Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 14(3); 2023 > Article
-
Original Article
Risk factors for COVID-19 outbreaks in livestock slaughtering and processing facilities in Republic of Korea -
Seongju Choi1
 , Tae Jong Son1
, Tae Jong Son1 , Yeon-Kyung Lee2
, Yeon-Kyung Lee2
-
Osong Public Health and Research Perspectives 2023;14(3):207-218.
DOI: https://doi.org/10.24171/j.phrp.2023.0035
Published online: June 8, 2023
1Division of Infectious Disease Response, Gyeongbuk Regional Center for Disease Control and Prevention, Korea Disease Control and Prevention Agency, Daegu, Republic of Korea
2Division of Healthcare Associated Infection Control, Bureau of Healthcare Safety and Immunization, Korea Disease Control and Prevention Agency, Cheongju, Republic of Korea
- Corresponding author: Yeon-Kyeng Lee Division of Healthcare Associated Infection Control, Bureau of Healthcare Safety and Immunization, Korea Disease Control and Prevention Agency, 187 Osongsaengmyeong 2-ro, Osong-eup, Heungdeok-gu, Cheongju 28159, Republic of Korea E-mail: yeonkyenglee@korea.kr
- Seongju Choi and Tae Jong Son contributed equally to this study as co-first authors.
© 2023 Korea Disease Control and Prevention Agency.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
- 1,213 Views
- 48 Download
Abstract
-
Objectives
- The goal of this study was to help prevent and control the spread of coronavirus disease 2019 (COVID-19) by identifying transmission routes and risk factors in livestock slaughtering and processing facilities (SPFs) and establishing an optimal intervention strategy for outbreaks.
-
Methods
- This case series study was a demographic analysis of patients with confirmed COVID-19 associated with 5 SPFs in Korea between January and June 2021. Additionally, in a retrospective cohort study, the association between COVID-19 infection and risk factors was analyzed for SPFs at which outbreaks occurred.
