Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 14(2); 2023 > Article
-
Original Article
Estimated impact of the national hepatitis B immunization program on acute viral hepatitis B among adolescents in Republic of Korea -
Chungman Chae
 , Sangwoo Tak
, Sangwoo Tak
-
Osong Public Health and Research Perspectives 2023;14(2):138-145.
DOI: https://doi.org/10.24171/j.phrp.2022.0321
Published online: March 24, 2023
Division of Risk Assessment, Bureau of Public Health Emergency Preparedness, Korea Disease Control and Prevention Agency, Cheongju, Republic of Korea
- Corresponding author: Chungman Chae Division of Risk Assessment, Bureau of Public Health Emergency Preparedness, Korea Disease Control and Prevention Agency, 187 Osongsaengmyeong 2-ro, Osong-eup, Heungdeok-gu, Cheongju 28159, Republic of Korea E-mail: cmchae@korea.kr
© 2023 Korea Disease Control and Prevention Agency.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
- 1,469 Views
- 61 Download
Abstract
-
Objectives
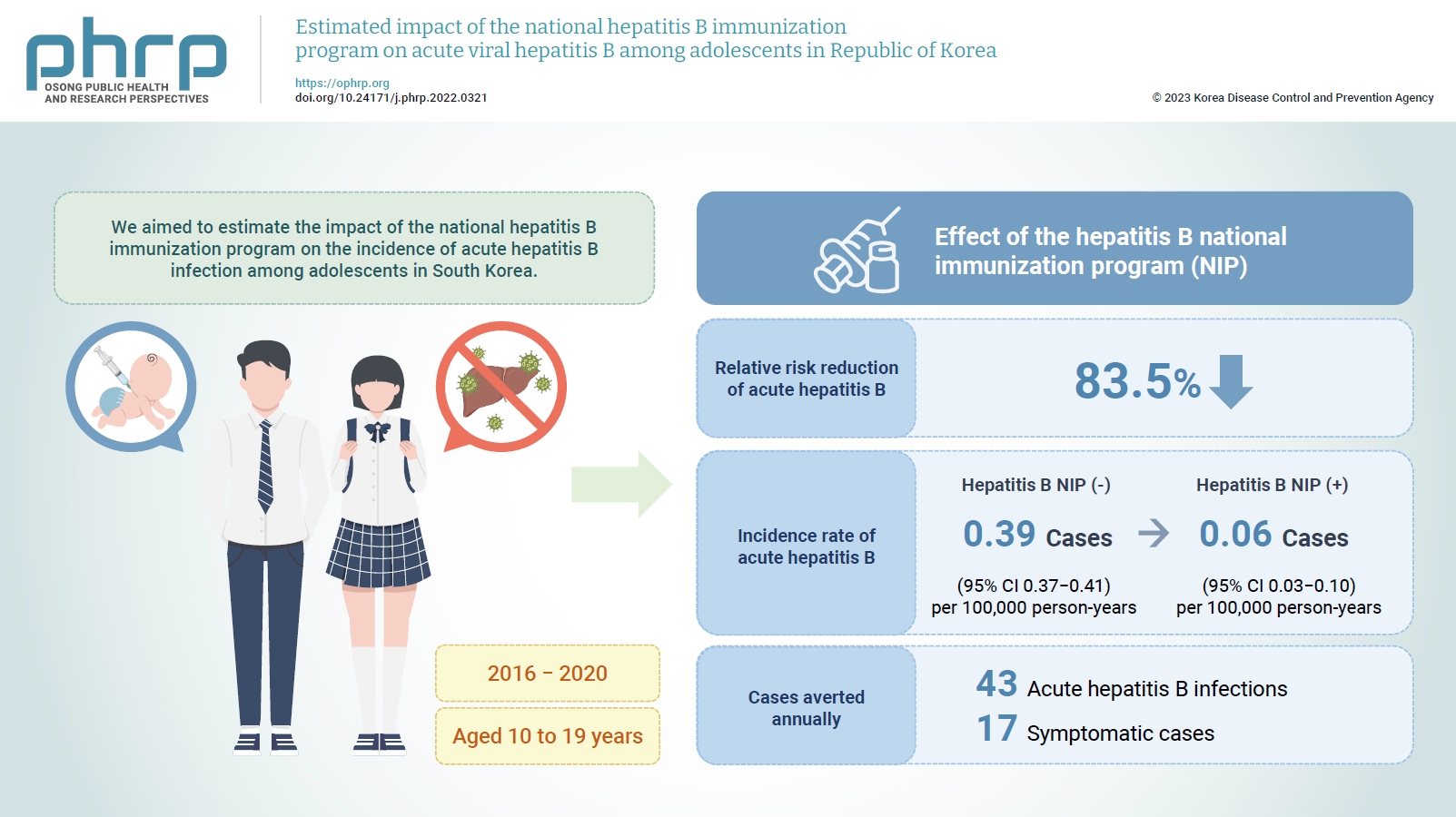
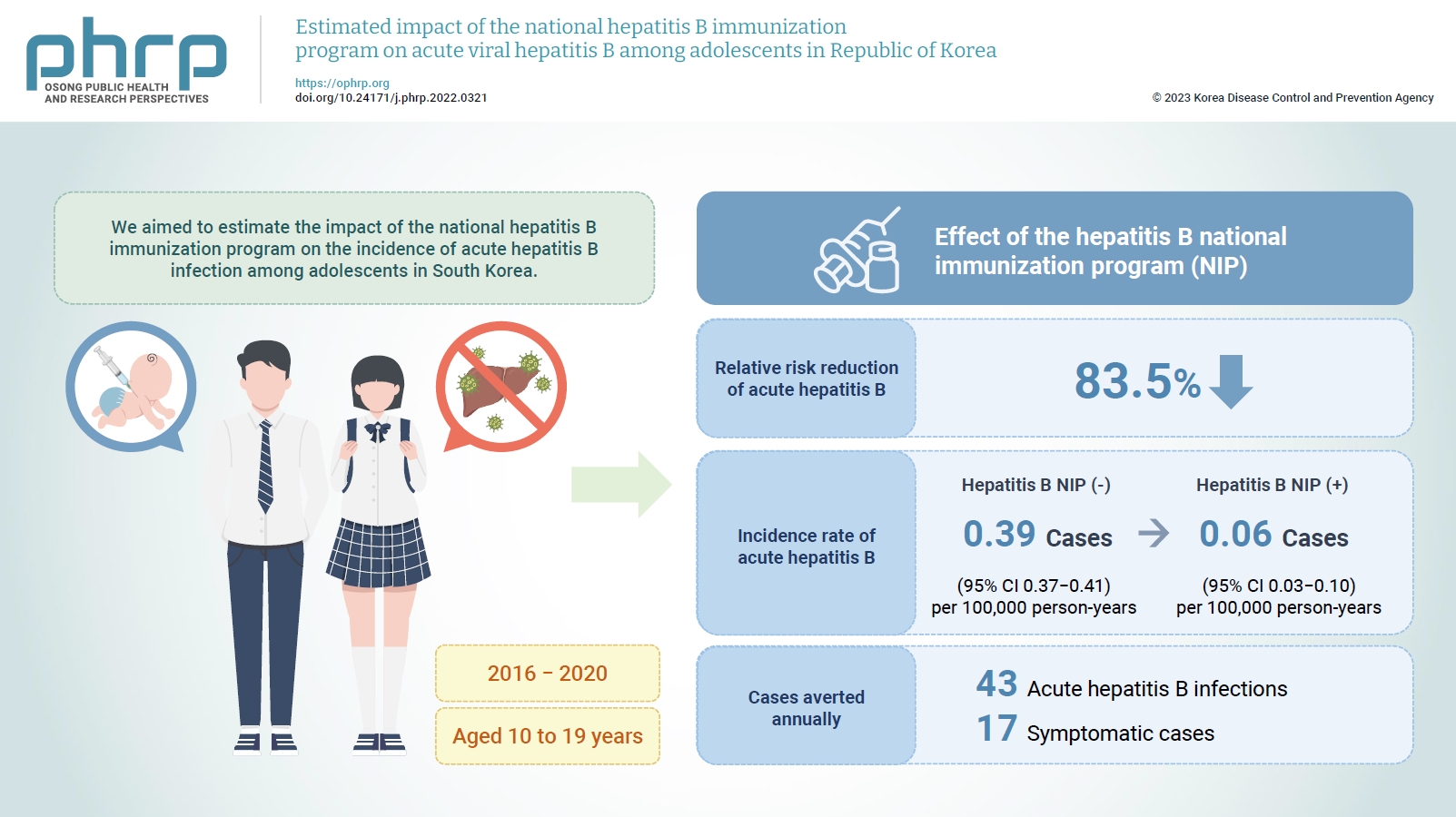
- We aimed to estimate the impact of the national hepatitis B immunization program on the incidence of acute hepatitis B infection among adolescents in South Korea.
-
Methods
- We estimated the counterfactual incidence rate of reported acute hepatitis B among adolescents from 2016 to 2020 compared to the assumption that the national hepatitis B immunization program for children had not been implemented since 1995. The impact of the national hepatitis B immunization program for adolescents was measured by estimating the absolute risk reduction and averted acute hepatitis B infections among adolescents from 2016 to 2020 attributed to the national immunization program.
-
Results
- The relative risk reduction of acute hepatitis B among adolescents was estimated to be 83.5% after implementing the national hepatitis B immunization program. The incidence rate of reported acute hepatitis B infections among adolescents decreased from 0.39 to 0.06 per 100,000 person-years, and 43 acute hepatitis B infections, including 17 symptomatic cases, were averted annually from 2016 to 2020 by the national hepatitis B immunization program.
-
Conclusion
- The national hepatitis B immunization program for children was effective in preventing acute hepatitis B infection among adolescents in South Korea.
