung, Seunghee Cho, Byounghak Jeon, Dongwook Kim. Center for Public Health Emergency Preparedness and Response, KCDC Gwack Jin, Seongsun Kim, Sungnam Kim, Youngki Kim, Eunyoung Kim, Byran Inho Kim, Heejung Kim, Hyeyoung Lee, Yeowon Jin, Jeonghyun Kim, Hwami Kim, Boyeong Ryu, Seunghwan Shin, Eensuk Shin, Jin Lee, Sangeun Lee, Yoonsuk Jang, Eunkyung Choi, Junghee Hyun, Daehyeon Ko, Garam Seo, Seunghwi Kwon, Eunmi Park, Seungwoo Choi. Center for Laboratory Control of Infectious Diseases, KCDC Seondo Hwang, Sangeun Lee, Byunghak Kang, Jaesun Park, Deogyong Lee, Sukyoung Jo, Siwon Choi. Center for Genome Science, KCDC Junghyun Lee, Sanghyun Cho, Jaekyung Park. Center for Organ Transplant Management, KCDC Junnyun Kim. National Center for Medical Information and Knowledge, KCDC Eungyu Lee, Jungsook Kim. Bureau of Planning & Coordination, KCDC Sunmi Kim. Bureau of Health Policy, Ministry of Health and Welfare, MOHW Unna Kim.
• Received: February 16, 2020 • Revised: February 20, 2020 • Accepted: February 21, 2020
Copyright ©2020, Korea Centers for Disease Control and Prevention
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Abstract
-
Objectives
- The first confirmed case of coronavirus disease 2019 (COVID-19) in South Korea was reported in January 2020, with 28 confirmed cases reported as of February 14th, 2020. The epidemiological and clinical characteristics of all 28 cases were analyzed in response to this disease.
-
Methods
- The epidemiological characteristics and early clinical features of the 28 patients from Korea with confirmed COVID-19 were analyzed using COVID-19 reporting and surveillance data and the epidemiological investigation reports prepared by the rapid response team.
-
Results
- There were 16 patients that entered Korea from foreign countries: Wuhan, China (11 patients), Zhuhai, China, (1 patient), Singapore (2 patients), Japan (1 patient), and Thailand (1 patient). The early symptoms were fever, sore throat, cough or sputum production, chills, and muscle ache. Three patients were asymptomatic, however, 18 developed pneumonia. Of the 28 cases, 16 were index cases imported from abroad, with 10 cases of secondary infection originating in Korea, and the route of transmission still under investigation for 2 patients. The 10 patients with secondary infection were infected from contact with family members or acquaintances of primary patients, and the suspected sites of transmission were mostly at home.
-
Conclusion
- COVID-19 in Korea was spread by 16 infected individuals traveling from other countries, leading to second-generation cases. The initial symptoms were mostly minor, but the disease was infectious at this stage, resulting from close contact, particularly at home. Establishing an early detection strategy for COVID-19 is crucial for managing the transmission of the disease.
- Twenty-seven patients in Wuhan City, Hubei Province of China were reported to have pneumonia of an unknown cause on December 31st, 2019 and were subsequently reported to have a novel coronavirus infection caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). After the announcement of 41 confirmed coronavirus disease 2019 (COVID-19) cases in Wuhan City, China on January 11th, infected patients were identified in Thailand on January 13th and in Japan on January 16th. More cases were confirmed in some areas of China outside Wuhan, including Beijing and Shenzhen City, Guangdong Province on January 20th, and the number of confirmed cases has continued to rise. Moreover, there have been reports of secondary transmission from China and countries including Singapore, Japan, Thailand, Malaysia, and Vietnam into Korea [1].
- In Korea, 28 confirmed cases of COVID-19 had been reported as of February 14th, since the first case was confirmed on January 20th, 2020. Of these, 16 were cases imported into the country (57.1%) and 10 were believed to be secondary cases of infections originating in Korea; in the other 2 cases, the route of transmission remained undetermined.
- The initial symptoms of COVID-19 are known to be respiratory symptoms such as coughing, in association with fevers, but the disease epidemiology remains largely unknown. To treat new infections and prevent further transmission, it is necessary to analyze and share epidemiological data on the cases reported to date [2].
Introduction
- This is a case series of the 28 patients with confirmed COVID-19 in Korea as of February 14th, 2020. To obtain demographic, epidemiological, and early clinical information, COVID-19 reporting and surveillance data from Korea Centers for Disease Control and Prevention (KCDC), and the 28 case reports of the epidemiological investigation conducted by KCDC rapid response team was utilized.
- Patient age was provided on the date of diagnosis, and key indicators such as estimated duration of exposure, date of onset of symptoms, and route of transmission were identified by an epidemiological investigator who participated in the field investigation and the epidemiological investigation team at KCDC headquarters. The incubation period was estimated based on the estimated exposure date and the date of symptom onset. However, it must be noted that the data presented in this study may change depending on the results of further epidemiological investigation.
Materials and Methods
- 1. Response to COVID-19 in Korea
- On December 31st, 2019, in Wuhan City, Hubei Province of China, 27 individuals developed pneumonia and all individuals had visited the seafood market in the area. The local centers for disease control and prevention, upon concluding that the novel infection had originated from overseas, established a “countermeasures taskforce against pneumonia of unknown cause” and set the crisis level to Blue. Accordingly, the situation overseas was constantly monitored, and surveillance in China was initiated, and responses initiated to suspected cases of infection. For suspected cases, a basic epidemiological assessment was conducted at the local health center and at the discretion of the central investigator, the patient was either admitted to a state-designated, negative-pressure isolation ward for further testing, or control measures of self-isolation and active surveillance were undertaken [3].
- On January 20th, the first case of infection from abroad was confirmed in Korea. Subsequently, the crisis level was scaled up from Blue to Yellow, and KCDC headquarters for the COVID-19 rapid response team was established. On January 27th, the crisis level was scaled up from Yellow to Orange, and the Ministry of Health and Welfare Central Accident Management Headquarters for the COVID-19 was established. Currently, all ministries of the government are cooperating in response to this novel emerging infectious disease.
- In particular, to block the transmission of infection among patients under quarantine, Wuhan City was designated as an endemic center for infection on January 8th. Based on the health questionnaire filled out by travelers from Wuhan at the point of entry, people with body temperature higher than 37.5°C or respiratory symptoms including coughing were classified as symptomatic and isolated for testing. On January 23rd, Wuhan airport, which has an average of 300 travelers per day, was shut down by the Chinese government, and travel restrictions were implemented later in Hubei Province, including Wuhan City.
- However, between January 20th and January 28th, 4 patients who presented with symptoms outside of the Hubei province who had visited Wuhan, tested positive for SARS-CoV-2, and the number of cases outside Wuhan continued to increase. On January 28th, other areas in China where the infection was reported, were also quarantined. On February 4th, a special quarantine procedure was implemented on flights from China. The procedure not only involved the assessment of symptoms upon arrival, but also included the identification of individuals confirmed to have COVID-19 and those who had been in close contact with these infected individuals.
- As of February 14th, a total of 7,242 patients were suspected of having COVID-19 and had been tested. Of those, 28 were confirmed to have COVID-19 of which 7 were discharged and 21 were treated.
- 2. Epidemiological characteristics
- Of the 28 patients with COVID-19, 15 were men (53.6%) and 13 were women (46.1%), with a mean age of 42.6 years (range: 20–73 years). Regarding age groups, 8 patients were in their 50’s (28.6%), 6 patients each were in their 20’s, 30’s, and 40’s (21.4%), and 1 patient each was in their 60’s and 70’s (3.6%). Of the 28 patients, 22 were Korean and 6 were Chinese, of whom 2 were visitors.