-
Results
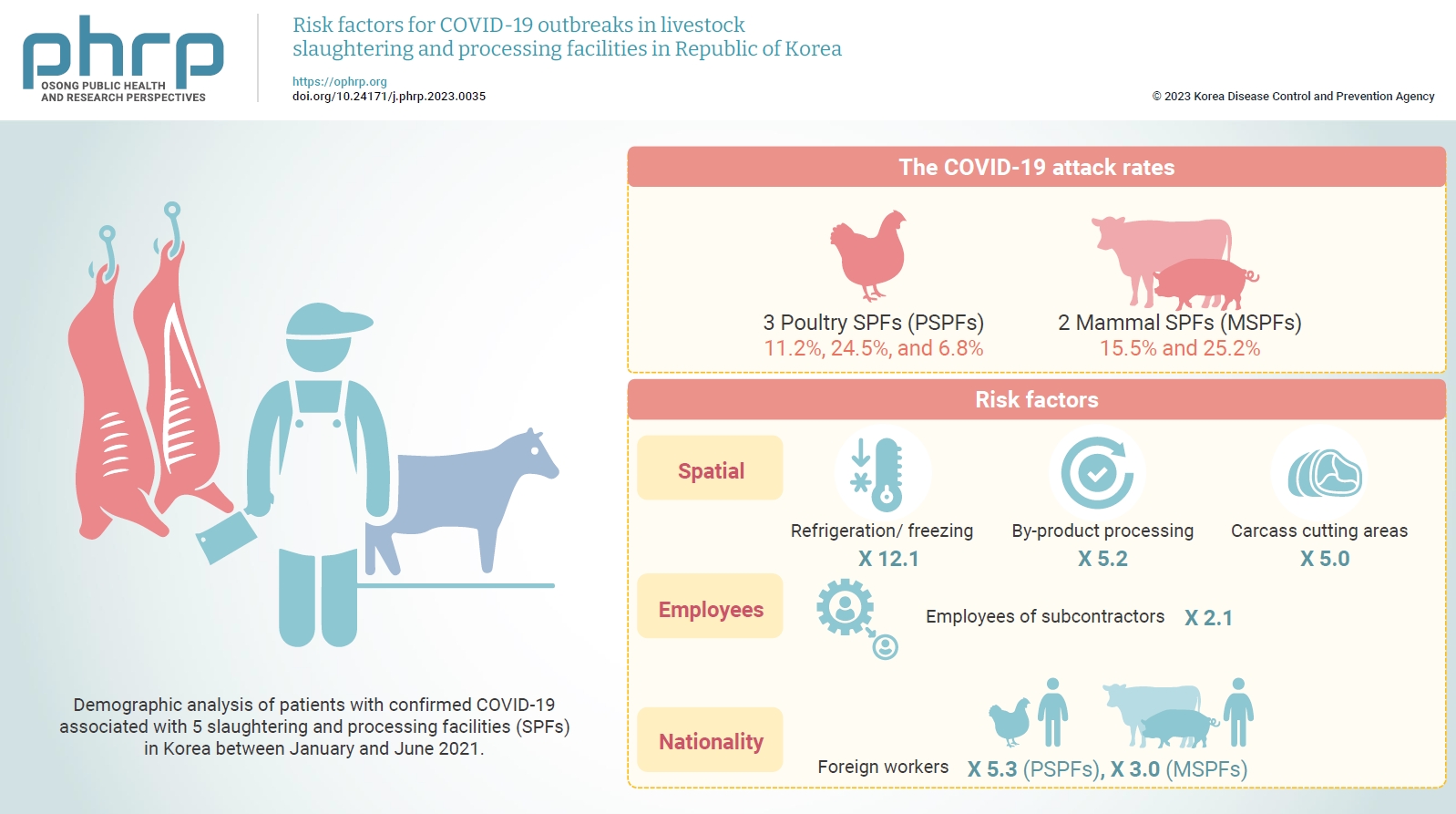
- The COVID-19 attack rates were 11.2%, 24.5%, and 6.8% at 3 poultry SPFs (PSPFs) and 15.5% and 25.2% at 2 mammal SPFs (MSPFs). Regarding spatial risk factors, the COVID-19 risk levels were 12.1-, 5.2-, and 5.0-fold higher in the refrigeration/freezing, by-product processing, and carcass cutting areas, respectively, than in the office area. The risk of COVID-19 infection was 2.1 times higher among employees of subcontractors than among employees of contractors. The COVID-19 risk levels were 5.3- and 3.0-fold higher in foreign workers than in native Korean workers in the PSPFs and MSPFs, respectively.
-
Conclusion
- As the COVID-19 pandemic continues, a detailed policy for infectious disease prevention and control intervention is needed, without interrupting economic activities. Thus, we propose an ideal intervention plan to prevent COVID-19 through disinfection and preemptive testing and to block its transmission through effective contact management during outbreaks at SPFs.
- In late December 2019, the first case of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was confirmed in Wuhan City, Hubei Province, China [1]. Since then, SARS-CoV-2 has spread rapidly throughout Asian countries, such as Japan and Korea, and developed into an international pandemic. The World Health Organization declared a public health emergency and named the disease caused by SARS-CoV-2 coronavirus disease 2019 (COVID-19) [2]. SARS-CoV-2 is transmitted among humans through contact with patients, inhalation of virus-laden droplets, contact with virus-contaminated surfaces, and exposure to aerosols in enclosed spaces [3].
