Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 13(5); 2022 > Article
-
Review Article
India’s efforts to achieve 1.5 billion COVID-19 vaccinations: a narrative review -
Kapil Singh1
 , Ashwani Verma2
, Ashwani Verma2 , Monisha Lakshminarayan3
, Monisha Lakshminarayan3
-
Osong Public Health and Research Perspectives 2022;13(5):316-327.
DOI: https://doi.org/10.24171/j.phrp.2022.0104
Published online: October 14, 2022
1Asia Pacific Vaccine Access Facility, Asian Development Bank, New Delhi, India
2School of Pharmaceutical and Populations Health Informatics, DIT University, Uttarakhand, India
3Global Development Network, New Delhi, India
- Corresponding author: Ashwani Verma School of Pharmaceutical and Populations Health Informatics, DIT University, Mussoorie, Diversion Road, Makka Wala, Uttarakhand 248009, India E-mail: vamit1989@gmail.com
© 2022 Korea Disease Control and Prevention Agency.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Abstract
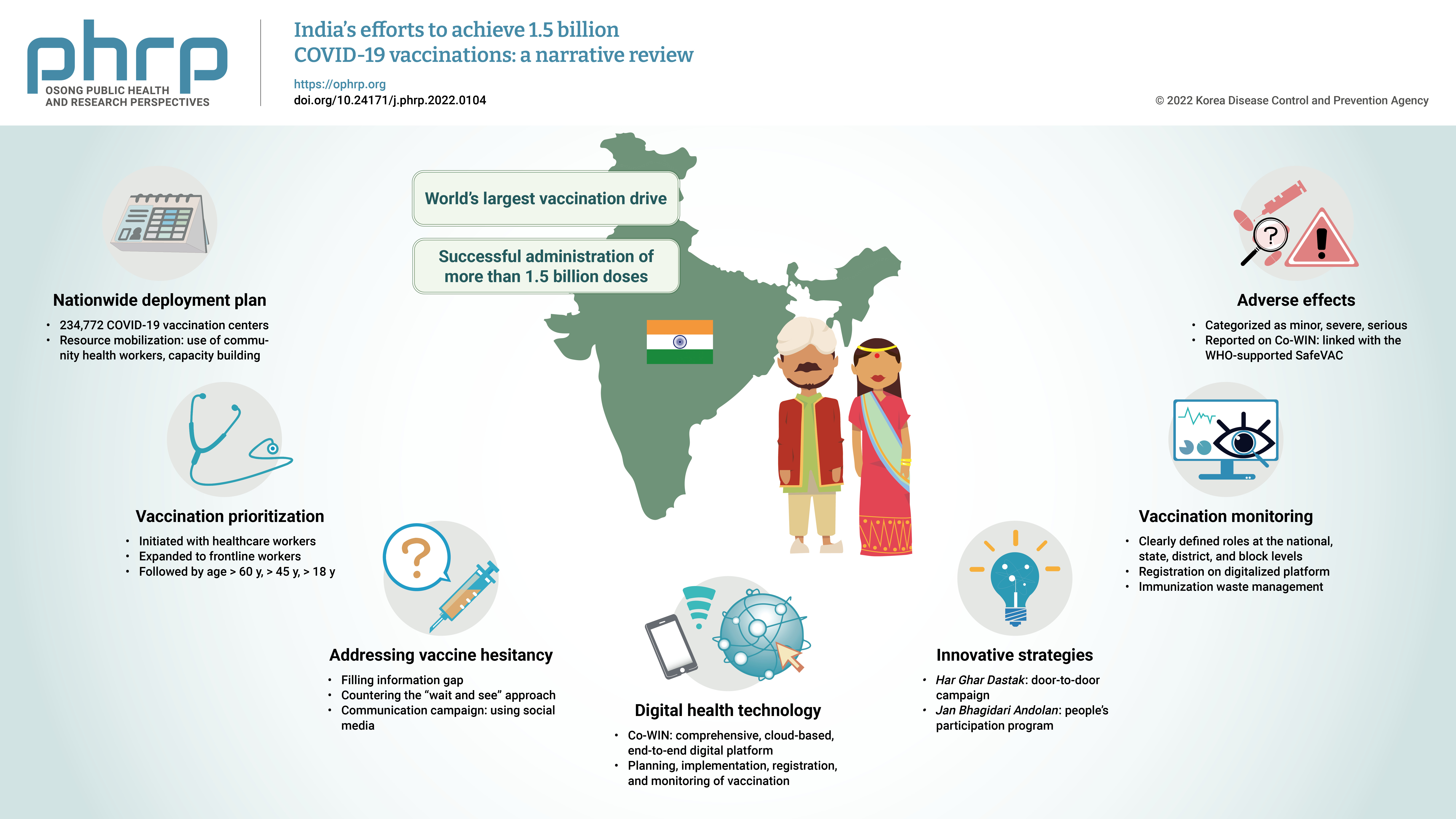
- The initial case of coronavirus disease 2019 (COVID-19) in India was reported on January 30, 2020, and subsequently, the number of COVID-19-infected patients surged during the first wave of April 2020 and the second wave in the same month of 2021. The government of India imposed a strict nationwide lockdown in April 2020 and extended it until May 2020. The second wave of COVID-19 in India overwhelmed the country’s health facilities and exhausted its medical and paramedical workforce. This narrative review was conducted with the aim of summarizing the evidence drawn from policy documents of governmental and non-governmental organizations, as well as capturing India's COVID-19 vaccination efforts. The findings from this review cover the Indian government's vaccination initiatives, which ranged from steps taken to combat vaccine hesitancy to vaccination roadmaps, deployment plans, the use of digital health technology, vaccination monitoring, adverse effects, and innovative strategies such as Har Ghar Dastak and Jan Bhagidari Andolan (people’s participation). These efforts collectively culminated in the successful administration of more than 1.8 billion doses of COVID-19 vaccines in India. This review also provides insights into other countries’ responses to COVID-19 and guidance for future pandemics.
- In January 2020, the World Health Organization (WHO) classified coronavirus disease 2019 (COVID-19) as a public health emergency of international concern and declared it a pandemic on March 11, 2020 [1]. As of December 31, 2021 in India, 34,822,040 COVID-19 cases had been confirmed with a case fatality rate of 1.36% after the earliest case was identified in Kerala, India on January 30, 2020 [2]. India, a low- and middle-income country, has a population of about 1.3 billion people and accounts for nearly 18% of the global population [3]. In India, the first wave of COVID-19 cases peaked in September 2020, followed by a distressing second wave that began in March 2021 and with the highest peak of more than 414,000 cases on May 7, 2021 [4].
- In India, the second wave of COVID-19 overwhelmed the country's health facilities, shattering health workers who became infected [5]. COVID-19 has had a profound impact on public health and the economy [6]. To appropriately respond to COVID-19, a range of containment and mitigation strategies were implemented, with the goal of averting large surges of patients in hospitals and safeguarding the most vulnerable people, such as the elderly and those with comorbidities [7]. Despite national and sub-national containment measures of COVID-19, the testing capacity of over 2.2 million samples within 24 hours to detect and isolate cases [8] and a nationwide vaccination drive, the probability of a third wave is high due to highly contagious mutant strains and variants. The WHO’s technical advisory group evaluated the B.1.1.529 variant of COVID-19, initially reported in South Africa, as “Omicron,” which has many mutations, and considered this as a variant of concern [9].