- Of the 16 index cases imported from abroad (57.1%), 6 contributed to the occurrence of secondary infections in 10 patients in Korea. Of those with secondary infection, 7 were first-generation patients (25.0%) and 3 were second-generation patients (10.7%). In the remaining 2 patients (7.2%), the route of transmission remains under investigation.
- The initial symptoms were fever or feeling hot (9 patients, 32.1%), sore throat (9 patients, 32.1%), cough or sputum production (5 patients, 17.9%), chills (5 patients, 17.9%), and muscle ache (4 patients, 14.3%). However, 3 patients were asymptomatic. In 18 patients, pneumonia was confirmed using imaging once hospitalized (64.3%). As of February 14th, 7 out of 28 patients had been discharged, and the average length of hospital stay was 12.7 days (range: 8–19 days).
- One patient had visited a marketplace in China, while 2 had visited a medical facility in Wuhan City. Of the 28 patients, 10 (35.7%) had at least 1 underlying disease including hypertension, diabetes, asthma, chronic rhinitis, dyslipidemia, and hypothyroidism, and 1 patient had undergone surgery for lung cancer (Table 1).
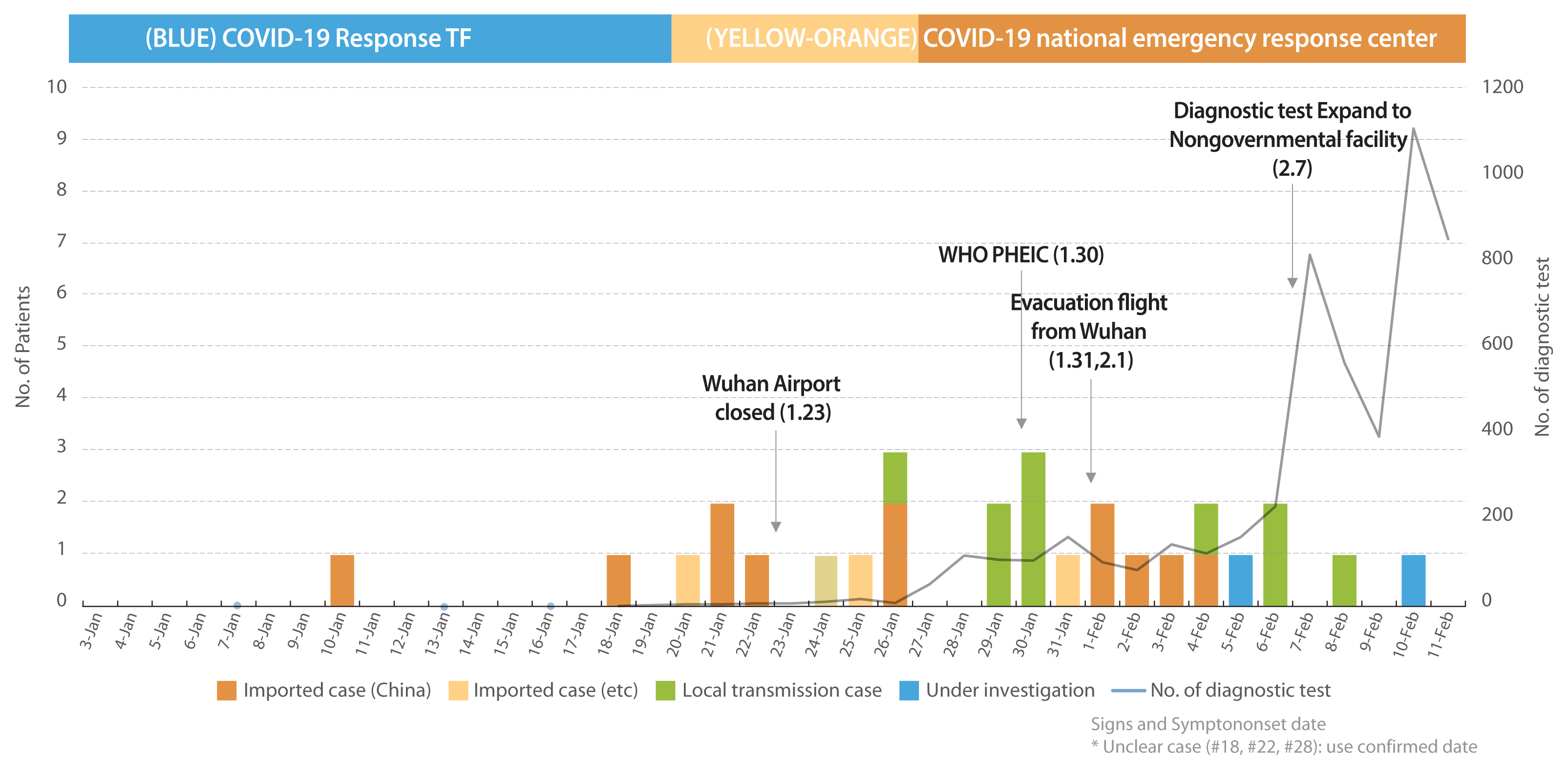
- “Test count” refers to the number of cases that were reported to KCDC by local health centers and were then tested. Prior to February 7th, tests were conducted by KCDC and the Research Institute of Public Health and Environment in the corresponding cities/provinces, the number of reports and test counts matched. After February 7th, additional tests were conducted for each individual suspected of having COVID-19 increasing the number of reports, aside from those initially conducted by the local health center.
- The earliest date of symptom onset among the 25 patients with a clear date of onset, was January 10th (for 3 patients, the date of onset was unclear). Since then, the number of confirmed index cases imported from abroad continued to increase, and symptoms were first confirmed in patients with secondary infection on January 26th. The incubation period was estimated to be 4.1 days based on the date of symptom onset and first exposure (among 9 patients, excluding 1 patient with an unclear date of onset) shown in Figure 1 and Table 2.
- In the 16 index cases imported from abroad, the suspected sites where the infection was first contracted were Wuhan, China (11 cases, 68.3%), Singapore (2 cases, 12.5%), Zhuhai, China (1 case, 6.3%), Thailand (1 case, 6.3%), and Japan (1 case, 6.3%). The 10 patients with secondary infection for which the routes of transmission were known were either family members (7 cases, 70.0%) including relatives (2 cases), or acquaintances (3 cases, 30%) of the primary patients. The suspected sites of transmission were the home (7 cases, 70.0%), a restaurant (1 case, 10.0%), a church (1 case, 10.0%), and other locations (1 case, 10.0%).
- With regard to the distribution of the 24 cases by region, excluding the 2 Wuhan residents and 2 patients who were evacuated via a charter flight, high incidence rates were reported in Gyeonggi-do (11 patients, 39.3%) and Seoul (9 patients, 32.1%), followed by Gwangju (2 patients, 7.1%), and Jeollabuk-do and Jeollanam-do (1 patient each, 3.6%) shown in Table 2.