- Identifying the transmission routes, characteristics, and risk factors of the highly contagious SARS-CoV-2 is critical in preventing and controlling its spread. Classifying and managing cluster outbreaks effectively blocks SARS-CoV-2 transmission and prevents infection. Accordingly, it is crucial to understand the transmission route and epidemiological characteristics of SARS-CoV-2 within the cluster and to establish testing and isolation strategies [4,5]. In 2020, during the early COVID-19 pandemic, livestock slaughtering and processing facilities (SPFs) in the United States (US) and Europe were hotspots for COVID-19 outbreaks and were a primary cause of community transmission [6]. Work environments at SPFs are conducive to the spread of respiratory viruses among employees. Potential risk factors include proximity to colleagues during long working hours, increased breathing rates due to physically strenuous work, and difficulty complying with infectious disease prevention and control rules because of the need to shout to communicate with colleagues amid ambient noise, thus increasing the risk of droplet transmission. Moreover, the indoor temperature is maintained at 10 to 15 °C when processing livestock products, and since the survival period of SARS-CoV-2 is longer in lower-temperature environments, this increases the risk of viral spread through contact with contaminated surfaces. The jobs at SPFs are difficult, and most of the work is subcontracted. Subcontractors perform the core activities of SPFs, including receiving, slaughtering, and deboning livestock as well as storing in cold temperatures, cutting, packaging, and distributing meat. Subcontractors work with human resources offices to hire foreign workers, who live in dormitories and form communities to rest and eat together. Failures in physical distancing and personal hygiene (for instance, not wearing the correct personal protective gear, such as masks) are major risk factors for viral transmission [7]. Many reports have emerged of COVID-19 outbreaks in Korea in 2020 from various facilities. Regarding hotspots of community outbreaks, epidemiological studies and reports have been conducted on fitness centers, a call center, nursing facilities, and a taekwondo gym (Tables S1, S2) [8−11]. In the first half of 2021, outbreaks of COVID-19 occurred at 8 domestic SPFs, greatly impacting the community spread; however, epidemiological studies and reports on COVID-19 outbreaks in domestic SPFs are lacking.
- The prolonged COVID-19 pandemic has created a conflict between the economy and public healthcare. Although continuous social distancing suppresses the spread of infectious diseases, it imposes economic damage and burdens the medical system [12]. In particular, local economies and national food supplies can be adversely impacted by COVID-19 control measures affecting SPFs. However, proper distancing in daily life and preemptive vaccination can reduce the possibility of infection and prevent outbreaks [13]. Therefore, this study was conducted to identify the COVID-19 risk factors associated with SPFs and suggest an optimal intervention to limit the spread of COVID-19 through efficient infectious disease prevention and control measures in the event of an outbreak.
Introduction
- Study Design
- In a case series study, demographic characteristics of patients with confirmed COVID-19 infection were examined to investigate the association with SPFs in Korea between January and June 2021. Additionally, a retrospective cohort study was conducted to analyze the correlation between COVID-19 infection and risk factors among all employees of the SPFs at which COVID-19 outbreaks occurred.
- Study Population
- As of March 2021, 87 mammal SPFs (MSPFs) and 56 poultry SPFs (PSPFs) existed in Korea. Between January and June 2021, among the 8 facilities at which at least 10 confirmed COVID-19 cases were reported, 5 facilities (2 MSPFs and 3 PSPFs) with COVID-19 test results of all employees were examined. A total of 2,125 individuals were surveyed, including 2,007 employees across 5 facilities; of the 402 confirmed cases, 280 people were infected in the facilities and 122 were cases of secondary transmission related to these facilities (i.e., among employees’ families, acquaintances, etc.).
- Setting
- Spatially, an SPF comprises subsidiary support facilities including a lairage area, a slaughterhouse or harvest area, space for chilling/refrigeration/freezing, a meat processing area, and an office and other auxiliary areas [14]. The lairage area, located outside the SPF, serves as a temporary holding space for livestock before slaughter. To mitigate heat stress for the animals during the summer, a spray device is installed in the lairage area. The slaughterhouse or harvest area should be kept at a temperature of 15 ℃ or lower and should utilize an air conditioning system that circulates air. Stainless steel is recommended for the machinery and equipment. The mammalian slaughter process includes the following stages: live animal entry and lairage, stunning, bleeding, head and hoof removal, scalding/dehairing, evisceration, carcass preparation, chilling/freezing, and meat processing. The slaughter space tends to be hot and humid, with depilation occurring in a hot water tank at 58 ℃ and cleaning done with hot water or steam. In contrast, chilling is typically conducted at around 2 ℃ to stabilize the meat temperature, while freezing is done at temperatures below −40 ℃. As such, the harvest area is a high-temperature, high-humidity, and noisy environment, while the refrigeration/freezing area is a low-temperature environment [15,16].