- As stated by the WHO, ending the COVID-19 pandemic would require equitable access to safe and effective vaccines, which have been shown to be effective and lifesaving [10].
- Based on the experience of India from the existing largest immunization program named as ‘Universal Immunization Program’ (UIP) which targets nearly 26 million infants every year to deliver vaccines against 12 vaccine preventable diseases in the country [11]. India conceptualized to immediately rollout the COVID-19 vaccination program leveraging the existing established infrastructure for the supply, storage and delivery of vaccines to the last mile, under the UIP, where around 600 million doses are administered each year the children every year. The universal immunization program has experiences of implementing large scale immunization campaigns. The country has been carrying out large scale Polio campaigns over more than 2 decades now [12]. Further, World’s largest Measles-Rubella Campaign covering more than 324 million children in the age group of 9 months to 15 years, from 2017 through 2020 has been implemented [13]. Data from various studies conducted in India reported MR vaccine coverage ranging from 80% to 90% [14,15], which depicts the implementation and high coverage of vaccination campaigns.
- The strength of the UIP made India confident to roll out COVID-19 vaccinations programme on January 16, 2021. By December 31, 2021, more than 1.45 billion vaccine doses had been administered, with 64% of the target population vaccinated with 2 doses and 89% vaccinated with the first dose [16], and the target set by India was to vaccinate 944.7 million adults ages 18 years or older (68.9% of the total population) [17]. However, in light of the emerging threat posed by the Omicron variant, India on December 25, 2021 announced that it would vaccinate children aged 15 to 18 years and administer additional doses to health care workers, frontline workers, and people aged 60 years and above with comorbidities [18].
- According to the trends observed in COVID-19 vaccination program in India, India is among the nations with the highest COVID-19 vaccination coverage globally, with 68% of the Indian population fully vaccinated as compared to 0% in January 2021, which is a proportion higher than the global COVID-19 vaccination coverage [10].
- This narrative review was undertaken with the goal of summarizing the vaccination strategies adopted by the government of India to contain the COVID-19 pandemic. The findings from this review could be beneficial for other low- and middle-income countries’ containment and immunization efforts, enabling more effective decision-making.
- Impact on the Health System
- This pandemic has placed a huge burden on India’s healthcare system, exposing long-standing deficiencies and exacerbating preexisting disparities. In the country, there are currently 5 hospital beds and 9 doctors per 10,000 inhabitants, highlighting the strain on the medical community and health infrastructure [19,20]. The abrupt and unexpected rise in the number of cases, especially in the second wave, led to a major scarcity of medical oxygen [21]. Due to the fear of catching COVID-19 and movement restrictions, supply-side interruptions and reduced health-seeking behavior had a negative impact on the delivery of vital and emergency healthcare services. The number of babies delivered at health care institutions was reduced by 45% [21], raising the risk of infection and maternal complications from risky delivery practices. Making matters worse, more than 80% of the population still lacks adequate health insurance coverage [22].
Introduction
- Narrative reviews usually discuss the “state of the art” on a distinct subject from a contextual or theoretical point of view [23]. This narrative review was conducted with the aim of summarizing the government of India’s actions and response against the COVID-19 pandemic.
- Search Terms and Strategy
- A literature search was conducted on March 24, 2022 using the search terms “coronavirus,” “coronavirus disease,” “COVID-19,” and “COVID-19 vaccine” among the government of India’s ministries’ publications, guidelines, and websites, such as the Ministry of Health and Family Welfare (MoHFW), Ministry of Home Affairs, Ministry of Women and Child Development, Ministry of Statistics & Programme Implementation, and Ministry of Railways from April 2020 to March 2022. Additionally, United Nations organizations such as the WHO, World Bank, United Nations Development Programme, United Nations International Children’s Emergency Fund (UNICEF), and the Asian Development Bank documents were also searched. We also searched websites of non-governmental organizations working in the field of vaccination uptake in India for pertinent documents and publications. In addition to searching the above-mentioned databases, we screened the bibliographies of included studies and located more eligible studies. The searches were executed independently by 2 reviewers on the review team.
- Policy documents and guidelines published in the above-identified databases on COVID-19 vaccination in India were included. There were no restrictions on study design for inclusion in the current review. Policies and guidelines for countries other than India were excluded. Documents based on vaccine initiatives other than COVID-19 vaccines were also excluded.
- Data Synthesize and Analysis
- Based on the review's objectives, data synthesis was carried out in an iterative manner. The information was extracted under the below-given broad qualitative themes that were predetermined by 2 independent authors.
- 1. COVID-19 vaccination program planning and implementation
- 2. Policies developed for COVID-19 vaccination
- 3. Prioritization of beneficiaries for COVID-19 vaccination
- 4. Vaccine regulations and available vaccine options
- 5. Vaccine hesitancy and Information, Education & Communication (IEC)campaign
- 6. Vaccine monitoring and planning
- 7. Service delivery system
- 8. Digital health solution for COVID-19 vaccination: Co-WIN
- 9. Innovations for COVID-19 vaccination
- 10. Adverse events following immunization
- After data extraction, the review team organized and analyzed the data that emerged under broad themes. Following that, a slew of sub-themes emerged. We attempted to go beyond simply describing and summarizing the major elements of the included studies in our analysis. Instead, we attempted to draw comparisons based on similarities and differences between studies, as well as to investigate relationships within the data.
Materials and Methods
- Nationwide Vaccination Planning
- India developed its COVID-19 vaccination program according to 3 parameters: (1) Epidemiological and scientific evidence; (2) WHO guidelines for COVID-19 vaccines; (3) Best practices on vaccination around the globe.
- Based on a methodical edge-to-edge management technique, India’s COVID-19 vaccination program was accomplished by the efficient and effective engagement of states/Union Territories and the community. The government of India has been steadfast and assertive in its commitment to the COVID-19 vaccination program, which ranges from expanding research and development capacity to enabling vaccine production to vaccinate every Indian individual at the utmost priority.
- • The government of India’s vaccination plan is based on scientific methodology that has consisted of the following early and proactive steps since April 2020
- • The Task Force for Focused Research on the COVID-19 Vaccine was established in April 2020 to encourage in-house research and development of drugs, diagnostics, and vaccines.
- • The National Expert Group on Vaccine Administration for COVID-19 (NEGVAC) was constituted in August 2020 to articulate a comprehensive action plan for vaccination.
- • The Empowered Group on Vaccine Administration for COVID-19 was constituted in January 2021 to expedite the optimal utilization of information technology to make COVID-19 vaccination inclusive, transparent, operable, and scalable.