- 3. Confirming the route of transmission
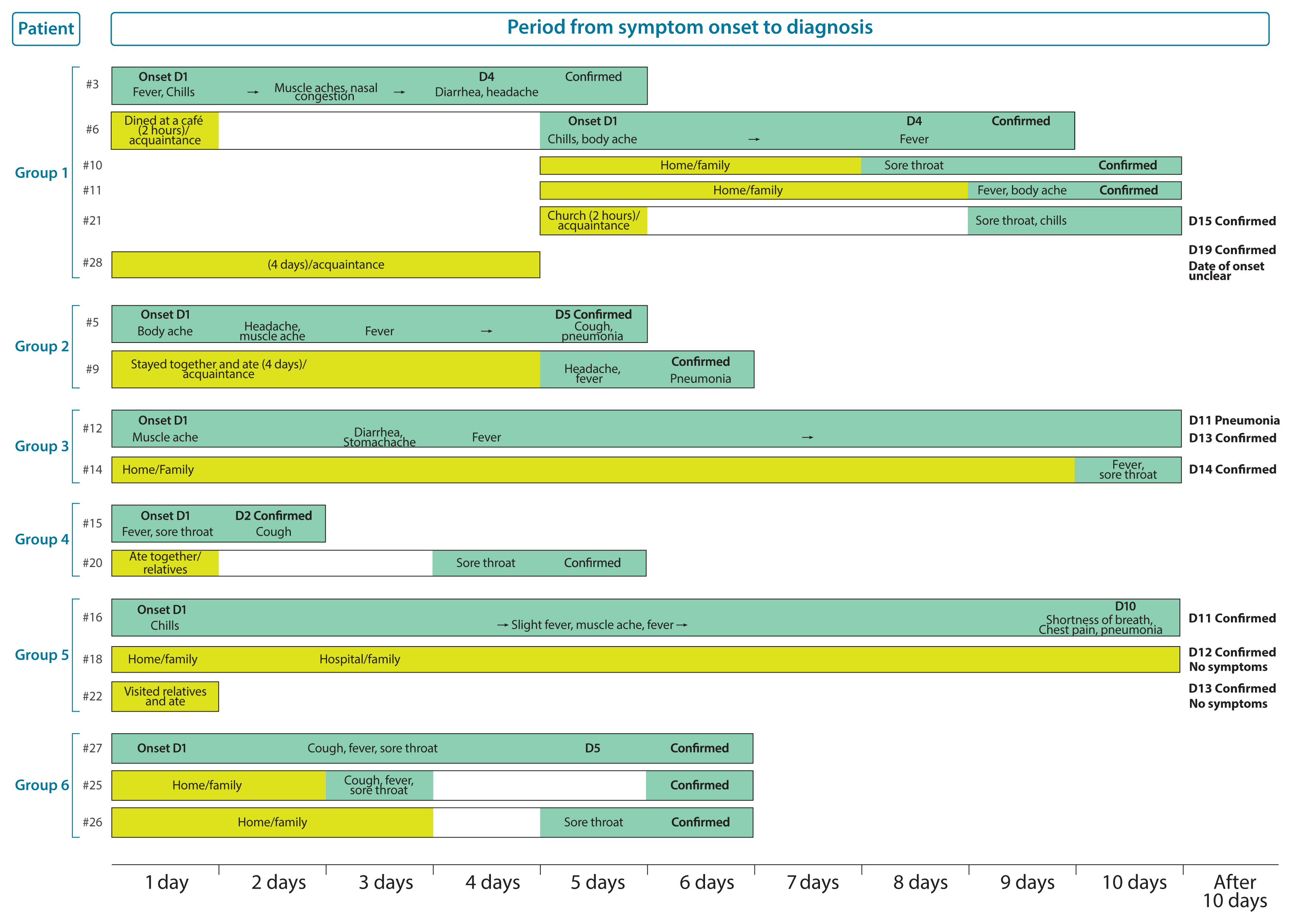
- Regarding the course of disease development in the 28 patients with confirmed COVID-19 as of February 14th, 6 patients developed secondary infection, which they contracted from previously infected individuals, with each group including 2–6 patients (Figure 2).
- The first group included the following index patients: Patient #3 was a 54-year-old man who was asymptomatic upon arrival in Korea on January 20th, but had developed a fever, chills, muscle ache, and nasal congestion by 13:00 on January 22nd. Patient #28, who was on the same flight bound from Wuhan to Korea as Patient #3, tested positive on February 10th during self-quarantine. The route of transmission is still under investigation. In addition, since Patient #28 underwent surgery following entry into the country, and was treated with antibiotics and analgesics, the exact date of onset of symptoms could not be calculated. Patient #6, an acquaintance of Patient #3, dined at a restaurant with Patient #3 on the evening of January 22nd for an hour and a half, developed symptoms including the chills on January 26th, and tested positive for COVID-19 on January 30th. Patients #10 and #11, the wife and son of Patient #6 who lived and dined at the restaurant with him, developed symptoms on January 29th and 30th, respectively, and tested positive for COVID-19. Patient #21, an acquaintance of Patient #6 who attended on January 26th, developed symptoms on January 30th and subsequently tested positive for COVID-19.
- The index case imported from abroad in the second group involved Patient #5, a 32-year-old man from Wuhan who visited Korea on January 24th and started to develop aches similar to that observed in the common cold on January 26th. Patient #9, who developed a secondary infection, was an acquaintance of Patient #5 who stayed and dined at the same place as Patient #9 until January 29th. Patient #9 developed a headache on January 30th, was managed as a contact case, and tested positive on January 31st.
- The third index case imported from abroad involved Patient #12, a 48-year-old man with a history of contact for business reasons, with a Japanese patient who had tested positive for COVID-19 in Japan. This was the first case imported from a country outside China. Following entry to Korea on January 19th, the patient started experiencing muscle aches on January 20th. However, COVID-19 was not suspected because he arrived in Korea from Japan, and thus reporting/testing was delayed. Patient #14 was his wife who stayed with him for more than 10 days before COVID-19 was confirmed. She developed symptoms on January 29th and subsequently tested positive.
- The fourth index case involved Patient #15, a 43-year-old man who was being monitored after having close contact with Patient #4 on the plane. He developed a fever and a sore throat on February 1st and subsequently tested positive. Patient #20, a relative living in the same building but on a different floor, experienced a sore throat on February 4th and subsequently tested positive. It is likely that he was infected whilst eating with Patient #15.
- The index case imported from abroad in the fifth group involved Patient #16, a 42-year-old woman who developed chills on January 25th after visiting Thailand and tested positive on February 4th. Since Patient #16 developed symptoms after visiting Bangkok and Pattaya, Thailand, between January 15th and January 19th, it is probable that she was either infected at a tourist destination in Thailand or Bangkok airport. The daughter of Patient #16 tested positive on February 5th and was designated as Patient #18. Among the other family members who dined with Patient #18 at her mother’s house on January 25th, the older brother (Patient #22) tested positive for COVID-19 on February 5th. Patients #18 and #22 were initially asymptomatic. Hence, the date of symptom onset could not be estimated. Moreover, Patient #18 had an overlapping history of visiting Thailand and a hospital visit with Patient #16 in Korea thus, the route of transmission was unclear and remained under investigation.
- The sixth transmission case originating in Korea involved Patient #25, a 73-year-old woman who tested positive at a screening clinic. Later, her son (Patient #26) and daughter-in-law (Patient #27) tested positive during the process of epidemiological investigation. After patients #26 and #27 entered Korea on January 31st from Zhuhai, Guangdong Province of China, via Macau, the 3 patients remained in the same place of residence in Korea. Considering that Patient #27 developed symptoms on February 4th, earlier than Patients #25 and #26, and Patient #25 did not have any previous history of overseas travel, it is likely that Patients #25 and #26 were infected by Patient #27.
- Of the 10 patients with secondary infection and known routes of transmission, 7 were family members including 2 relatives and 3 were acquaintances. All these patients either dined or resided together. Transmission from patients #3 to #6, and from patients #16 to #22 was assumed to have taken place while they dined together at the same place. Patients #6 and #21 did not dine together, but were together for 2 hours at a chapel. Regarding transmission, patients with secondary infection had a history of close contact with the primary patient including physical contact, co-dining, and co-habitation for a considerable amount of time.