- Processing can take place either in the same facility or at a dedicated processing facility. The poultry slaughter process involves live animal entry and lairage, electrical stunning, bleeding, scalding/defeathering, head and foot removal, evisceration, chilling, segmentation, processing, packaging, and cooling. Scalding/defeathering is performed by immersing the poultry in hot water treated with sodium carbonate. Evisceration is automated, and chilling for 1 hour is necessary to lower the meat temperature. The meat is either packaged immediately after segmentation or processed prior to packaging. Cooling should be maintained below −2 ℃. The processing part of the facility consists of a meat processing area and a by-product processing area; to maintain freshness, the temperature there should be maintained at approximately 4 ℃. Processing tables and equipment should be made of stainless steel. Finally, auxiliary supporting facilities include offices, laboratories, dressing/locker rooms, staff lounges, and cafeterias (Figure 1).
- SPF field workers include employees of the contractor that manages the facility, employees of subcontractors related to livestock product processing and distribution, and external workers such as inspectors (e.g., veterinarians), cafeteria staff, and environmental service and security workers.
- Case Definition
- For the 5 SPFs with COVID-19 outbreaks between January and June 2021, employees who tested positive on a polymerase chain reaction (PCR) test, as well as their family members and acquaintances who tested positive through community transmission due to contact with the employees, were evaluated.
- Data and Statistical Analysis
- Information on confirmed cases of SPF-related COVID-19 outbreaks was provided through the COVID-19 information management system and COVID-19 outbreak database of the Korea Disease Control and Prevention Agency. Epidemiological investigation reports from the local public health center regarding the employees of the 5 SPFs were used to collect data on the type of employment (contractor, subcontractor, or external company), workspace, type of residence (private home or dormitory), and COVID-19 test results.
- For statistical analysis, logistic regression analysis was performed using IBM SPSS ver. 22.0 (IBM Corp.). Orange software ver. 3.32.0 (Bioinformatics Laboratory, Faculty of Computer and Information Science, University of Ljubljana) was used to conduct the Fisher exact test and independent samples t-test. The demographic characteristics of the confirmed cases were categorized by sex, age, symptoms, nationality, and