- As an essential requirement for COVAX AMC92 countries, India developed a COVID-19 National Deployment and Vaccination Plan (NDVP) [24], and has relied on guidance from the NEGVAC to guide its deployment activities. The NDVP delivers a robust and comprehensive vaccine deployment strategy that incorporates all key aspects as described [25]. To achieve equitable vaccination, the government has developed a number of policies, including free vaccination at public vaccination centers, several registration alternatives, including help for individuals with disabilities, and multiple delivery modes, such as near-to-home outreach camps [26]. India has followed a need-based approach for the country's COVID-19 vaccination program, which was initiated with the vaccination of all healthcare workers. With time, the program was expanded to frontline workers and people over the age of 60, followed by the population over the age of 18 years.
- The government of India revised the guidelines for direct procurement of vaccine es and inoculation strategies in response to state government recommendations. Effective from May 1, 2021, state governments and the government of India procured COVID-19 vaccines on a 50–50 sharing regime. Vaccines procured through the government of India will be provided to states free of cost for administration to predefined priority groups [27]. The revised guideline dated June 21, 2021 increased the government of India’s share of vaccine procurement to 75% of the total vaccines being produced by the manufacturer and stated that the government of India would deliver these vaccines to states and Union Territories free of cost based on predefined allocation criteria [27]. Therefore, government COVID-19 vaccination centers (CVCs) are inoculating citizens for COVID-19 free of charge. The government of India also provides the number of vaccines allocated to states beforehand for robust planning and further peripheral level allocation.
- A few states, along with smaller and more rural private hospitals subsequently reported trouble with handling vaccine financing, procurement, and logistics, which slowed the national COVID-19 vaccination program’s progress. States were also supposed to make vaccine availability information available at the district and CVC levels in the public domain and to spread vaccine availability information extensively among the local community, enhancing visibility and accessibility for the eligible population. Domestic vaccine makers were provided with an opportunity to provide vaccine doses directly (25% of their production) to private hospitals in order to boost vaccine manufacturing and encourage novel vaccines. Later, the government of India purchased more than 75% of the vaccines and gave them to the states and Union Territories at no cost.
- Based on the regime of 2 vaccination doses per person, it was estimated that around 1,889.4 million vaccine doses would be required to vaccinate 68.91% of the Indian population aged 18 years or above (944.7 million people) [17]. On December 25, 2021, it was decided to update the scientific prioritization and COVID-19 vaccination coverage based on the detection of the Omicron variant, which was categorized as a variant of concern by the WHO, scientific global evidence and practices, along with in-house recommendations from the National Technical Advisory Group on Immunisation and Standing Technical Scientific Committee [18]: (1) Inoculation of Covaxin for children aged 15 to 18 years from January 3, 2022. (2) Based on sequencing and prioritization, healthcare workers and frontline workers will receive a precaution dose from January 10, 2022. (3) Based on the doctor’s advice, a precautionary dose of the COVID-19 vaccine will be provided to all citizens aged 60 and above with a known comorbidity after the completion of 9 months or 39 weeks following the second dose.
- Inoculation with the Corbevax vaccine for children aged 12 to 14 years was planned to start on March 16, 2022, and precautionary doses would be given to all citizens aged 60 years and above on the same date [28]. The priority group-wise vaccine dose requirements are shown in Table 1, and different phases of the COVID-19 vaccination program in India are summarized in Table 2.
- Vaccine Regulations
- The government has developed regulatory recommendations for vaccine development, with special attention paid to COVID-19 vaccines [29]. Two vaccines, Covishield and Covaxin, manufactured by Serum Institute of India and Bharat Biotech International Limited, respectively, have been a part of the government’s COVID-19 national vaccination program since its launch on January 16, 2021. Six other vaccines have been granted approval for emergency use in India. These include:
- • Sputnik V (received emergency use authorization [EUA] from the Drugs Controller General of India in April 2021 and is now being administered in India at private vaccination centers)
- • Moderna (received an EUA in June 2021 for import and deployment by Cipla)
- • Janssen (Johnson & Johnson single-dose vaccine; received an EUA in August 2021)
- • ZyCoV-D (DNA-based vaccine approved for emergency use in those aged 12 years and above in August 2021)
- • Covovax (protein subunit vaccine; EUA received in December 2021)
- • Corbevax (protein subunit vaccine, received an EUA in Dec 2021)
- In addition, the government waived the requirement for a bridging trial for these imported vaccines on May 27, 2021 [30]. This will make it easier to receive imported vaccinations and bulk medication materials, as well as make the best use of domestic fill and finish capabilities. Various vaccine options are available in other South Asian countries, such as Afghanistan (Covishield, AstraZeneca [AZD1222], Sinopharm BIBP COVID-19 vaccine, J&J/Janssen Single-Shot COVID-19 vaccines), Bangladesh (AstraZeneca-Covishield), Pfizer, Sinopharm, and Moderna), Bhutan (AstraZeneca-Oxford, Sinopharm, Moderna) [31]. J&J/Janssen, Pfizer, Moderna, and Novovax are the other vaccines approved in the United States and Europe [32,33].
- Vaccine Hesitancy
- The WHO defined vaccine hesitancy as “delay in acceptance or refusal of vaccines despite availability of vaccine services” [34]. In the near past, vaccine hesitancy has resulted in a 30% rise in measles cases worldwide, including in the USA where measles had been eradicated in 2000 [35]. This prompted the WHO to declare vaccine hesitancy as 1 of the 10 biggest threats to global health. Although India has achieved more than 1.5 billion vaccinations, health care workers and frontline workers have reported general population resistance and apprehension to COVID-19 vaccination in the early stages of the vaccination program, which acted as a critical barrier to service delivery [36]. The COVID-19 Trends and Impact Survey in India has reported a vaccine acceptance rate of 77% among the Indian population and a vaccine hesitancy rate of 23% among respondents, of whom 16% reported “reluctance to vaccine” and 12% reported “not taking COVID-19 vaccines”. The 2 major factors associated with hesitancy were “to wait and see if vaccines are safe” and “I think other people need it more than I do right now” [36]. Alternatively, more than three-quarters of men and 73% of women showed a strong willingness for COVID-19 vaccine uptake. An online survey conducted by Chandani et al. [37] in December 2020 in India found that 67% of the participants showed willingness to receive the COVID-19 the vaccine, 23% were not sure, and one-tenth of the participants refused to receive the vaccine. As compared to other South Asian countries, a study conducted by Marzo et al. [38] reported vaccine hesitancy rates in Indonesia (10.2%), Malaysia (18.8%), Myanmar (7.2%), Philippines (7.7), Thailand (52.1%), and Vietnam (3.7%). Another systematic review conducted by Yasmin et al. [39] on COVID-19 vaccine acceptance in the USA reported the COVID-19 vaccine acceptance rate ranged from 12% to 91.4%, demonstrating a huge gap in vaccine uptake. Another multi-country study conducted by Hawlader reported that the vaccine acceptance rate in India was 65.7%, Pakistan (71.5%), Nepal (74%) and Bangladesh (65%) [40]. The government of India has launched a COVID-19 vaccine communication strategy to address vaccine hesitancy and debunk myths and misconceptions related to COVID-19 vaccines [41].