- In summary, of the 28 confirmed cases, 16 were index cases imported from abroad, 10 were secondary infection cases, and 2 remained under investigation to determine the route of transmission. As of February 14th, the 28 patients had come into close contact with 1,781 people, of whom 1,356 were released from surveillance, and 457 were under self-quarantine, and active surveillance. The suspected sites of transmission for the 10 patients with secondary infection were the home (7 patients, 60.0%), a restaurant, a church, and other locations (1 patient each, 8.3%). The relationship between the primary patient and patients with secondary infection were as follows: family (7 patients, 70.0%, including 2 relatives) and acquaintances (3 patients, 30.0%). This finding suggests that secondary infection occurred among individuals who were in close contact with an infected person for a considerable amount of time whilst they lived and dined together.
Results
- Among the Korean patients, 15 were men (53.9%). It has been reported that 56%–73.2% of confirmed cases of COVID-19 in Wuhan, China are in men [4,5]. The estimated incubation period was 4.6 days to develop COVID-19, which was shorter than the period of 5.2 days reported in China [5]. The mean age of the Korean patients was 42.6 years, which was lower than the age reported in previous studies conducted in China (49 years, 55.5 years, and 59 years) [2,4,5].
- Chen et al [2] and Huang et al [4] also reported that 32–51% of the hospitalized patients with confirmed COVID-19 had hypertension, diabetes, and cardiovascular diseases, while 10 of the 28 Korean patients (35.7%) had at least 1 underlying disease, including hypertension and diabetes. In addition, the early symptoms, such as a fever, coughing, a sore throat, the chills, and muscle ache, were similar to the reported symptoms of COVID-19 [4].
- Currently, the COVID-19 cases originating in Korea have been reported to be index cases imported from abroad, and resultant first-generation and second-generation cases. So far, all the patients confirmed to have COVID-19 have identifiable epidemiological connections. In other words, cases of secondary infection were limited to closely related people (family and acquaintances) who spent time together co-dining and co-habiting. It is important to analyze and share such epidemiological and clinical data on COVID-19 to establish an effective response strategy.
Discussion
-
Acknowledgements
- We thank the relevant ministries, including the Ministry of Interior and Safety, cities and provinces, medical staff in health centers, and medical facilities for their effort in responding to cases of COVID-19.
Acknowledgments
- 1. World Health Organization [Internet]. Coronavirus disease (COVID-19): Situation reports Geneva (Switzerland): World Health Organization; 2020 [cited 2020 Feb 17]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
- 2. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020;395(10223). 507−13. PMID: 10.1016/S0140-6736(20)30211-7. PMID: 32007143.ArticlePubMedPMC
- 3. Korea Centers for Disease Control and Prevention [Internet]. COVID-19: Health alerts, the fastest updates Cheongju (Korea): Korea Centers for Disease Control and Prevention; 2020 [cited 2020 Feb 14]. Available from: http://ncov.mohw.go.kr/tcmBoardList.do?brdId=&brdGubun=&dataGubun=&ncvContSeq=&contSeq=&board_id=.
- 4. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395(10223). 497−506. PMID: 10.1016/S0140-6736(20)30183-5. PMID: 31986264.ArticlePubMedPMC
- 5. Li Q, Guan X, Wu P, et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. New Engl J Med 2020;Epub 2020 Jan 29. [Epub ahead of print]. PMID: 10.1056/NEJMoa2001316.Article
References
Figure 1
COVID-19 epidemic curve (onset of signs and symptoms).
COVID-19 = coronavirus disease 2019.


Table 1Demographic characteristics of 28 COVID-19 patients in South Korea (N = 28).
| Variables | n | % | |
|---|---|---|---|
| Gender | |||
| Male | 15 | 53.6 | |
| Female | 13 | 46.4 | |
|
|
|||
| Age (y) | |||
| 20–29 | 6 | 21.4 | |
| 30–39 | 6 | 21.4 | |
| 40–49 | 6 | 21.4 | |
| 50–59 | 8 | 28.6 | |
| 60–69 | 1 | 3.6 | |
| 70–79 | 1 | 3.6 | |
|
|
|||
| Nationality | |||
| Korean | 22 | 78.6 | |
| Chinese | 6 | 21.4 | |
|
|
|||
| Signs and Symptoms at onset (may be duplicated) | |||
| Fever | 9 | 32.1 | |
| Sore Throat | 9 | 32.1 | |
| Cough or Sputum | 5 | 17.9 | |
| Chills | 5 | 17.9 | |
| Muscle ache | 4 | 14.3 | |
| Generalized weakness | 3 | 10.7 | |
| Headache | 3 | 10.7 | |
| Asymptomatic infection or Unknown* | 3 | 10.7 | |
|
|
|||
| Pneumonia after admission | |||
| Pneumonia | 18 | 64.3 | |
Table 2Epidemiological characteristics of 28 patients with COVID-19 in South Korea (N = 28).
| Source of infection | n | % | |
|---|---|---|---|
| Case imported | |||
| Wuhan, China | 11 | 68.8 | |
| Zhuhai, China | 1 | 6.3 | |
| Japan | 1 | 6.3 | |
| Singapore | 2 | 12.5 | |
| Thailand | 1 | 6.3 | |
|
|
|||
| Local transmission site | |||
| Residence | 7 | 70.0 | |
| Outside residence | 3 | 30.0 | |
| Hospital | - | - | |
| Airplane | - | - | |
|
|
|||
| Relationship in local transmission | |||
| Family | 5 | 50.0 | |
| Relatives | 2 | 20.0 | |
| Acquaintance | 3 | 30.0 | |
| Co-worker | - | - | |
|
|
|||
| Mean ± SD | Range | ||
|
|
|||
| Incubation period* | 4.1 ± 1.85 | 2–9 | |
Figure & Data
References
Citations
Citations to this article as recorded by 

- Environmental routes of virus transmission and the application of nanomaterial-based sensors for virus detection
Wei Wang, Seju Kang, Wei Zhou, Peter J. Vikesland
Environmental Science: Nano.2023; 10(2): 393. CrossRef - COVID-19: Mechanisms, risk factors, genetics, non-coding RNAs and neurologic impairments
Irina Gilyazova, Yanina Timasheva, Alexandra Karunas, Anastasiya Kazantseva, Albert Sufianov, Andrey Mashkin, Gulnaz Korytina, Yaolou Wang, Ilgiz Gareev, Elza Khusnutdinova
Non-coding RNA Research.2023; 8(2): 240. CrossRef - Asymptomatic infection and transmission of COVID-19 among clusters: systematic review and meta-analysis