type of transmission, and numbers and ratios were described for each variable. To understand whether the employment type, workspace, and/or residence type affected COVID-19 transmission, the attack rate was calculated, and multivariate logistic regression analysis was performed to calculate the odds ratio (OR), 95% confidence interval, and p-value. Statistical significance was considered to be indicated by p-values <0.05. To determine whether the risk of COVID-19 and presence of symptoms differed depending on nationality, the t-test and chi-square test were conducted to characterize any differences in the average reverse transcription real-time PCR (RT-PCR) cycle threshold (Ct) values and asymptomatic percentages of the patients with confirmed COVID-19.
- Ethics Statement
- This study was approved by the Korea Disease Control and Prevention Agency Institutional Review Board (IRB No: 2022-10-2-PE-A).
Materials and Methods
- Outbreak Description
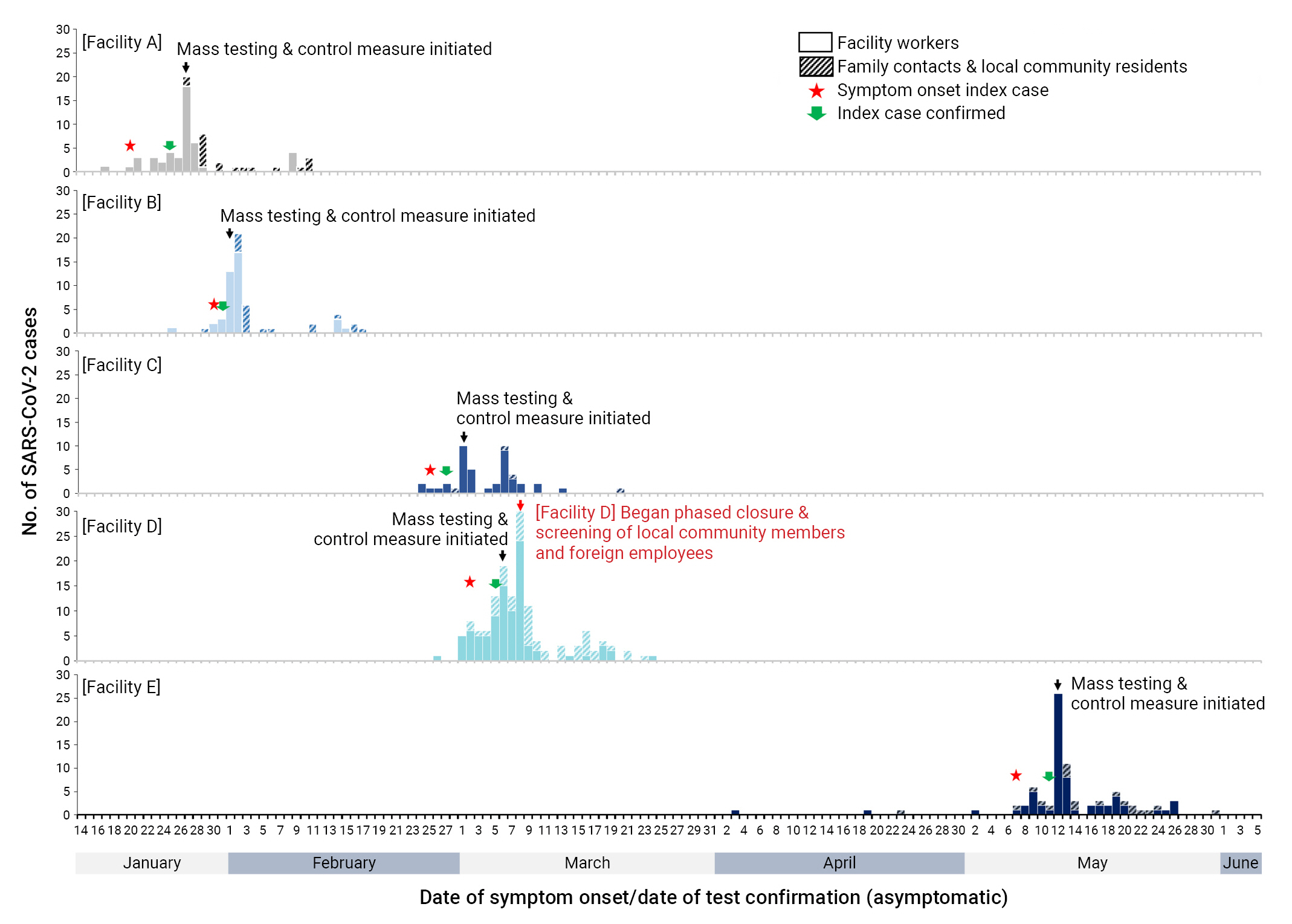
- Among the COVID-19 outbreaks at SPFs across Korea between January and June 2021, 3 PSPFs (facilities A, B, and C) and 2 MSPFs (facilities D and E) were investigated after all of their employees were tested for COVID-19. The slaughtering capacities were 150,000, 42,985, and 300,000 heads/day at facilities A, B, and C, respectively. Daily slaughters of 80 cows and 1,800 pigs at facility D and 400 cows and 3,000 pigs at facility E were reported. The COVID-19 attack rates during the outbreaks were 11.2%, 24.5%, 6.8%, 15.5%, and 25.2% at facilities A, B, C, D, and E, respectively. For both PSPFs and MSPFs, high slaughtering capacity was associated with a low COVID-19 attack rate.
- The index patient in facility A was a female foreign worker who lived in a dormitory and worked in carcass processing as an employee of a subcontractor. She had symptoms of cough and fever starting on January 20, 2021, and COVID-19 was confirmed on January 26, 2021. When all employees working at facility A and their 572 family members were tested for COVID-19, infection was confirmed in 27 employees and 3 family members. By February 10, when the outbreak ended, COVID-19 was confirmed in 44 of 392 employees at facility A (attack rate, 11.2%). Including the 22 family and community contacts confirmed to have COVID-19, a total of 66 patients were infected. The median age was 45.5 years, with more female patients (n=37, 56.1%) than male patients. The majority of those with COVID-19 were asymptomatic (n=40, 61.5%). The number of foreign patients (n=36, 54.5%) was greater than that of native Korean patients.