- Information, Education, and Communication Campaign on Vaccine Hesitancy in India
- United Nations agencies such as UNICEF have developed a series of media campaigns on the following topics in collaboration with the Yale Institute for Global Health, UNICEF, and Facebook [36].
- 1. Filling information gaps with emphasis on vaccine safety and efficacy: This campaign aimed to fill the information gap by reflecting rigorous testing by scientists and advocacy for the COVID-19 vaccine to prevent the spread of COVID-19.
- 2. Countering the “wait and see” approach: This time-based approach highlighted the urgency of the COVID-19 vaccine with a message saying, “Every day you wait to get vaccinated is another day that you could be spreading COVID-19 in your family and community.”
- 3. National pride: With the aim of obtaining social approval for the COVID-19 vaccine through social media, this campaign expressed that India developed an indigenous vaccine that it will share with other countries, with messages such as “Make India #1 in COVID-19 vaccination” and “Don’t let India down, get vaccinated against COVID-19.”
- 4. Testimonials and messengers: An analysis from social media showed that vaccinated individuals shared their vaccination testimonies and also encouraged others to get vaccinated.
- Vaccination Monitoring and Planning
- India is employing a whole-government approach to vaccination deployment, which includes 19 federal ministries of the government of India, state governments, and other government organizations and apex bodies, such as the Indian Council of Medical Research and National Institution for Transforming India (NITI Aayog). Because of their importance, the Prime Minister's office, Parliament, and the Supreme Court, as well as institutional control mechanisms, closely monitor statewide COVID-19 immunization programs. The government has a strong cascading system of decentralized planning, coordination, and implementation procedures with clearly defined roles and responsibilities at the federal, state, district, and block levels. The NEGVAC was established at the national level and offers guidance on all areas of the vaccination strategy, including equitable vaccine procurement and distribution, delivery systems, prioritizing, and safety surveillance [42]. Task forces have been formed at the state, district, and block levels, with clear budget outlay plans for each level under the leadership of state steering committees. There are also operational control rooms at the state, district, and block levels that operate throughout the day and night. Supervisors are also assigned 3–5 vaccination sites, which they visit twice a day.
- With 4 government medical store depots, 37 state vaccine stores, 118 regional vaccine stores, 726 district vaccine stores, and 28,575 sub-district cold chain points located at community health centers, primary health centers (urban and rural), and sub-centers, India has a fully operational cold chain system under the Universal Immunization Programme.
- Service Delivery
- There are around 234,772 CVCs in India, with 215,927 being government-run and 18,845 being privately run [43] with the provision of providing routine immunization services. The system has considerable human resource capacity, with the option of deploying retired auxiliary nurses and midwives, retired staff nurses or nursing assistants, pharmacists, lab technicians, and nursing students on a temporary basis. Each team must have at least 5 professionals to handle verification, crowd management, ensuring COVID-19-appropriate behavior, vaccination, and observation for any potential adverse events following immunization (AEFIs), as well as a supervisor who oversees 3 to 5 vaccination sites [24]. For vaccination, all private facilities that were enrolled in various insurance plans, as well as any other private facilities that met the operational capacity requirements, were engaged. Furthermore, private-sector experts were included in the state, district, and block-level task forces to strengthen engagement. Private facilities can purchase vaccines directly from the manufacturers (up to 25% of their monthly supply) [34]. On April 11, 2021, the government also issued guidelines for private employers to inoculate their eligible employees through private CVCs (workplace vaccination) [44].
- Co-WIN: a Win Over COVID-19
- Co-WIN is a comprehensive, cloud-based, end-to-end, and digital platform for planning, implementation, registration, and monitoring of COVID-19 vaccination from the central to peripheral levels [45,46]. Registration for vaccination on this digitalized platform is obligatory to record vaccination data and ensure transparency and accountability. A single digital public portal could also promote awareness, leaving little room for myths, thereby also addressing the issue of vaccine hesitancy with higher precision. India’s vaccination drive was initiated with the Co-WIN platform and now includes a beneficiary module covering an online pre-registration system, beneficiary verification, beneficiary ID, vaccination slot booking at centers of choice with the vaccination of choice, second-dose follow-up, and a digital vaccination certificate [46]. Co-WIN is linked with other preexisting government digital platforms such as Aarogya Setu, Digilocker, and Umang to download vaccination certificates.
- The Co-WIN platform also ensures that the following tasks are carried out:
- • Verifiable data are available to all vaccinated individuals.
- • A second dose of the same vaccine is provided to the beneficiary.
- • The time prescribed by the government of India guidelines between both doses should be maintained.
- • A vaccine dose is administered to an identifiable individual through verification.
- • The platform provides a linkage between beneficiary registrations and vaccine availability for improved planning.
- • Available data is useful for future pandemic planning and research.
- Furthermore, the digital vaccination data enable the program managers to:
- • Monitor the vaccination status of any state, district, or population group in real time.
- • Monitor vaccine availability and utilization for improved planning at the national level and below.
- • Evaluate vaccine waste and take immediate steps to reduce waste.
- • Make it easier to refer individuals to future digital health interventions, such as the administration of booster shots.
- Registration without Using the Co-Win Portal
- To enable the registration and vaccination of persons without access to a smartphone or the internet, registration of beneficiaries can be done through a common service center. Up to 4 persons can be registered using a mobile phone, allowing the registration of a person by friends and family members. An assisted registration facility is made available through a 1,075 helpline/call center; vaccination slots can also be booked by sending the WhatsApp message “book Slot” to MyGovIndia Corona Helpdesk’s number (+91-9013151515) [47]. This is further backed up by facilities that provide walk-in registration and vaccination. Furthermore, in areas without internet connectivity, vaccination sessions can still be organized. In such cases, the vaccination records are prepared in reporting formats and entered into the Co-WIN platform for the generation of vaccination certificates. The Co-WIN system receives over a billion visits per day and has recorded 3.1 billion visits per day for booking vaccine slots [48].
- Innovations in the Vaccination Drive
- The Indian government launched a month-long door-to-door campaign called Har Ghar Dastak in November 2021 to encourage people to get fully vaccinated, with the goal of covering all eligible beneficiaries with the first dose and all due beneficiaries with the second dose through reaching out to all missed-out and dropped-out eligible beneficiaries via house-to-house visits [49]. The COVID-19 vaccination drive is being coordinated as a Jan Bhagidari Andolan (people’s participation) program and has involved stakeholders from various ministries or departments, medical colleges, media houses, non-governmental organizations, professional organizations, civil service organizations, the private sector, youth, and women’s networks.
- Management of AEFIs
- The Co-WIN platform is linked with the WHO-supported Surveillance and Action for Events Following Vaccination (SafeVAC) application for the monitoring of AEFIs [46]. Adverse events are categorized as minor, severe, and serious, and those following vaccination will be reported in Co-WIN either by the vaccinator or by the district immunization officer (DIO). DIOs can access the Co-WIN SafeVAC for serious or severe AEFIs via a single Co-WIN login and then fill out a case report form, preliminary case investigation form, and final case investigation form and submit the materials. Furthermore, all AEFIs must be recorded in AEFI registers at planning units and notified on a weekly basis. This enables the analysis of AEFI cases using both automated data mining and proper statistical approaches to spot alarming trends quickly.