K. Ravindra, V.S. Malik, B.K. Padhi, S. Goel, M. Gupta
Public Health.2022; 203: 100. CrossRef - Prevalence of comorbidities and symptoms stratified by severity of illness amongst adult patients with COVID-19: a systematic review
Ritambhara Pandey, Devesh Rai, Muhammad Tahir, Abdul Wahab, Dhrubajyoti Bandyopadhyay, Emil Lesho, Maryrose Laguio-Vila, Emilio Fentanes, Raseen Tariq, Srihari Naidu, Wilbert Aronow
Archives of Medical Science – Atherosclerotic Dise.2022; 7(1): 5. CrossRef - Diagnostic power of one-step and two-step RT-qPCR methods to SARS‑CoV‑2 detection
Asra Malekshahi, Sayyad Khanizadeh, Shirzad Fallahi, Gholamreza Talei, Mehdi Birjandi, Faezeh Hajizadeh
BMC Infectious Diseases.2022;[Epub] CrossRef - Unintended beneficial effects of COVID-19 on influenza-associated emergency department use in Korea
Sola Kim, Ju Ok Park, Hye Ah. Lee, Hang A. Park, Choung Ah. Lee, Soon-Joo Wang, Eun Ju Jung
The American Journal of Emergency Medicine.2022; 59: 1. CrossRef - The Impact of COVID-19 on Psychological and Social Stigma for Indonesian Nurses: A Cross-Sectional Survey
Mustikasari Mustikasari, Harif Fadhillah, Apri Sunadi, Nursalam Nursalam, Ati Surya Mediawati, Muhammad Adam
Frontiers in Psychiatry.2022;[Epub] CrossRef - The Impact of Chest Computed Tomography in A Covid-19 Reference Hospital - First Wave - Distrito Federal - Brazil
Gleim Dias De Souza, Luciana Rodrigues Queiroz De Souza, Gabriela Gomes De Souza, Thales Queiroz Souza, Ulysses Rodrigues Castro, Adriano Guimaraes Ibiapina, Paulo Henrique Ramos Feitosa, Sérgio Aron Ajzen, Ian James Martins
International Journal of Coronaviruses.2022; 4(3): 28. CrossRef - Identification of Bacteria and Fungi in Various Types of Multi-Use Facilities in Bucheon, South Korea
Min-kyeong Kim, Sung chul Seo, Duckshin Park
Environments.2022; 9(11): 136. CrossRef - Identification of Infectious Bacteria and Fungi in Various Types of Multi-Use Facilities in Bucheon, South Korea
Min-kyeong KIM, sung chul Seo, Duckshin Park
SSRN Electronic Journal .2022;[Epub] CrossRef - Response System for and Epidemiological Features of COVID-19 in Gyeongsangnam-do Province in South Korea
Yu Mi Wi, Su Jin Lim, Si-Ho Kim, Seungjin Lim, Su Jin Lee, Byung-Han Ryu, Sun In Hong, Oh-Hyun Cho, Kyunglan Moon, Kyung-Wook Hong, Sunjoo Kim, In-Gyu Bae
Clinical Infectious Diseases.2021; 72(4): 661. CrossRef - A Meta‐Analysis of 67 Studies with Presenting Symptoms and Laboratory Tests of COVID‐19 Patients
Manish Mair, Hitesh Singhavi, Ameya Pai, Jinesh Singhavi, Prachi Gandhi, Peter Conboy, Andrew Baker, Sudip Das
The Laryngoscope.2021; 131(6): 1254. CrossRef - Gastrointestinal and renal complications in SARS‐CoV‐2‐infected patients: Role of immune system
Fatemeh Maghool, Ali Valiani, Tahereh Safari, Mohammad Hassan Emami, Samane Mohammadzadeh
Scandinavian Journal of Immunology.2021;[Epub] CrossRef - Experience of 101 patients with coronavirus infectious disease 2019 (COVID-19) at a tertiary care center in Japan
Kenta Yao, Shinya Hasegawa, Yasuaki Tagashira, Akane Takamatsu, Yuki Uenoyama, Keiki Shimizu, Hitoshi Honda, Yoshiki Nagai, Koichiro Okumura, Tomoko Onda, Takuya Kakutani, Takami Seki, Takuro Sekine, Yasunori Yoshida, Haruka Miyamoto, Kenta Furuhashi, Fuj
Journal of Infection and Chemotherapy.2021; 27(2): 413. CrossRef - Can Stimulus Checks Boost an Economy Under Covid-19? Evidence from South Korea
Moon Jung Kim, Soohyung Lee
International Economic Journal.2021; 35(1): 1. CrossRef - Características y evolución de los pacientes COVID-19 en un centro de salud urbano al inicio de la pandemia
Karen Ruth Barroso López, Paloma Peñasco García, Clara Isabel Soria López, María Carmen Pérez Fernández, José Generoso Gómez Cruz, Yolanda González Silva
Atención Primaria.2021; 53(2): 101957. CrossRef - Clinical Characteristics and Diagnostic Challenges of COVID−19: An Update From the Global Perspective
S. M. Hasan Israfil, Md. Moklesur Rahman Sarker, Parisa Tamannur Rashid, Ali Azam Talukder, Khandkar Ali Kawsar, Farzana Khan, Selina Akhter, Chit Laa Poh, Isa Naina Mohamed, Long Chiau Ming
Frontiers in Public Health.2021;[Epub] CrossRef - A new SYBR Green real-time PCR to detect SARS-CoV-2
D. R. Marinowic, G. Zanirati, F. V. F. Rodrigues, M. V. C. Grahl, A. M. Alcará, D. C. Machado, J. C. Da Costa
Scientific Reports.2021;[Epub] CrossRef - Risk factors for SARS-CoV-2 infection in health care workers and prevention measures
Nadezhda I. Shulakova, Aleksey V. Tutelyan, Olga A. Kvasova, Vasiliy G. Akimkin, Alexander V. Konyukhov
Russian Journal of Occupational Health and Industr.2021; 61(1): 34. CrossRef - COVID‐19 in Australia: our national response to the first cases of SARS‐CoV‐2 infection during the early biocontainment phase
Ramon Z. Shaban, Cecilia Li, Matthew V. N. O'Sullivan, John Gerrard, Rhonda L. Stuart, Joanne Teh, Nicole Gilroy, Tania C. Sorrell, Elizabeth White, Shopna Bag, Kate Hackett, Sharon C. A. Chen, Jen Kok, Dominic E. Dwyer, Jonathan R. Iredell, Susan Maddock
Internal Medicine Journal.2021; 51(1): 42. CrossRef - A Meta-analysis on the Role of Children in Severe Acute Respiratory Syndrome Coronavirus 2 in Household Transmission Clusters
Yanshan Zhu, Conor J Bloxham, Katina D Hulme, Jane E Sinclair, Zhen Wei Marcus Tong, Lauren E Steele, Ellesandra C Noye, Jiahai Lu, Yao Xia, Keng Yih Chew, Janessa Pickering, Charles Gilks, Asha C Bowen, Kirsty R Short
Clinical Infectious Diseases.2021; 72(12): e1146. CrossRef - East–West differences in clinical manifestations of COVID‐19 patients: A systematic literature review and meta‐analysis
Xiucheng Liu, Xiang Li, Teng Sun, Hao Qin, Yeqing Zhou, Chenghang Zou, Junli Cao, Hao Zhang
Journal of Medical Virology.2021; 93(5): 2683. CrossRef - Gastroenterological and hepatic manifestations of patients with COVID-19, prevalence, mortality by country, and intensive care admission rate: systematic review and meta-analysis
Mohammad Shehab, Fatema Alrashed, Sameera Shuaibi, Dhuha Alajmi, Alan Barkun
BMJ Open Gastroenterology.2021; 8(1): e000571. CrossRef - Vitamin D and COVID-19: is there a role?