- Globally, 296 million people were living with chronic hepatitis B infection in 2019, with 2.5 million new infections every year [1]. In 2016, the member states of the World Health Organization committed to eliminating viral hepatitis as a major public health threat by 2030. The World Health Organization established a global health sector strategy on viral hepatitis and set global targets of achieving a 90% reduction in new chronic viral hepatitis B and C infections and a 65% reduction in deaths because of viral hepatitis B and C infections [2].
- In South Korea, hepatitis B is the main cause of chronic liver disease, accounting for 60% to 70% of all cases of chronic liver disease [3]. The hepatitis B surface antigen (HBsAg) positivity rates were 2.7% among people over 20 years and 0.2% among adolescents aged 10 to 18 years in 2020 [4]. The hepatitis B surveillance system was initially operated as a sentinel monitoring system starting in 2000, and it was changed to a mandatory surveillance system in 2010 [5]. The focus of surveillance was limited to acute hepatitis B infections in January 2016 [6]. The national immunization program (NIP) for hepatitis B in infants was introduced in South Korea in 1995, and coverage of the 3 doses of hepatitis B vaccination among newborns increased from 82% in 1998 to 98% in 2018 [3,7]. According to a previous study, hepatitis B vaccination coverage was 37% among adults in 1994, although coverage in more recent years has not been determined [8].
- Countries with low HBsAg positivity rates are likely to have horizontal transmission as the major mode of infection transmission, and data from the acute hepatitis B surveillance system indicate that around 400 cases of horizontally transmitted acute hepatitis B have occurred annually in South Korea [5,9]. The impact of vaccination on horizontal transmission as well as vertical transmission should be evaluated to estimate the impact of the hepatitis B NIP correctly. However, most studies in South Korea have investigated the impact of the hepatitis B NIP on vertical transmission based on the HBsAg positivity rate, and the impact of the hepatitis B NIP on horizontal transmission based on acute hepatitis B surveillance data has not yet been evaluated [9,10]. Hence, the aim of this study was to estimate the impact of the hepatitis B NIP on the incidence of acute hepatitis B infection among adolescents by estimating the absolute risk reduction (ARR) in South Korea from 2016 to 2020, with a focus on horizontal transmission.