- Immunization Waste Management
- The biomedical waste management (BMWM) guidelines (2016 and later changes) spell out the requirements for the generation, storage, transportation, disinfection, treatment, and disposal of biomedical waste, which includes vaccination waste [50]. Additional guidance has been provided for BMWM from the COVID-19 immunization program under UIP 2021 [51]. The biomedical waste monitoring software “COVID-19 BWM” was also created for trash generators, carriers, and treatment and disposal facility operators. In the United States, immunization wastage is being reported through VTrckS ExIS (External Information System) interface [52].
- Accessibility of Vaccines to the Marginalized, Women, and Hard-To-Reach Areas
- MoHFW has issued guidelines for differently abled and senior citizens to get vaccinated at nearby CVCs [26], and some states or municipal corporations provide additional services such as beneficiary transportation [53] for vaccination. Special vaccination sessions are also organized at government CVCs for people such as nomads or migrants, inmates in prisons or mental health institutions, elderly home populations, beggars, residents in rehabilitation centers or camps, and any other identified eligible individuals [54].
- Learnings from India’s COVID-19 Vaccination Program
- India’s COVID-19 vaccination program is built on epidemiological evidence, WHO guidelines, and best practices, and it is implemented through a multidimensional approach and active participation of all states and Union Territories. The strategies adopted by India could assist other countries in the implementation of their nationwide vaccination programs in the COVID-19 pandemic or a future pandemic. This may include:
- • Prioritization of the eligible population: India initiated COVID-19 vaccination with health care workers, and then expanded vaccination to frontline workers, the population aged more than 60 years, followed by those aged more than 45 years and eventually the population aged 18 years and above [27]. This step-wise approach may assist other countries in prioritizing their population for vaccination programs in ongoing and future pandemics.
- • Resource mobilization: (1) The use of trained community health workers, such as accredited social health activists (ASHAs), was critical in mobilizing and connecting the community with the health system. An ASHA is a trained female community health activist belonging to the same village who supports routine immunization and other health services. Recently, the WHO named them global health leaders for providing immunization services during the COVID-19 pandemic in India [55]. (2) Capacity building: Quality training has been provided to health care workers involved in providing immunization services for the successful introduction of COVID-19 vaccines in India. These training sessions were followed by the nationwide “dry run” conducted in January 2021, which assisted India in preparing for COVID-19 vaccination. (3) Cold chain management: The temperature of COVID-19 vaccines in India needed to be maintained between +2°C to +8°C and stored in walk-in-coolers at state or regional vaccine stores. The cold chain requirement for COVID-19 vaccines in the immunization supply chain can be estimated based on the calculation given in the operational guidelines (Page 91) for COVID-19 vaccination [25].
- This is easier said than done, as the last-mile logistics of vaccines in a vast country like India is a difficult task. As an alternative, micro-cold storage, which is known to be quiet, hygienic, portable, without moving parts, and dependable for last-mile vaccine logistics was proposed as a method to deliver vaccines to remote rural areas was also proposed [56].
- The manufacturers of vaccines airlifted vaccines in cold boxes with digital temperature tags to 4 major government medical supply depots in Karnal (Haryana), Mumbai, Chennai, and Kolkata, where they are kept in walk-in coolers. The vaccines would then be transported by planes or insulated vans to designated stores in 37 states and Union Territories. The state and Union Territory governments transport them from these 41 centers to temperature-controlled facilities at district-level vaccine stores. Vaccines are stored in ice-lined refrigerators in districts before being transported in cold boxes to distribution centers and then in ice-packed vaccine carriers to vaccination sites. The electronic Vaccine Intelligence Network (eVIN) already monitors the temperature of 29,000 cold chain points in real time [55].
- • Use of digital health technology: Other countries may benefit from digital health technologies, such as Co-WIN for planning, implementation, registration, and monitoring of COVID-19 vaccination for current or future pandemics. This system provides support in scheduling sessions and implementing the vaccination process from the central level to the peripheral level.
- Wherever possible, virtual training methods were used to train human resources. The newer training modalities emphasized “the new normal” (i.e., mitigation of the risk of transmission). The Integrated Govt. Online Training portal on the Ministry of Human Resources and Development's DIKSHA platform for the capacity building of frontline workers on COVID-19 [57].
- • Vaccine hesitancy: India has addressed vaccine hesitancy in a variety of ways [34]. (1) Community engagement with communication approaches to build trust in COVID-19 vaccines. (2) Identification of high-risk groups, areas, and communities known for prior experiences of vaccine hesitancy and the involvement of local leaders to address fear and build trust among those identified. (3) The involvement of influencers at both local and national levels to promote COVID-19 vaccine safety and efficacy. (4) Real-time monitoring of digital media to address myths and misconceptions related to COVID-19 vaccines.
- Limitations
- This narrative review was conducted while India’s COVID-19 vaccination program was still ongoing. New innovations may occur with time; therefore, this review will require a timely update based on the guidelines and policies related to COVID-19 vaccination. This review lacked specific criteria for the selection of articles or documents, and there was no evaluation of the validity of the selected documents. The findings of this review were limited by a lack of quantitative data, as this review reported qualitative data only.
Results and Discussion
- This review summarizes India’s proactive response to COVID-19 through different measures such as vaccination planning and initiatives. Vaccination prioritization, resource mobilization, capacity building, addressing vaccine hesitancy, and embracing digital health technology such as CO-WIN played a vital role in achieving 1.5 billion vaccinations in India. The paper, in a nutshell, attempted to capture the vaccination process and strategies used for the implementation of the national COVID-19 vaccination program in India. The country's healthcare system was largely unprepared to cope with the pandemic, but it resorted to efficient and innovative real-time implementation to deal with it.
- This review contributes guidance as a document for knowledge sharing, which could support other countries in their fight against this pandemic. This review also reflects India’s iterative process of dealing with COVID-19 and provides vital lessons on how to minimize the impact of COVID-19, which will prepare other countries for current and future pandemics. In countries such as India, focusing on social norms and promoting cohesion could be a vital strategy for vaccine hesitancy.
Conclusion
-
Ethics Approval
Not applicable.
-
Conflicts of Interest
The authors have no conflicts of interest to declare.
-
Funding
None.
-
Availability of Data
All data synthesized or analyzed during this review from the eligible articles are included in this published review.
-
Authors’ Contributions
Conceptualization: KS, AV; Methodology: AV; Data curation: AV, ML; Writing-original draft: KS, AV, ML; Writing-review & editing: KS, AV, ML.