Aysha Habib Khan, Noreen Nasir, Nosheen Nasir, Quratulain Maha, Rehana Rehman
Journal of Diabetes & Metabolic Disorders.2021; 20(1): 931. CrossRef - SARS-CoV-2 routes of transmission and recommendations for preventing acquisition: joint British Infection Association (BIA), Healthcare Infection Society (HIS), Infection Prevention Society (IPS) and Royal College of Pathologists (RCPath) guidance
A. Bak, M.A. Mugglestone, N.V. Ratnaraja, J.A. Wilson, L. Rivett, S.M. Stoneham, J. Bostock, S.E. Moses, J.R. Price, M. Weinbren, H.P. Loveday, J. Islam, A.P.R. Wilson
Journal of Hospital Infection.2021; 114: 79. CrossRef - SARS-Cov2: a meta-analysis of symptom distribution by continent in 7310 adult COVID-19 infected patients
Hitesh Singhavi, Ameya Pai, Manish Mair, Jinesh Singhavi, Prachi Gandhi, Andrew Baker, Sudip Das, Sanjeev Kumar, Peter Conboy
VirusDisease.2021; 32(3): 400. CrossRef - Differences in seroprevalence between epicenter and non-epicenter areas of the COVID-19 outbreak in South Korea
Hye Won Jeong, Hyun-Ha Chang, Eun Ji Kim, Yu Kyung Kim, Se-Mi Kim, Eun-Ha Kim, Young-Il Kim, Mark Anthony B. Casel, Seong-Gyu Kim, Rare Rollon, Seung-Gyu Jang, Kwang-Min Yu, Hee-Sung Kim, Hee Sue Park, Su-Jin Park, Yong-Dae Kim, Eung-Gook Kim, Young Ki Ch
Journal of Microbiology.2021; 59(5): 530. CrossRef - Upper respiratory tract and otolaryngological manifestations of coronavirus disease 2019 (COVID-19): A systemic review
Jamil N Al-Swiahb, Mohammed A Motiwala
SAGE Open Medicine.2021; 9: 205031212110169. CrossRef - Antiviral peptides against the main protease of SARS-CoV-2: A molecular docking and dynamics study
Shafi Mahmud, Suvro Biswas, Gobindo Kumar Paul, Mohasana Akter Mita, Shamima Afrose, Md. Robiul Hasan, Mst. Sharmin Sultana Shimu, Mohammad Abu Raihan Uddin, Md. Salah Uddin, Shahriar Zaman, K.M. Kaderi Kibria, Md. Arif Khan, Talha Bin Emran, Md. Abu Sale
Arabian Journal of Chemistry.2021; 14(9): 103315. CrossRef - Ações de vigilância à saúde integradas à Atenção Primária à Saúde diante da pandemia da COVID-19: contribuições para o debate
Nilia Maria de Brito Lima Prado, Daniela Gomes dos Santos Biscarde, Elzo Pereira Pinto Junior, Hebert Luan Pereira Campos dos Santos, Sara Emanuela de Carvalho Mota, Erica Lima Costa de Menezes, Josilene Silva Oliveira, Adriano Maia dos Santos
Ciência & Saúde Coletiva.2021; 26(7): 2843. CrossRef - Asymptomatic SARS-CoV-2 infection: A systematic review and meta-analysis
Pratha Sah, Meagan C. Fitzpatrick, Charlotte F. Zimmer, Elaheh Abdollahi, Lyndon Juden-Kelly, Seyed M. Moghadas, Burton H. Singer, Alison P. Galvani
Proceedings of the National Academy of Sciences.2021;[Epub] CrossRef - Gastrointestinal and hepatic diseases during the COVID-19 pandemic: Manifestations, mechanism and management
Dina Zakaria Mohamed, Mai El-Sayed Ghoneim, Sally El-Sayed Abu-Risha, Ramy Ahmed Abdelsalam, Mohamed Abdelhalem Farag
World Journal of Gastroenterology.2021; 27(28): 4504. CrossRef - Pneumonia-targeted lopinavir/ritonavir-based treatment for patients with COVID-19: an early-period retrospective single center observational study
Jongkyu Kim, Jiwoong Jung, Tae Ho Kim, Naree Kang, Hanzo Choi, Dong Hyun Oh, Mi Young Ahn, Su hyun Kim, Chorom Hahm, Young Kyong Lee, Keunhong Park, Kiho Hong, Jae-phil Choi
BMC Infectious Diseases.2021;[Epub] CrossRef - A Comprehensive Overview of the Newly Emerged COVID-19 Pandemic: Features, Origin, Genomics, Epidemiology, Treatment, and Prevention
Md. Sarker, A. Hasan, Md. Rafi, Md. Hossain, H. El-Mageed, Reem Elsapagh, Raffaele Capasso, Talha Emran
Biologics.2021; 1(3): 357. CrossRef - Impact of COVID-19 Pandemic on Cancer Surgical Services—AIIMS, New Delhi Experience
S. V. S. Deo, Sunil Kumar, Mukurdipi Ray, Sandeep Bhoriwal, Ashutosh Mishra, Jyoti Sharma, Raghuram K, Naveen Kumar, Jyoutishman Saikia, Babul Bansal, Amitabha Mandal, Kunal Dhall, Manish Gaur, Sourabh Nandi, Madiwalesh Chhebbi, Sushma Bhatnagar, Seema Mi
Indian Journal of Surgical Oncology.2021; 12(S2): 294. CrossRef - Effectiveness for the Response to COVID-19: The MERS Outbreak Containment Procedures
Hae-Wol Cho
Osong Public Health and Research Perspectives.2020; 11(1): 1. CrossRef - Coronavirus Disease-19: Summary of 2,370 Contact Investigations of the First 30 Cases in the Republic of Korea
Osong Public Health and Research Perspectives.2020; 11(2): 81. CrossRef - Clinical Course and Outcomes of Patients with Severe Acute Respiratory Syndrome Coronavirus 2 Infection: a Preliminary Report of the First 28 Patients from the Korean Cohort Study on COVID-19
Eu Suk Kim, Bum Sik Chin, Chang Kyung Kang, Nam Joong Kim, Yu Min Kang, Jae-Phil Choi, Dong Hyun Oh, Jeong-Han Kim, Boram Koh, Seong Eun Kim, Na Ra Yun, Jae-Hoon Lee, Jin Yong Kim, Yeonjae Kim, Ji Hwan Bang, Kyoung-Ho Song, Hong Bin Kim, Ki-hyun Chung, My
Journal of Korean Medical Science.2020;[Epub] CrossRef - COVID-19 in otolaryngologist practice: a review of current knowledge
Joanna Krajewska, Wojciech Krajewski, Krzysztof Zub, Tomasz Zatoński
European Archives of Oto-Rhino-Laryngology.2020; 277(7): 1885. CrossRef - Coronavirus Disease Outbreak in Call Center, South Korea
Shin Young Park, Young-Man Kim, Seonju Yi, Sangeun Lee, Baeg-Ju Na, Chang Bo Kim, Jung-il Kim, Hea Sook Kim, Young Bok Kim, Yoojin Park, In Sil Huh, Hye Kyung Kim, Hyung Jun Yoon, Hanaram Jang, Kyungnam Kim, Yeonhwa Chang, Inhye Kim, Hyeyoung Lee, Jin Gwa
Emerging Infectious Diseases.2020; 26(8): 1666. CrossRef - Risk factors for predicting mortality in elderly patients with COVID-19: A review of clinical data in China