Introduction
- Descriptive Analysis
- We conducted a descriptive analysis of acute hepatitis B cases reported from 2016 to 2020 and examined the distribution of cases by age group. Acute hepatitis B cases reported to the Korea Disease Control and Prevention Agency (KDCA) from January 2016 to December 2020 were collected from the integrated public healthcare information system. National population data were collected from the Korean Statistical Information Service [11]. The incidence rate (IR) per 100,000 person-years was estimated using the cumulative number of reported acute hepatitis B cases and person-years by age group for each year from 2016 to 2020.
- Population
- Members of the population aged 10 to 19 years and those aged 20 years and above in each year from 2016 to 2020 were defined as adolescents and adults, respectively. We did not define adolescents and adults based on birth cohorts in a specific year, because older adolescents drop out of the adolescent cohort as they become adults in later years, and the adolescent cohort is not affected by the different prevalence of risk exposures among adults, including the increased prevalence of sexual contacts and illicit drug use [12−14]. We conducted a sensitivity analysis to account for the effect of the hepatitis B NIP on the population that was defined as adults but born after the implementation of the hepatitis B NIP in each year from 2016 to 2020.
- Study Design
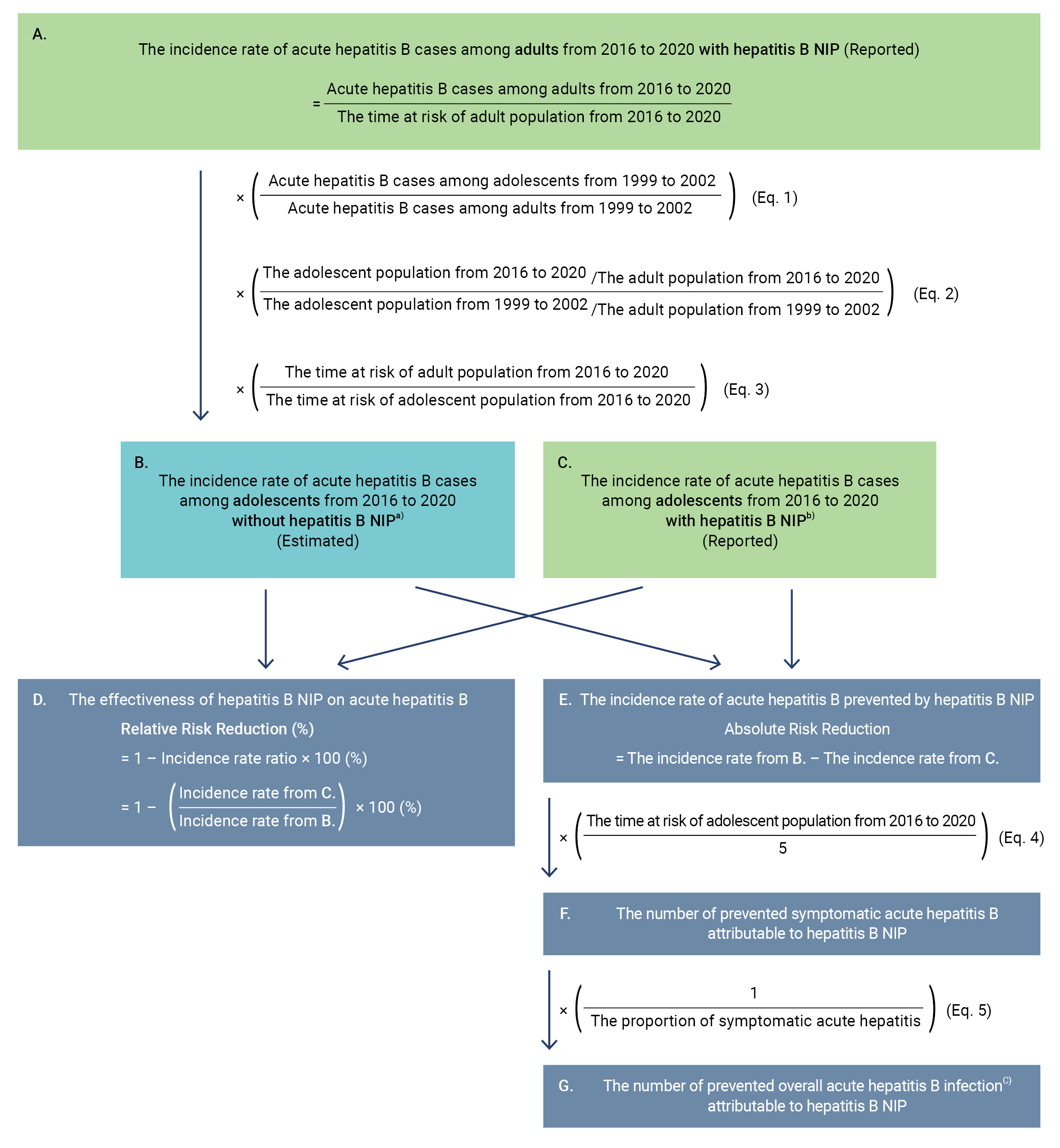
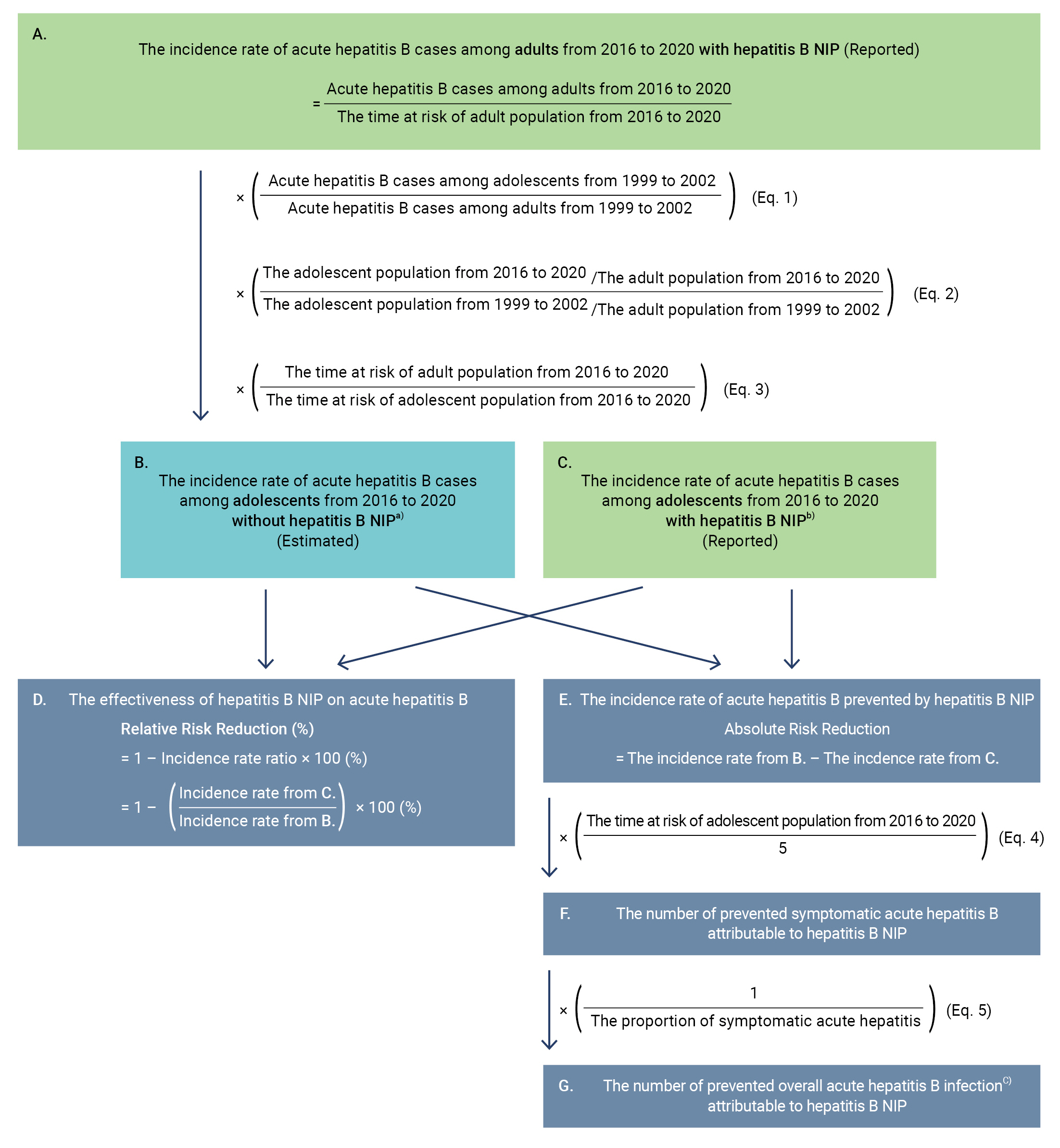
- We estimated the relative risk reduction (RRR) and the ARR of the hepatitis B NIP by comparing the reported IR of acute hepatitis B among adolescents from 2016 to 2020 (status with the hepatitis B NIP) with the estimated IR assuming that the NIP had not been implemented (status without the hepatitis B NIP). To estimate the IR among adolescents from 2016 to 2020 without the hepatitis B NIP, we used the ratio of adolescents to adults among acute hepatitis B patients in a previous study conducted by Yim et al. [15]. That study investigated acute hepatitis B patients at 3 tertiary general hospitals from February 1999 to February 2002.