Article information
| Phase | Commencement date | Priority group | Eligible population (million) | % of total population | No. of doses required (million)a) |
|---|---|---|---|---|---|
| 1a | January 16, 2021 | Health care workers | 10 | 0.73 | 20.0 |
| 1b | February 2, 2021 | Frontline workers | 20 | 1.46 | 40.0 |
| 2a | March 1, 2021 | Senior citizens (≥60 years) & those above 45 years with defined comorbidities | 138 | 10.07 | 276.1 |
| 2b | April 1, 2021b) | Population 45–59 years of age | 209 | 15.27 | 418.6 |
| 3 | May 1, 2021 | Population 18–44 years of age | 597 | 43.57 | 1,194.7 |
| 4a | January 3, 2022 | Population 15–18 years of age | 74 | 5.41 | 148.2 |
| Total | 1,018.81c) | 74.32 | 2,037.6 | ||
| 4b | January 10, 2022 | Health care workers and frontline workers | 28d) | 28.77 | |
| Senior citizens (≥60 years) | 137 | 137.9 | |||
| 5 | March 16, 2022 | Population 12–14 years of age | 46 | 3.39 | 92.8 |
| Total Doses Required | 77.71 | 2,297.1 |
a) Assuming a 2-dose regime (wastage not factored in).
b) Population aged 45–59 years with comorbidities were made eligible for vaccine access on March 1, 2021 along with the priority group of senior citizens (60 years and above) followed by extension of vaccine access to all citizens aged 45 years and above from April 1, 2021.
c) Population aged 15 and above, 76.51% of total population of 1,371 million. Health care and frontline workers are included in their respective age category.
d) As of December 26, 2021, some health care and frontline workers are still receiving their first doses, and 8.387 received first doses in December 2021.
- 1. World Health Organization (WHO). WHO Director-General’s opening remarks at the media briefing on COVID-19 [Internet]. Geneva: WHO; 2020 [cited 2022 Mar 29]. Available from: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
- 2. Ministry of Health and Family Welfare. COVID-19 statewise status [Internet]. Delhi: Ministry of Health and Family Welfare, Government of India; 2021 [cited 2022 Mar 29]. Available from: https://www.mohfw.gov.in/.
- 3. United Nations Department of Economic and Social Affairs. World population prospects [Internet]. New York: United Nations; 2019 [cited 2022 Mar 29]. Available from: https://www.un.org/en/global-issues/population.
- 4. United Nations Children’s Fund (UNICEF). Geneva Palais briefing note on the impact of the deadly COVID-19 surge on children in India, and increasingly in the region [Internet]. New York: UNICEF; 2021 [cited 2022 Mar 29]. Available from: https://www.unicef.org/press-releases/geneva-palais-briefing-note-impact-deadly-covid-19-surge-children-india-and.
- 5. The Lancet. India’s COVID-19 emergency. Lancet 2021;397:1683. ArticlePubMedPMC
- 6. McKee M, Stuckler D. If the world fails to protect the economy, COVID-19 will damage health not just now but also in the future. Nat Med 2020;26:640−2.ArticlePubMedPDF
- 7. Parodi SM, Liu VX. From containment to mitigation of COVID-19 in the US. JAMA 2020;323:1441−2.ArticlePubMed
- 8. 2020 World Health Organization (WHO). India situation reports [Internet]. Geneva: WHO; 2020 [cited 2022 Mar 29]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
- 9. World Health Organization (WHO). Classification of Omicron (B.1.1.529): SARS-CoV-2 variant of concern [Internet]. Geneva: WHO; 2021 [cited 2022 Mar 29]. Available from: https://www.who.int/news/item/26-11-2021-classification-of-omicron-(b.1.1.529)-sars-cov-2-variant-of-concern.
- 10. World Health Organization (WHO). COVID-19 vaccines [Internet]. Geneva: WHO; 2022 [cited 2022 Mar 29]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines.
- 11. Ministry of Health and Family Welfare. Universal Immunization Program [Internet]. Delhi: Ministry of Health and Family Welfare, Government of India; 2020 [cited 2022 Mar 29]. Available from: https://main.mohfw.gov.in/sites/default/files/5628564789562315.pdf.
- 12. National Health Mission. Pulse Polio Programme [Internet]. NHP; 2015 [cited 2022 Mar 29]. Available from: https://www.nhp.gov.in/pulse-polio-programme_pg.
- 13. World Health Organization (WHO). Moving towards the measles and rubella elimination goal in India [Internet]. Geneva: WHO; 2022 [cited 2022 Mar 29]. Available from: https://www.who.int/india/news/feature-stories/detail/moving-towards-the-measles-and-rubella-elimination-goal-in-india.
- 14. Newtonraj A, Vincent A, Selvaraj K, et al. Status of coverage of MR vaccination, after supplementary immunization activities in a rural area of South India: a rapid immunization coverage survey. Rural Remote Health 2019;19:5261. ArticlePubMed
- 15. Jasmine A. Coverage survey of Measles-Rubella mass vaccination campaign in a rural area in Tamil Nadu. J Family Med Prim Care 2019;8:1884−8.Article
- 16. Ministry of Health and Family Welfare. Co-WIN: Winning over Covid-19 [Internet]. Delhi: Ministry of Health and Family Welfare, Government of India; 2021 [cited 2022 Mar 29]. Available from: https://dashboard.cowin.gov.in.
- 17. Kant A. One billion doses: India’s leadership in the world. NITI Aayog [Internet]. Delhi: NITI Aayog; 2021 [cited 2022 Mar 29]. Available from: https://www.niti.gov.in/one-billion-doses-indias-leadership-world.
- 18. Ministry of Health and Family Welfare. Guidelines for COVID-19 vaccination of children between 15-18 years and precaution dose to HCWs, FLWs & 60+ population with comorbidities [Internet]. Delhi: Ministry of Health and Family Welfare, Government of India; 2022 [cited 2022 Mar 29]. Available from: https://www.mohfw.gov.in/pdf/GuidelinesforCOVID19VaccinationofChildrenbetween15to18yearsandPrecautionDosetoHCWsFLWs&60populationwithcomorbidities.pdf.
- 19. The World Bank. Physicians (per 1,000 people)-India [Internet]. Washington, DC: The World Bank; 2018 [cited 2022 Mar 29]. Available from: https://data.worldbank.org/indicator/SH.MED.PHYS.ZS?locations=IN.
- 20. The World Bank. Hospital beds (per 1,000 people)-India [Internet]. Washington, DC: The World Bank; 2017 [cited 2022 Mar 29]. Available from: https://data.worldbank.org/indicator/SH.MED.BEDS.ZS?locations=IN.
- 21. Ministry of Health and Family Welfare. Union Government takes steps to boost supply of oxygen to hospitals [Internet]. PIB; 2021 [cited 2022 Mar 29]. Available from: https://pib.gov.in/PressReleaseIframePage.aspx?PRID=1712590.
- 22. Goyal M, Singh P, Singh K, et al. The effect of the COVID-19 pandemic on maternal health due to delay in seeking health care: experience from a tertiary center. Int J Gynaecol Obstet 2021;152:231−5.ArticlePubMedPDF
- 23. Rother ET. Systematic literature review X narrative review. Acta Paul Enferm 2007;20.
- 24. Gavi. Country readiness for COVID-19 vaccines [Internet]. Washington, DC: Gavi; 2021 [cited 2022 Mar 29]. Available from: https://www.gavi.org/vaccineswork/country-readiness-covid-19-vaccines.