Char Leung
Mechanisms of Ageing and Development.2020; 188: 111255. CrossRef - Letter: Neurological Implications of COVID-19 and Lessons Learned From Prior Epidemics and Pandemics
Badih J Daou, Sravanthi Koduri, Gregory Palmateer, B Gregory Thompson, Neeraj Chaudhary, Joseph J Gemmete, Aditya S Pandey
Neurosurgery.2020; 87(2): E234. CrossRef - Guiding Principles for Cancer Surgery during the COVID-19 Pandemic
S. V. S. Deo, Sunil Kumar, Naveen Kumar, Jyoutishman Saikia, Sandeep Bhoriwal, Sushma Bhatnagar, Atul Sharma
Indian Journal of Surgical Oncology.2020; 11(S1): 3. CrossRef - The CoV-2 outbreak: how hematologists could help to fight Covid-19
Sara Galimberti, Chiara Baldini, Claudia Baratè, Federica Ricci, Serena Balducci, Susanna Grassi, Francesco Ferro, Gabriele Buda, Edoardo Benedetti, Rita Fazzi, Laura Baglietto, Ersilia Lucenteforte, Antonello Di Paolo, Mario Petrini
Pharmacological Research.2020; 157: 104866. CrossRef - Comparison of Epidemiological Variations in COVID-19 Patients Inside and Outside of China—A Meta-Analysis
Ali Ahmed, Areeba Ali, Sana Hasan
Frontiers in Public Health.2020;[Epub] CrossRef - Clinical Features, Diagnosis, and Treatment of COVID-19 in Hospitalized Patients: A Systematic Review of Case Reports and Case Series
Azin Tahvildari, Mahta Arbabi, Yeganeh Farsi, Parnian Jamshidi, Saba Hasanzadeh, Tess Moore Calcagno, Mohammad Javad Nasiri, Mehdi Mirsaeidi
Frontiers in Medicine.2020;[Epub] CrossRef - SARS-CoV-2/COVID-19: Viral Genomics, Epidemiology, Vaccines, and Therapeutic Interventions
Mohammed Uddin, Farah Mustafa, Tahir A. Rizvi, Tom Loney, Hanan Al Suwaidi, Ahmed H. Hassan Al-Marzouqi, Afaf Kamal Eldin, Nabeel Alsabeeha, Thomas E. Adrian, Cesare Stefanini, Norbert Nowotny, Alawi Alsheikh-Ali, Abiola C. Senok
Viruses.2020; 12(5): 526. CrossRef - Neurologic Characteristics in Coronavirus Disease 2019 (COVID-19): A Systematic Review and Meta-Analysis
Rizaldy Taslim Pinzon, Vincent Ongko Wijaya, Ranbebasa Bijak Buana, Abraham Al Jody, Patrick Nalla Nunsio
Frontiers in Neurology.2020;[Epub] CrossRef - AGA Institute Rapid Review of the Gastrointestinal and Liver Manifestations of COVID-19, Meta-Analysis of International Data, and Recommendations for the Consultative Management of Patients with COVID-19
Shahnaz Sultan, Osama Altayar, Shazia M. Siddique, Perica Davitkov, Joseph D. Feuerstein, Joseph K. Lim, Yngve Falck-Ytter, Hashem B. El-Serag
Gastroenterology.2020; 159(1): 320. CrossRef - Detection of Novel Coronavirus on the Surface of Environmental Materials Contaminated by COVID-19 Patients in the Republic of Korea
Sang-Eun Lee, Deog-Yong Lee, Wook-Gyo Lee, ByeongHak Kang, Yoon Suk Jang, Boyeong Ryu, SeungJae Lee, Hyunjung Bahk, Eungyu Lee
Osong Public Health and Research Perspectives.2020; 11(3): 128. CrossRef - COVID-19: from epidemiology to treatment
J M Pericàs, M Hernandez-Meneses, T P Sheahan, E Quintana, J Ambrosioni, E Sandoval, C Falces, M A Marcos, M Tuset, A Vilella, A Moreno, J M Miro, Jose M Miró, Juan Ambrosioni, Juan M Pericàs, Adrian Téllez, Marta Hernandez-Meneses, Delia Garcia-Pares, As
European Heart Journal.2020; 41(22): 2092. CrossRef - Gastrointestinal Manifestations of SARS-CoV-2 Infection and Virus Load in Fecal Samples From a Hong Kong Cohort: Systematic Review and Meta-analysis
Ka Shing Cheung, Ivan F.N. Hung, Pierre P.Y. Chan, K.C. Lung, Eugene Tso, Raymond Liu, Y.Y. Ng, Man Y. Chu, Tom W.H. Chung, Anthony Raymond Tam, Cyril C.Y. Yip, Kit-Hang Leung, Agnes Yim-Fong Fung, Ricky R. Zhang, Yansheng Lin, Ho Ming Cheng, Anna J.X. Zh
Gastroenterology.2020; 159(1): 81. CrossRef - Clinical manifestations and evidence of neurological involvement in 2019 novel coronavirus SARS-CoV-2: a systematic review and meta-analysis
Lei Wang, Yin Shen, Man Li, Haoyu Chuang, Youfan Ye, Hongyang Zhao, Haijun Wang
Journal of Neurology.2020; 267(10): 2777. CrossRef - What do we know about COVID-19? A review article
Júlia Maggi Vieira, Olívia Moura de Paula Ricardo, Carolina Miranda Hannas, Tereza Cristina Moreira Kanadani, Tiago dos Santos Prata, Fábio Nishimura Kanadani
Revista da Associação Médica Brasileira.2020; 66(4): 534. CrossRef - Update on possible animal sources for COVID‐19 in humans
Tanja Opriessnig, Yao‐Wei Huang
Xenotransplantation.2020;[Epub] CrossRef - Why lockdown? Why national unity? Why global solidarity? Simplified arithmetic tools for decision-makers, health professionals, journalists and the general public to explore containment options for the 2019 novel coronavirus
Gerry F. Killeen, Samson S. Kiware
Infectious Disease Modelling.2020; 5: 442. CrossRef - COVID‐19: Focus on the lungs but do not forget the gastrointestinal tract
Wiktor Smyk, Maciej K. Janik, Piero Portincasa, Piotr Milkiewicz, Frank Lammert, Marcin Krawczyk
European Journal of Clinical Investigation.2020;[Epub] CrossRef - Headache is an important symptom in patients with coronavirus disease 2019 (COVID-19)
Giuseppe Lippi, Camilla Mattiuzzi, Chiara Bovo, Brandon Michael Henry
Diagnosis.2020; 7(4): 409. CrossRef - Diabetes and COVID-19: Global and regional perspectives
In-Kyung Jeong, Kun Ho Yoon, Moon Kyu Lee
Diabetes Research and Clinical Practice.2020; 166: 108303. CrossRef - Clinical Epidemiology of Coronavirus Disease 2019:Defined on Current Research
Fengyu Zhang, Claude Hughes
Global Clinical and Translational Research.2020; : 54. CrossRef - The concern about ACE/ARB and COVID-19: Time to hold your horses!