- We assumed that the ratio of adults to adolescents among acute hepatitis B patients reported from 2016 to 2020 without the hepatitis B NIP would be the same as the ratio from 1999 to 2002 if the population ratios in the 2 periods were identical. The number of reported acute hepatitis B cases among adults from 2016 to 2020 was multiplied by the ratio of adolescents to adults among acute hepatitis B cases from the previous study (Figure 1A, Eq. 1). Since the ratio of adolescents to adults changed from 1999 to 2020, the average ratio of adolescents to adults from 2016 to 2020 was divided by the average ratio of that from 1999 to 2002, and the result was multiplied by the previously estimated number (Figure 1, Eq. 2). We conducted a sensitivity analysis to account for the change in the ratio of adolescents to adults among acute hepatitis B patients. The denominator for calculating the IR was changed from the time at risk of the adult population to the time at risk of the adolescent population (Figure 1, Eq. 3).
- We assumed that the trends in hepatitis B vaccination coverage among adults subject to the hepatitis B NIP would be the same as those of hepatitis B vaccination coverage among the overall population not subject to the hepatitis B NIP during the overall study period. We divided the estimated IR of acute hepatitis B among adolescents without the hepatitis B NIP from 2016 to 2020 (Figure 1B) by the reported IR with the hepatitis B NIP (Figure 1C) to estimate the incidence rate ratio (IRR), and we subtracted the IRR from 1 to estimate the RRR attributed to the hepatitis B NIP (Figure 1D).
- We estimated the ARR of acute hepatitis B by subtracting the reported IR of acute hepatitis B among adolescents from 2016 to 2020 with the hepatitis B NIP from the estimated IR without the hepatitis B NIP (Figure 1E). Since clinical symptoms and laboratory confirmation are essential for reporting acute hepatitis B, we assumed that all reported acute hepatitis B cases were symptomatic [5]. We multiplied the ARR by the average annual time at risk of the adolescent population from 2016 to 2020 to estimate the annual reduction of symptomatic acute hepatitis B cases from 2016 to 2020 (Figure 1F, Eq. 4). We also multiplied the reduction of symptomatic cases by the reciprocal proportion of symptomatic cases among all acute hepatitis B infections to estimate the overall reduction of acute hepatitis B infection, including symptomatic and asymptomatic cases (Figure 1G Eq. 5) [16].