- 25. Ministry of Health and Family Welfare. COVID-19 vaccines: operational guidelines [Internet]. Delhi: Ministry of Health and Family Welfare, Government of India; 2020 [cited 2022 Mar 29]. Available from: https://www.mohfw.gov.in/pdf/COVID19VaccineOG111Chapter16.pdf.
- 26. Ministry of Health and Family Welfare. Near to Home COVID Vaccination Centres (NHCVC) for elderly and differently abled citizens: guidance note [Internet]. Delhi: Ministry of Health and Family Welfare, Government of India; 2021 [cited 2022 Mar 29]. Available from: https://www.mohfw.gov.in/pdf/GuidanceNeartoHomeCovidVaccinationCentresforElderlyandDifferentlyAbledCitizens.pdf.
- 27. Ministry of Health and Family Welfare. Revised guidelines for implementation of National COVID Vaccination Program [Internet]. Delhi: Ministry of Health and Family Welfare, Government of India; 2021 [cited 2022 Mar 29]. Available from: https://www.mohfw.gov.in/pdf/RevisedVaccinationGuidelines.pdf.
- 28. Kaul R. Vaccination for 12-15 age group to kick-start today. Hindustan Times [Internet]. 2022 [cited 2022 Mar 29]. Available from: https://www.hindustantimes.com/india-news/vaccination-for-12-15-age-group-to-kick-start-today-101647368886533.html.
- 29. Central Drugs Standard Control Organization. Draft regulatory guidelines for development of vaccines with special consideration for COVID-19 vaccine [Internet]. Delhi: Ministry of Health and Family Welfare, Government of India; 2021 [cited 2022 Mar 29]. Available from: https://cdsco.gov.in/opencms/resources/UploadCDSCOWeb/2018/UploadPublic_NoticesFiles/Regulatory_guidelines_for__development_of_Vaccine_20.9.20.pdf.
- 30. Dutta SS. Centre waives “bridging trials” to allow foreign vaccines for emergency use. The New Indian Express [Internet]. 2021 [cited 2022 Mar 29]. Available from: https://www.newindianexpress.com/nation/2021/may/27/centre-waives-bridging-trials-to-allow-foreign-vaccines-for-emergency-use-2308362.html.
- 31. Hayat M, Uzair M, Ali Syed R, et al. Status of COVID-19 vaccination around South Asia. Hum Vaccin Immunother 2022;18:2016010. ArticlePubMedPMC
- 32. Centers for Disease Control and Prevention (CDC). U.S. COVID-19 vaccine product information [Internet]. Atlanta: CDC; 2022 [cited 2022 Mar 29]. Available from: https://www.cdc.gov/vaccines/covid-19/info-by-product/index.html.
- 33. European Commissions. Safe COVID-19 vaccines for Europeans [Internet]. Directorate-General for Communication; 2022 [cited 2022 Mar 29]. Available from: https://ec.europa.eu/info/live-work-travel-eu/coronavirus-response/safe-covid-19-vaccines-europeans_en#securing-safe-and-effective-vaccines.
- 34. Eskola J, Xiaofeng L, Reingold A, Chaudhuri M DE. Report of the SAGE working group on Vaccine hesistancy [Internet]. Geneva: World Health Organization; 2014 [cited 2022 Mar 29]. Available from: https://www.asset-scienceinsociety.eu/sites/default/files/sage_working_group_revised_report_vaccine_hesitancy.pdf.
- 35. Lindmeier C, Rowland A, Fulker J SS. Measles cases spike globally due to gaps in vaccination coverage [Internet]. Geneva: World Health Organization; 2018 [cited 2022 Mar 29]. Available from: https://www.who.int/news/item/29-11-2018-measles-cases-spike-globally-due-to-gaps-in-vaccination-coverage.
- 36. UNICEF India. Building confidence in the COVID-19 vaccine in India [Internet]. New Delhi: UNICEF India; 2021 [cited 2022 Mar 29]. Available from: https://www.unicef.org/india/stories/building-confidence-covid-19-vaccine-india.
- 37. Chandani S, Jani D, Sahu PK, et al. COVID-19 vaccination hesitancy in India: state of the nation and priorities for research. Brain Behav Immun Health 2021;18:100375. ArticlePubMedPMC
- 38. Marzo RR, Sami W, Alam MZ, et al. Hesitancy in COVID-19 vaccine uptake and its associated factors among the general adult population: a cross-sectional study in six Southeast Asian countries. Trop Med Health 2022;50:4. ArticlePubMedPMCPDF
- 39. Yasmin F, Najeeb H, Moeed A, et al. COVID-19 vaccine hesitancy in the United States: a systematic review. Front Public Health 2021;9:770985. ArticlePubMedPMC
- 40. Hawlader MD, Rahman ML, Nazir A, et al. COVID-19 vaccine acceptance in South Asia: a multi-country study. Int J Infect Dis 2022;114:1−10.ArticlePubMed
- 41. Singh P, Dhawan V. Covid-19 vaccine communication strategy [Internet]. Delhi: Ministry of Health and Family Welfare; 2020 [cited 2022 Mar 29]. Available from: https://www.mohfw.gov.in/pdf/Covid19CommunicationStrategy2020.pdf.
- 42. Ministry of Health and Family Welfare. National Expert Group on Vaccine Administration for COVID-19 deliberates on strategy to ensure COVID-19 vaccines’ availability and its delivery mechanism [Internet]. PIB; 2020 [cited 2022 Mar 29]. Available from: https://pib.gov.in/PressReleasePage.aspx?PRID=1645363.
- 43. Pradhan Mantri Jan Arogya Yojana. COVID Vaccination Hospitals [Internet]. National Health Authority; 2021 [cited 2022 Mar 29]. Available from: https://pmjay.gov.in/covid-vaccination-hospitals.
- 44. Ministry of Health and Family Welfare. Guidance on COVID-19 vaccination at work places (government & private) [Internet]. Delhi: Ministry of Health and Family Welfare, Government of India; 2021 [cited 2022 Mar 29]. Available from: https://www.mohfw.gov.in/pdf/GuidelinesforCOVID19VaccinationatWorkplace.pdf.
- 45. Ministry of Health and Family Welfare. Guidance note for CoWIN 2.0 [Internet]. Delhi: Ministry of Health and Family Welfare, Government of India; 2021 [cited 2022 Mar 29]. Available from: https://www.mohfw.gov.in/pdf/GuidancedocCOWIN2.pdf.
- 46. Ministry of Health and Family Welfare. Guidelines for integration of Co-WIN with third-party applications [Internet]. Delhi: Ministry of Health and Family Welfare, Government of India; 2021 [cited 2022 Mar 29]. Available from: https://www.mohfw.gov.in/pdf/CoWINAPIGuidelinesFinal240521.pdf.
- 47. Government of India. India Fights Corona COVID-19 [Internet]. Hyderabad: Government of India; 2020 [cited 2022 Mar 29]. Available from: https://www.mygov.in/covid-19.