Joseph V. Pergolizzi, Giustino Varrassi, Peter Magnusson, Jo Ann LeQuang, Marianna Leopoulou, Antonella Paladini, Robert Taylor, Charles Wollmuth, Frank Breve
Journal of the American Pharmacists Association.2020; 60(6): e88. CrossRef - Comorbidities, clinical signs and symptoms, laboratory findings, imaging features, treatment strategies, and outcomes in adult and pediatric patients with COVID-19: A systematic review and meta-analysis
Catherine R. Jutzeler, Lucie Bourguignon, Caroline V. Weis, Bobo Tong, Cyrus Wong, Bastian Rieck, Hans Pargger, Sarah Tschudin-Sutter, Adrian Egli, Karsten Borgwardt, Matthias Walter
Travel Medicine and Infectious Disease.2020; 37: 101825. CrossRef - Clinical Features and Outcomes of 105 Hospitalized Patients With COVID-19 in Seattle, Washington
Frederick S Buckner, Denise J McCulloch, Vidya Atluri, Michela Blain, Sarah A McGuffin, Arun K Nalla, Meei-Li Huang, Alex L Greninger, Keith R Jerome, Seth A Cohen, Santiago Neme, Margaret L Green, Helen Y Chu, H Nina Kim
Clinical Infectious Diseases.2020; 71(16): 2167. CrossRef - An adapted emergency department triage algorithm for the COVID‐19 pandemic
Douglas W. Wallace, Samuel L. Burleson, Matthew A. Heimann, James C. Crosby, Jonathan Swanson, Courtney B. Gibson, Christopher Greene
Journal of the American College of Emergency Physi.2020; 1(6): 1374. CrossRef - Containment of a healthcare-associated COVID-19 outbreak in a university hospital in Seoul, Korea: A single-center experience
Sei Won Kim, Sung Jin Jo, Heayon Lee, Jung Hwan Oh, Jihyang Lim, Sang Haak Lee, Jung Hyun Choi, Jehoon Lee, Xia Jin
PLOS ONE.2020; 15(8): e0237692. CrossRef Awareness of Health Professionals on COVID-19 and Factors Affecting It Before and During Index Case in North Shoa Zone, Ethiopia, 2020
Ayele Abebe, Abinet Mekuria, Awraris Balchut
Infection and Drug Resistance.2020; Volume 13: 2979. CrossRef- Considerations for future novel human-infecting coronavirus outbreaks
Georges Sinclair, Philippa Johnstone, Mustafa Aziz Hatiboglu
Surgical Neurology International.2020; 11: 260. CrossRef - Real Asymptomatic SARS-CoV-2 Infection Might be Rare: the Importance of Careful Interviews and Follow-up
Tae Heum Jeong, Chuiyong Pak, Minsu Ock, Seock-Hwan Lee, Joung Sik Son, Young-Jee Jeon
Journal of Korean Medical Science.2020;[Epub] CrossRef - Identifying common baseline clinical features of COVID-19: a scoping review
Daniela Ferreira-Santos, Priscila Maranhão, Matilde Monteiro-Soares
BMJ Open.2020; 10(9): e041079. CrossRef - Potential sources, modes of transmission and effectiveness of prevention measures against SARS-CoV-2
G. Kampf, Y. Brüggemann, H.E.J. Kaba, J. Steinmann, S. Pfaender, S. Scheithauer, E. Steinmann
Journal of Hospital Infection.2020; 106(4): 678. CrossRef - Gastrointestinal insights during the COVID-19 epidemic
Kai Nie, Yuan-Yuan Yang, Min-Zi Deng, Xiao-Yan Wang
World Journal of Clinical Cases.2020; 8(18): 3934. CrossRef - Response to COVID-19 in South Korea and implications for lifting stringent interventions
Amy Dighe, Lorenzo Cattarino, Gina Cuomo-Dannenburg, Janetta Skarp, Natsuko Imai, Sangeeta Bhatia, Katy A. M. Gaythorpe, Kylie E. C. Ainslie, Marc Baguelin, Samir Bhatt, Adhiratha Boonyasiri, Nicholas F. Brazeau, Laura V. Cooper, Helen Coupland, Zulma Cuc
BMC Medicine.2020;[Epub] CrossRef - A Public-Private Partnership Model to Build a Triage System in Response to a COVID-19 Outbreak in Hanam City, South Korea
Seong Su Ku, Young June Choe
Osong Public Health and Research Perspectives.2020; 11(5): 339. CrossRef - Gastrointestinal and hepatic manifestations of COVID-19 infection: Lessons for practitioners
Syed B Pasha, Ahmed Swi, Ghassan M Hammoud
World Journal of Meta-Analysis.2020; 8(5): 348. CrossRef - Emergency exploratory laparotomy in a COVID-19 patient - A case report -
Seong Su Lee, Ji Hyun Park, Gunn Hee Kim, Mi Young Kwon, Hee Yeong Kim, Yeon Jin Moon, Su Jin Kim, Mi Jung Yun
Anesthesia and Pain Medicine.2020; 15(4): 498. CrossRef - Effectiveness of contact tracing and quarantine on reducing COVID-19 transmission: a retrospective cohort study
R. Malheiro, A.L. Figueiredo, J.P. Magalhães, P. Teixeira, I. Moita, M.C. Moutinho, R.B. Mansilha, L.M. Gonçalves, E. Ferreira
Public Health.2020; 189: 54. CrossRef - What is the clinical course of patients hospitalised for COVID-19 treatment Ireland: a retrospective cohort study in Dublin’s North Inner City (the ‘Mater 100’)
Brendan O’Kelly, Colm Cronin, Stephen Peter Connolly, Walter Cullen, Gordana Avramovic, Tina McHugh, Eileen O’Connor, Aoife Cotter, Peter Doran, Tara McGinty, Dermot S O’Callaghan, Sean Gaine, Gerard Sheehan, Eamonn Brazil, Brian Marsh, John S. Lambert
HRB Open Research.2020; 3: 80. CrossRef - Delay-adjusted age- and sex-specific case fatality rates for COVID-19 in South Korea: Evolution in the estimated risk of mortality throughout the epidemic
A.T. Newall, R.N.F. Leong, A. Nazareno, D.J. Muscatello, J.G. Wood, W.J. Kim
International Journal of Infectious Diseases.2020; 101: 306. CrossRef - Clinical presentations, laboratory and radiological findings, and treatments for 11,028 COVID-19 patients: a systematic review and meta-analysis
Carlos K. H. Wong, Janet Y. H. Wong, Eric H. M. Tang, C. H. Au, Abraham K. C. Wai
Scientific Reports.2020;[Epub] CrossRef - Pain as clinical manifestations of COVID-19 infection and its management in the pandemic era: a literature review
I. Putu Eka Widyadharma, Ni Nyoman Shinta Prasista Sari, Kadek Enny Pradnyaswari, Kadek Tresna Yuwana, I. Putu Gede Danika Adikarya, Clarissa Tertia, I. A. Sri Wijayanti, I. A. Sri Indrayani, Desak Ketut Indrasari Utami
The Egyptian Journal of Neurology, Psychiatry and .2020;[Epub] CrossRef - Clinical spectrum of coronavirus disease 2019 in Iceland: population based cohort study
Elias Eythorsson, Dadi Helgason, Ragnar Freyr Ingvarsson, Helgi K Bjornsson, Lovisa Bjork Olafsdottir, Valgerdur Bjarnadottir, Hrafnhildur Linnet Runolfsdottir, Solveig Bjarnadottir, Arnar Snaer Agustsson, Kristin Oskarsdottir, Hrafn Hliddal Thorvaldsson,
BMJ.2020; : m4529. CrossRef - Coronavirus Disease 2019 (COVID-19): The Singapore Experience. A Review of the First Eight Months
Trevor Hwee Yong Tan, Matthias Paul Han Sim Toh, Shawn Vasoo, David Chien Boon Lye, Brenda Sze Peng Ang, Yee Sin Leo, Vernon Jian Ming Lee, Ser Hon Puah, Asok Kurup
Annals of the Academy of Medicine, Singapore.2020; 49(10): 764. CrossRef - Available evidence on risk factors associated with COVID-19's poorer outcomes, worldwide and in Brazil
Bruna Rinaldi, João Pedro S. N. Rinaldi
REVISTA CIÊNCIAS EM SAÚDE.2020; 10(2): 80. CrossRef - Early cases of SARS-CoV-2 infection in Uganda: epidemiology and lessons learned from risk-based testing approaches – March-April 2020
Richard Migisha, Benon Kwesiga, Bernadette Basuta Mirembe, Geofrey Amanya, Steven N. Kabwama, Daniel Kadobera, Lilian Bulage, Godfrey Nsereko, Ignatius Wadunde, Tonny Tindyebwa, Bernard Lubwama, Atek A. Kagirita, John T. Kayiwa, Julius J. Lutwama, Amy L.
Globalization and Health.2020;[Epub] CrossRef



 PubReader
PubReader ePub Link
ePub Link Cite
Cite