- Parameters
- The ratio of adolescents to adults among acute hepatitis B cases at 3 tertiary hospitals from 1999 to 2002 was 0.10 (95% confidence interval [CI], 0.02–0.21) [15]. The average ratio of the adolescent population to the adult population from 2016 to 2020 (0.13) was 0.61 times the average ratio of adolescents to adults from 1999 to 2002 (0.20). The average adolescent population from 2016 to 2020 was 5,214,595, which was equal to one-eighth of the adult population [11]. According to the estimate by Klevens et al. [16], 39.5% of overall acute hepatitis B infections were symptomatic (Table 1) [11,15,16].
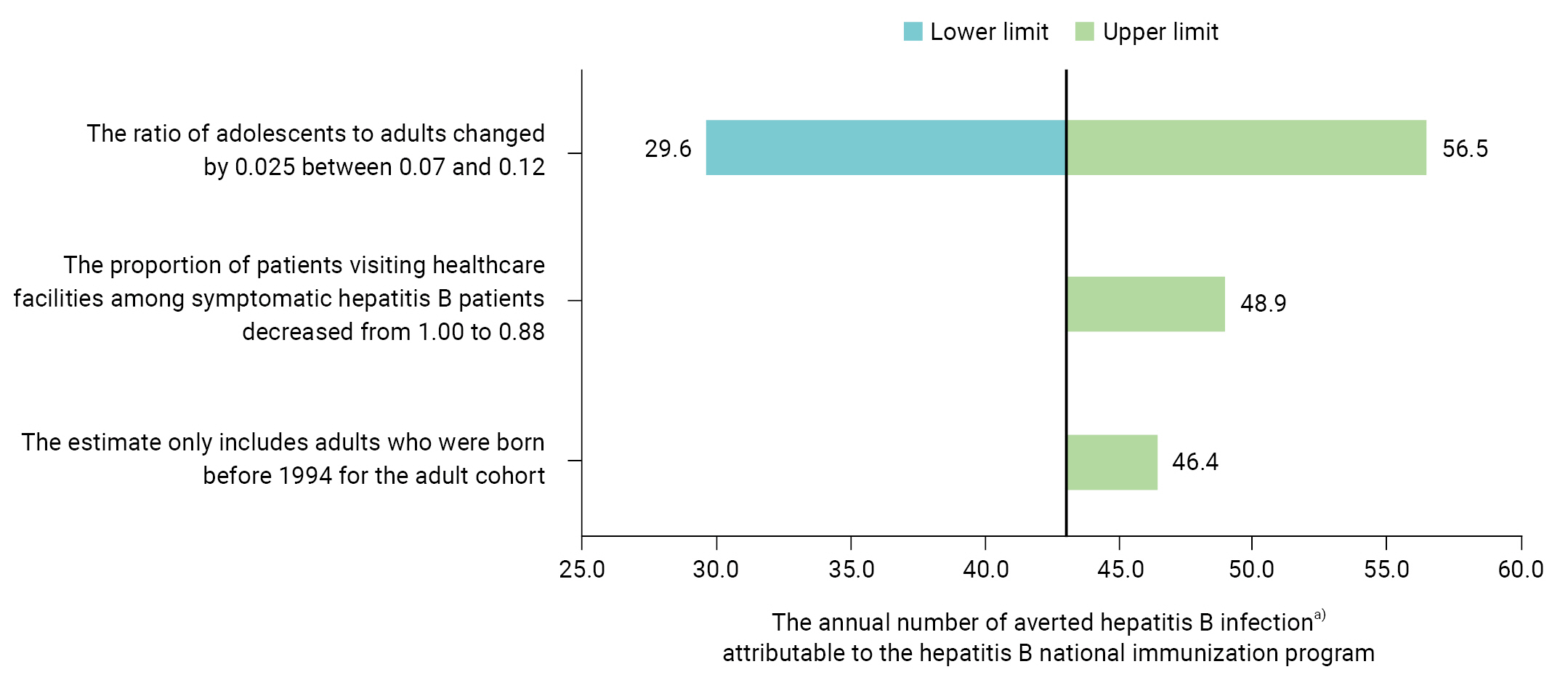
- Sensitivity Analysis
- We conducted a 1-way deterministic sensitivity analysis to investigate the uncertainty originating from each parameter, and the results were presented in a tornado diagram to show the effect of variation in parameters on the outcome. We assumed that the ratio of adolescents to adults among patients was 0.10 without the hepatitis B NIP, using the same ratio of adolescents to adults as that from 1999 to 2002. However, the ratio of adolescents to adults was 0.12 (95% CI, 0.07–0.19) in a previous study investigating 185 acute hepatitis B patients from 1982 to 1986 [17]. The ratio decreased by 0.025 during approximately 15 years. The difference in the average ratios of adolescents to adults from 1982 to 1986 and from 1999 to 2002 was similar to the difference in the average ratios from 1999 to 2002 and from 2016 to 2020. Therefore, we conducted a sensitivity analysis to investigate how the outcomes changed when the ratio of adolescents to adults changed by 0.025.
- There could have been uncaptured symptomatic acute hepatitis B cases in individuals who did not visit healthcare facilities. Klevens et al. [16] estimated that 88% of symptomatic hepatitis B patients visited healthcare facilities in the United States. Since most South Koreans (97%) are covered by the National Health Insurance Service, the proportion of symptomatic hepatitis B patients who visited healthcare facilities would likely be higher in South Korea [18]. Therefore, we investigated how the study outcomes changed when the proportion of symptomatic individuals visiting healthcare facilities changed from 88% to 100%.