- 48. Ministry of Health and Family Welfare. Tech Backbone of India’s vaccination program [Internet]. National Health Authority; 2021 [cited 2022 Mar 29]. Available from: https://nha.gov.in/img/resources/CoWIN-Final-Vikas-Sheel.pdf.
- 49. Ministry of Health and Family Welfare. "Har Ghar Dastak” vaccination campaign [Internet]. New Delhi: Press Information Bureau; 2021 [cited 2022 Mar 29]. Available from: https://www.pib.gov.in/PressReleaseIframePage.aspx?PRID=1767056.
- 50. Central Pollution Control Board (CPCB). Bio-medical waste rules [Internet]. CPCB; 2017 [cited 2022 Mar 29]. Available from: https://cpcb.nic.in/bio-medical-waste-rules/.
- 51. Central Pollution Control Board (CPCB). Technical guidelines [Internet]. CPCB; 2022 [cited 2022 Mar 29]. Available from: https://cpcb.nic.in/technical-guidelines-3/.
- 52. Centers for Disease Control and Prevention (CDC). Identifying, disposing, and reporting COVID-19 vaccine wastage [Internet]. Atlanta: CDC; 2022 [cited 2022 Mar 29]. Available from: https://www.cdc.gov/vaccines/covid-19/hcp/wastage-operational-summary.html.
- 53. Goswami S. Those with special needs to get dedicated vaccination centres. Hindustan Times [Internet]. 2022 [cited 2022 Mar 29]. Available from: https://www.hindustantimes.com/cities/others/delhi-govt-orders-dedicated-vaccination-centres-for-differently-abled-in-each-zone-101622745673259.html.
- 54. Ministry of Health and Family Welfare. SOPs on COVID-19 vaccination of persons without prescribed identity cards through CoWIN [Internet]. Delhi: Ministry of Health and Family Welfare, Government of India; 2021 [cited 2022 Mar 29]. Available from: https://www.mohfw.gov.in/pdf/SOPforCOVID19VaccinationofPersonswithoutPrescribedIdentityCards.pdf.
- 55. World Health Organization (WHO). WHO Director: general announces Global Health Leaders Awards [Internet]. Geneva: WHO; 2022 [cited 2022 Mar 29]. Available from: https://www.who.int/news/item/22-05-2022-who-director-general-announces-global-health-leaders-awards.
- 56. Nadimuthu LPR, Victor K. Environmental friendly micro cold storage for last-mile COVID-19 vaccine logistics. Environ Sci Pollut Res Int 2022;29:23767−78.ArticlePubMedPDF
- 57. Kumar VM, Pandi-Perumal SR, Trakht I, et al. Strategy for COVID-19 vaccination in India: the country with the second highest population and number of cases. NPJ Vaccines 2021;6:60. ArticlePubMedPMCPDF
References
Figure & Data
References
Citations

- Digital health technology used in emergency large-scale vaccination campaigns in low- and middle-income countries: a narrative review for improved pandemic preparedness
Paula Mc Kenna, Lindsay A. Broadfield, Annik Willems, Serge Masyn, Theresa Pattery, Ruxandra Draghia-Akli
Expert Review of Vaccines.2023; 22(1): 243. CrossRef - Media Reporting Relating to COVID-19 Vaccination as a Driver of Vaccine Hesitancy Prior to the Second Wave of the COVID-19 Pandemic in India: A Content Analysis of Newspaper and Digital Media Reports
Saurav Basu, Himanshi Sharma
Cureus.2023;[Epub] CrossRef - An assessment of the strategy and status of COVID-19 vaccination in India
Sneh Lata Gupta, Surbhi Goswami, Ananya Anand, Namrata Naman, Priya Kumari, Priyanka Sharma, Rishi K. Jaiswal
Immunologic Research.2023; 71(4): 565. CrossRef - Development of a Choice-framework for Covid vaccines in India using a multi-criteria decision analysis approach
Tarun K. George, Nayana P. Nair, Awnish Kumar Singh, A. Dilesh Kumar, Arup Deb Roy, Varshini Neethi Mohan, Gagandeep Kang
Vaccine.2023; 41(25): 3755. CrossRef - COVID-19 Booster Dose Coverage and Hesitancy among Older Adults in an Urban Slum and Resettlement Colony in Delhi, India
Nandini Sharma, Saurav Basu, Heena Lalwani, Shivani Rao, Mansi Malik, Sandeep Garg, Rahul Shrivastava, Mongjam Meghachandra Singh
Vaccines.2023; 11(7): 1177. CrossRef - Review of the unmet medical need for vaccination in adults with immunocompromising conditions: An Indian perspective
Ashok Vaid, Neha Rastogi, T. Mark Doherty, Peter San Martin, Yashpal Chugh
Human Vaccines & Immunotherapeutics.2023;[Epub] CrossRef - Translating the COVID-19 experience in widening the HPV vaccination campaign for cervical cancer in India
Aruni Ghose, Anisha Agarwal, Bhawna Sirohi, Shona Nag, Linus Chuang, Swarupa Mitra
Gynecologic Oncology Reports.2023; 48: 101247. CrossRef - Symptomatic prevalence of covid-19 in vaccinated and non-vaccinated population
Jay Bhupesh Pandya, Nirali Milind Shethia, Divya Bangera, Shailaja Gada Saxena
IP International Journal of Medical Microbiology a.2023; 9(2): 110. CrossRef - Active surveillance of adverse events following COVID-19 vaccines in a tertiary care hospital
Naveena Mary Cherian, Dravya Anna Durai, Muhammed Jaisel, Divyansh Sharma, Juny Sebastian, Chetak Kadabasal Basavaraja, Merrin Mathew
Therapeutic Advances in Vaccines and Immunotherapy.2023;[Epub] CrossRef - Effectiveness of ayurvedic formulation, NAOQ19 along with standard care in the treatment of mild-moderate COVID-19 patients: A double blind, randomized, placebo-controlled, multicentric trial
Pankaj Bhardwaj, Kalaiselvan Ganapathy, Monika Pathania, K.H. Naveen, Jaykaran Charan, Siddhartha Dutta, Ravisekhar Gadepalli, Srikanth Srinivasan, Manoj Kumar Gupta, Akhil D. Goel, Naresh Midha, Bharat Kumar, Meenakshi Sharma, Praveen Sharma, Mithu Baner
Journal of Ayurveda and Integrative Medicine.2023; 14(6): 100778. CrossRef - Balancing Routine and Pandemic: The Synergy of India’s Universal Immunization Program and COVID-19 Vaccination Program
Pawan Kumar, Ashish Birendra Chakraborty, Suhas Dhandore, Pritu Dhalaria, Ajeet Kumar Singh, Disha Agarwal, Kapil Singh, Pretty Priyadarshini, Paras Jain, Vidushi Bahl, Gunjan Taneja
Vaccines.2023; 11(12): 1776. CrossRef - Unveiling vaccine safety: a narrative review of pharmacovigilance in India's COVID-19 vaccination
Megha Hegde, Saurav Raj, Dhananjay Tikadar, Sanatkumar B Nyamagoud
Monaldi Archives for Chest Disease.2023;[Epub] CrossRef



 Cite
Cite