- Since the hepatitis B NIP was implemented in 1995, young adults from 2016 to 2020 would have been covered by the hepatitis B NIP. The time at risk of adults born after 1995 accounted for 6.5% of the overall observed time at risk of the adult cohort during the study period. Therefore, we conducted a sensitivity analysis to explore the impact of excluding adults who were born after 1995 from the adult cohort. We estimated the IR among adults born before 1994 under the assumption that the IR among adults born after 1995 was the same as the IR among the adolescent population.
- Statistical Analysis
- All statistical analyses were performed using R Statistical Software ver. 4.1.2 (R Foundation for Statistical Computing) and the “epiR” R package ver. 2.0.41, and the exact method based on the Poisson distribution was used to present CIs for the IRs. Wald CIs were presented for the RRR and the ARR.
- Ethical Statement
- The KDCA Institutional Review Board (IRB No: 2022-08-06-PE-A) determined that this study was exempt from ethics approval and informed consent because we used data without personal identifiers that were collected during legally mandated public health investigations under the authority of the Infectious Diseases Control and Prevention Act (No: 12444; No: 13392; No: 17067; No: 17642).
Materials and Methods
- Descriptive Analysis
- In total, 1,741 acute hepatitis B cases were reported from 2016 to 2020. The overall IR was 0.68 (95% CI, 0.65–0.71) per 100,000 person-years. The IR among adolescents was significantly lower than the IR among adults. The IRs per 100,000 person-years were 0.06 (95% CI, 0.03–0.10) among adolescents and 0.83 (95% CI, 0.79–0.87) among adults. The cumulative number of reported acute hepatitis B cases among adolescents was only 17, while the cumulative number of reported acute hepatitis B cases among adults aged over 20 years was 1,719 from 2016 to 2020 (Table 2).
- Impact of the Hepatitis B NIP
- The IR of acute hepatitis B cases among adolescents from 2016 to 2020 without the hepatitis B NIP was estimated as 0.39 (95% CI, 0.37–0.41) cases per 100,000 person-years. The IR of acute hepatitis B among adolescents from 2016 to 2020 with the hepatitis B NIP was 0.06 (95% CI, 0.03–0.10) cases per 100,000 person-years. The RRR of acute hepatitis B attributed to the hepatitis B NIP was 83.5% (95% CI, 72.2–90.8) and the ARR was 0.33 (95% CI, 0.24–0.41) cases per 100,000 person-years. The annual number of averted hepatitis B infections among adolescents attributable to the NIP from 2016 to 2020 was 43.0 cases (95% CI, 32.2–53.9), including 17.0 (95% CI, 12.7–21.3) symptomatic cases (Table 3).
- Sensitivity Analysis
- If the ratio of adolescents to adults was 0.07, the estimated RRR was 77.7%, and the ARR per 100,000 person-years was 0.22. The number of overall averted acute hepatitis B infections was 30 cases including 12 symptomatic cases annually. In contrast, if the ratio of adolescents to adults was 0.12, the estimated RRR was 86.9% and the ARR per 100,000 person-years was 0.43. The overall number of averted acute hepatitis B infections increased to 56 cases, including 22 symptomatic cases every year. If the proportion of patients visiting healthcare facilities among symptomatic hepatitis B patients decreased from 100% to 88%, the yearly number of averted overall acute hepatitis B infections increased to 49 cases, including 19 symptomatic cases. If the IR of acute hepatitis B among adults born after 1995 was the same as the IR among adolescents, the estimated RRR was 84.5% and the ARR was 0.35, and the annual number of averted overall hepatitis B infections was raised to 46, including 18 symptomatic cases (Figure 2).
Results
- We found that the current IR of acute hepatitis B among adolescents is dramatically lower than that among adults in South Korea. The hepatitis B NIP for children appears to be an effective measure to prevent acute hepatitis B infections in adolescents. Our estimates suggest that approximately 83.5% of acute hepatitis B cases have been prevented by the hepatitis B NIP in South Korea, averting more than 40 cases of acute hepatitis B infection annually among adolescents. To the best of our knowledge, this is the first study to investigate the impact of the hepatitis B NIP in children on the incidence of acute hepatitis B in adolescents in South Korea.
- We did not use an observational cohort design that would directly compare the IR between adults and adolescents because the risk exposure frequency among adolescents could be different from that of adults. Additionally, we did not compare different age cohorts in the same period or the same age cohort in different periods to estimate the effectiveness of the hepatitis B NIP. This is because hepatitis B surveillance focusing on acute hepatitis B infections was implemented in 2016 and has only been in operation for a limited period. Furthermore, the annual incidence of acute hepatitis B cases in adolescents is too small (fewer than 4 cases) to be divided into sub-cohorts.
- We estimated the effectiveness of the hepatitis B NIP in South Korea under specific circumstances, rather than the effectiveness of the hepatitis B vaccination program in general. This is because we were unable to identify parameters such as coverage of the hepatitis B NIP in each age group, even though the annual coverage of the hepatitis B NIP gradually increased from 90% in the early 2000s to 98% in 2019 [7]. Therefore, the estimated effectiveness of the hepatitis B NIP in South Korea cannot be directly compared to the effectiveness of hepatitis B vaccination programs in other countries.
- The coverage of hepatitis B vaccination among adults in South Korea in recent years is unknown. However, the outcomes of our study already account for the effect of vaccination coverage among adults if the vaccination coverage among adults was the same as the coverage among the overall population without the hepatitis B NIP. This is because the estimated IR in the adolescent population (Figure 1B) was derived from the IR in the adult population (Figure 1A). However, even if the hepatitis B NIP had not been implemented, other vaccination programs for children may have raised awareness and coverage of the hepatitis B vaccine, especially among children. Therefore, the impact of the hepatitis B NIP implementation could have been smaller than the estimate in this study.
- Several social, behavioral, and environmental changes can lead to changes in the risk pattern and incidence of hepatitis B infections. For example, the reuse of syringes was prohibited by law in 2016, and hepatitis B virus screening tests for transfusions have improved over the years [19,20]. However, the estimated RRR in this study was minimally affected by these changes when the risk of exposure to hepatitis B infection changed evenly among adolescents and adults. This is because both the estimated IR among adolescents without the hepatitis B NIP (Figure 1B) and the reported IR among adolescents with the hepatitis NIP (Figure 1C) were affected by these changes. However, these changes could affect the ARR and the number of averted cases by changing the scale of the IRs.
- Changes in the frequency of risk exposure to hepatitis B infection in specific age cohorts could affect the RRR and ARR. For example, the HBsAg positivity rate among the population aged over 20 years decreased from 5.0% in 1998 to 2.7% in 2020, and the number of acute hepatitis B cases among adults could have been reduced by the decrease in positivity rate. Moreover, the introduction of oral antiviral therapy and positive externalities of the hepatitis B NIP, such as herd immunity, also could have reduced the incidence of acute hepatitis B among adults. The reduced incidence of acute hepatitis B among adults could have decreased the estimated IR among adolescents without the hepatitis B NIP (Figure 1B), as well as the estimated RRR (Figure 1D) and ARR (Figure 1E). Considering the positive externalities of the hepatitis B NIP to the adult population, our estimates of the RRR and ARR could have been underestimated.
- Furthermore, the proportion of asymptomatic hepatitis B cases is generally higher among people who are infected at a younger age [21]. The estimated IR among adolescents without hepatitis B NIP (Figure 1B) could be overestimated compared with the reported IR among adolescents with hepatitis B NIP (Figure 1C) because the estimated IR was based on the reported numbers of symptomatic acute hepatitis B cases among adults, which may have a higher proportion of symptomatic cases than among adolescents. As a result, our estimates of RRR (Figure 1D) and ARR (Figure 1E) could also have been overestimated.
- We estimated the overall protection provided by the hepatitis B NIP using population-level data, which cannot be directly compared to the effectiveness of hepatitis B vaccination programs in other countries. Therefore, it is necessary to conduct further studies that measure direct and indirect protection using individual-level infection records and vaccination histories. Moreover, the trends of risk factors for hepatitis B infection among adolescents, including sexual behavior, tattooing, and use of improperly sanitized equipment for cosmetic procedures, require more investigation. Given the substantial public health burden posed by hepatitis B infection, in-depth studies focusing on risk factors and the impact of exposure to these factors on the incidence of acute hepatitis B infection among adolescents should be conducted.
Discussion
- In many countries, acute hepatitis B infections have been consistently caused by horizontal transmission of the hepatitis B virus. However, the focus of most hepatitis B vaccination programs has been on preventing mother-to-child transmission. Our findings highlighted that the hepatitis B NIP for children, which is known to be effective in preventing mother-to-child transmission, has also been effective in preventing acute hepatitis B infections in adolescents. However, our study estimated the overall protection provided by hepatitis B NIP, and the trends of risk factors for hepatitis B infection among adolescents have not been fully investigated. Therefore, it is necessary to conduct further studies that measure the direct and indirect protection provided by the hepatitis B NIP, as well as studies focusing on risk factors for hepatitis B infection and its impact on the incidence of acute hepatitis B infection among adolescents.
Conclusion
- The hepatitis B national immunization program (NIP) for children was effective in preventing acute hepatitis B infection among adolescents in South Korea.
- The relative risk reduction of acute hepatitis B among adolescents was estimated to be 83.5% after implementing the hepatitis B NIP.
- From 2016 to 2020, 43 acute hepatitis B infections including 17 symptomatic cases were estimated to be averted annually attributed to the hepatitis B NIP.
HIGHLIGHTS
-
Ethics Approval
The KDCA Institutional Review Board (IRB No: 2022-08-06-PE-A) determined that this study was exempt from ethics approval and informed consent because we used data without personal identifiers that were collected during legally mandated public health investigations under the authority of the Infectious Diseases Control and Prevention Act (No: 12444; No: 13392; No: 17067; No: 17642).
-
Conflicts of Interest
The authors have no conflicts of interest to declare.
-
Funding
None.
-
Availability of Data
The datasets are not publicly available but are available from the corresponding author upon reasonable request.
Article information
-
Acknowledgements
- National acute hepatitis B cases reported to the KDCA collected from the integrated public healthcare information system were used for this analysis. The views expressed here are those of the authors, and not necessarily those of the KDCA.

| Description | Value | Reference |
|---|---|---|
| The ratio of adolescents to adults among acute hepatitis B cases from 1999 to 2002 (95% confidence interval) | 0.10 (0.02–0.21) | [15] |
| The average ratio of the adolescent population to the adult population from 2016 to 2020 divided by the ratio of that from 1999 to 2002 | 0.61 | [11] |
| The average ratio of the adult population to the adolescent population from 2016 to 2020 | 8.00 | [11] |
| The average size of the adolescent population from 2016 to 2020 | 5,214,595 | [11] |
| The proportion of symptomatic acute hepatitis among overall hepatitis B infections | 0.395 | [16] |
| Age group (y) | No. of cases among males | No. of cases among females | Total | Time at risk (person-year) | Incidence rate (95% CI)a) | |
|---|---|---|---|---|---|---|
| 0–9 | 2 | 3 | 5 | 21,744,242 | 0.02 (0.01–0.05) | |
| 10–19 | 11 | 6 | 17 | 26,972,974 | 0.06 (0.03–0.10) | |
| 20–39 | 392 | 203 | 595 | 70,008,079 | 0.84 (0.77– 0.91) | 0.83 (0.79–0.87)b) |
| 40–59 | 541 | 228 | 769 | 84,492,096 | 0.91 (0.84–0.97) | |
| ≥60 | 188 | 167 | 355 | 54,013,848 | 0.68 (0.61–0.75) | |
| Overall | 1,134 | 607 | 1,741 | 256,331,238 | 0.68 (0.65–0.71) | |
| Description | Estimated value (95% CI) |
|---|---|
| The incidence ratea) of acute hepatitis B cases among adolescents from 2016 to 2020 without the hepatitis B NIPb) | 0.39 (0.37–0.41) |
| The relative risk reduction (%) attributed to the hepatitis B NIP on acute hepatitis B infection | 83.5 (72.2–90.8) |
| The absolute risk reductiona) attributed to the hepatitis B NIP | 0.33 (0.24–0.41) |
| The annual number of prevented symptomatic acute hepatitis B cases attributable to the hepatitis B NIP from 2016 to 2020 | 17.0 (12.7–21.3) |
| The annual number of prevented overall hepatitis B infectionsc) attributed to the hepatitis B NIP from 2016 to 2020 | 43.0 (32.2–53.9) |
- 1. World Health Organization (WHO). Global progress report on HIV, viral hepatitis and sexually transmitted infections, 2021: accountability for the global health sector strategies 2016-2021: actions for impact: web annex 2: data methods [Internet]. WHO; 2021 [cited 2022 May 30] Available from: https://apps.who.int/iris/handle/10665/342813.
- 2. World Health Organization (WHO). Global health sector strategy on viral hepatitis 2016-2021. Towards ending viral hepatitis [Internet]. WHO; 2016 [cited 2022 May 30] Available from: https://apps.who.int/iris/handle/10665/246177.
- 3. Kim DY. History and future of hepatitis B virus control in South Korea. Clin Mol Hepatol 2021;27:620−2.ArticlePubMedPMCPDF
- 4. Korea Disease Control and Prevention Agency (KDCA). Korea Health Statistics 2020: Korea National Health and Nutrition Examination Survey (KNHANES VIII-2) [Internet]. KDCA; 2022 [cited 2022 Jun 9] Available from: https://knhanes.kdca.go.kr/knhanes/sub04/sub04_04_01.do. Korean.
- 5. Korea Disease Control and Prevention Agency (KDCA). Guidelines for vaccine preventable disease management 2022 [Internet]. KDCA; 2022 [cited 2022 Jun 9]. Available from: https://kdca.go.kr/filepath/boardSyview.es?bid=0019&list_no=719032&seq=1. Korean.
- 6. Korea Disease Control and Prevention Agency. Guidelines for infectious disease management program 2022 [Internet]. Korea Disease Control and Prevention Agency; 2022 [cited 2022 Jun 9]. Available from: https://kdca.go.kr/filepath/boardSyview.es?bid=0019&list_no=718118&seq=2. Korean.
- 7. World Health Organization (WHO). Hepatitis B vaccination coverage [Internet]. WHO; 2022 [cited 2022 Jul 17]. Available from: https://immunizationdata.who.int/pages/coverage/hepb.html?CODE=KOR&ANTIGEN=&YEAR=.
- 8. Hur YJ, Choe SA, Choe YJ, et al. Hepatitis B surface antigen and antibody positivity among women of childbearing age after three decades of universal vaccination in South Korea. Int J Infect Dis 2021;104:551−5.ArticlePubMed
- 9. Yim SY, Kim JH. The epidemiology of hepatitis B virus infection in Korea. Korean J Intern Med 2019;34:945−53.ArticlePubMedPMCPDF
- 10. Cho HY, Kim CH, Go UY, et al. Immunization decision-making in the Republic of Korea: the structure and functioning of the Korea Advisory Committee on Immunization Practices. Vaccine 2010;28 Suppl 1:A91−A95.ArticlePubMed
- 11. Statistics Korea. Korean Statistical Information Service: population trend survey [Internet]. Statistics Korea; 2022 [cited 2022 May 30]. Available from: https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B040M5. Korean.
- 12. Statistics Korea. Korean Statistical Information Service: age of the offenders at the time crime [Internet]. Statistics Korea; 2022 [cited 2022 Aug 20]. Available from: https://stat.kosis.kr/statHtml_host/statHtml.do?orgId=132&tblId=DT_13204_4101&dbUser=NSI_IN_132. Korean.
- 13. Park J, Park SH, Lee SJ, et al. Changing trends in sexual debut age in the Korean Internet Sexuality Survey. World J Mens Health 2022;40:465−72.ArticlePubMedPMCPDF
- 14. Kwon SY, Lee CH. Epidemiology and prevention of hepatitis B virus infection. Korean J Hepatol 2011;17:87−95.ArticlePubMedPMC
- 15. Yim HJ, Chang YJ, Byun KS, et al. The changing patterns of acute hepatitis B infection in Korea in the early 2000’s. Korean J Med 2005;69:601−7. Korean.
- 16. Klevens RM, Liu S, Roberts H, et al. Estimating acute viral hepatitis infections from nationally reported cases. Am J Public Health 2014;104:482−7.ArticlePubMedPMC
- 17. Dongarwar D, Salihu HM. Implementation of universal health coverage by South Korea during the COVID-19 pandemic. Lancet Reg Health West Pac 2021;7:100093. ArticlePubMedPMC
- 18. Korea Legislation Research Institute. Medical Service Act: General Provisions. Act No. 18468, Article 4 Paragraph 6 [Internet]. Korea Legislation Research Institute; 2021 [cited 2023 Mar 4]. Available from: https://elaw.klri.re.kr/kor_service/lawView.do?hseq=60889&lang=ENG.
- 19. Yu JM, Suh DJ. The etiology of acute viral hepatitis in Korean. Korean J Med 1987;33:203−10. Korean.
- 20. Kim HO. Current state of blood management services in Korea. Ann Lab Med 2022;42:306−13.ArticlePubMedPMC
- 21. McMahon BJ, Alward WL, Hall DB, et al. Acute hepatitis B virus infection: relation of age to the clinical expression of disease and subsequent development of the carrier state. J Infect Dis 1985;151:599−603.ArticlePubMed
References
Figure & Data
References
Citations



 Cite
Cite