- The index patient at facility B was a native Korean man in charge of inspecting livestock products. He was tested for COVID-19 on January 29, 2021 due to symptoms of runny nose, headache, muscle pain, and cough, and COVID-19 was confirmed on February 1, 2021. An outbreak was suspected, and 33 additional cases were confirmed after COVID-19 testing of all 147 employees of facility B. By February 17, when the outbreak ended, 37 employees were confirmed to have COVID-19 (attack rate, 24.5%). The additional confirmation of 22 family and community contacts yielded a total of 59 confirmed cases. The median age was 44 years, with more male patients (n=33, 55.9%) than female patients. The majority of those with COVID-19 were asymptomatic (n=42, 71.2%). The number of native Korean patients (n=36, 61.0%) was greater than that of foreign patients.
- The index patient at facility C was a female foreign worker who lived in a dormitory and worked in carcass processing as an employee of a subcontractor. She was tested for COVID-19 on February 25, 2021 for symptoms of fever, chills, and muscle pain, and COVID-19 was confirmed on February 28, 2021. When all 736 employees of facility C and their family members were tested, COVID-19 was confirmed for 14 employees and 1 family member. By March 20, when the outbreak ended, 41 of 606 employees had been confirmed to have COVID-19 (attack rate, 6.8%). The additional confirmation of 4 family contacts yielded a total of 45 confirmed cases. The median age was 32 years, with more male patients (n=28, 62.2%) than female patients. Most patients were asymptomatic (n=28, 62.2%). Foreign workers accounted for the majority of the confirmed cases (n=41, 91.1%).
- The index patient at facility D was a native Korean female family member of an employee at the facility. She was tested on March 2, 2021 for symptoms of loss of taste, loss of smell, and runny nose, and COVID-19 was confirmed on March 6, 2021. An epidemiological survey of confirmed COVID-19 cases in the community revealed 2 facility D employees and 1 family member. When the coworkers and family contacts of the confirmed patients associated with facility D were tested, 11 employees and 3 family contacts were found to have COVID-19. An outbreak was suspected, and all employees of facility D as well as their family and community contacts were tested on March 7, 2021. Overall, 66 employees and 11 family and community contacts were confirmed to have COVID-19. On March 8, 2021, part of facility D was closed for 2 weeks, and preemptive COVID-19 testing was conducted among foreign community residents. By March 24, when the outbreak ended, 93 of 600 employees had been confirmed to have COVID-19 (attack rate, 15.5%). Including an additional 51 family members and community contacts, a total of 144 confirmed COVID-19 cases were recorded. The median age was 51 years, with more male patients (n=99, 68.8%) than female patients. More patients had mild symptoms (n=82, 56.9%) than were asymptomatic, and 4 patients (2.8%) died. The number of native Korean patients (n=105, 72.9%) was greater than that of foreign patients.
- The index patient in facility E was a native Korean woman. As an employee of the contractor, she worked in carcass processing. She was tested for COVID-19 on May 7, 2021 for symptoms of cough and sore throat, and COVID-19 was confirmed on May 11, 2021. On May 12, 2021, all employees of facility E were tested for COVID-19, which was confirmed in 37 people. By May 31, when the outbreak ended, 65 of 258 employees were confirmed positive for COVID-19 (attack rate, 25.2%). Including 20 family members and community contacts, 85 COVID-19 cases were confirmed in total. The median age was 47 years, with more men (n=61, 69.3%) than women. The number of asymptomatic patients (n=46, 52.3%) was greater than that of symptomatic patients, and 2 patients (2.3%) died. The number of foreign patients (n=47, 53.4%) was greater than that of native Korean patients (Table 1; Figure 2).
- Analysis of Risk Factors
- Logistic regression analysis was conducted to examine the effects of the type of employment, work area, and type of residence on the risk of COVID-19. For the PSPFs, multivariate analysis revealed that subcontractor employees (OR, 2.09; p=0.018), external worker status (OR, 0.04; p<0.001), work in the refrigeration/freezing area (OR, 12.09; p<0.001), work in the inspection area (OR, 34.38; p=0.002), work area other than harvest and livestock product processing (OR, 0.46, p=0.011), and dormitory living (OR, 4.54; p<0.001) were significant risk factors for COVID-19. The infection risk was 2.09 times higher among employees of subcontractors than among contractor employees. Moreover, the external workers had a 96% lower COVID-19 risk than the contractor employees. The COVID-19 risk was 12.09-fold higher among those working in the refrigeration/freezing area than among the office area employees, and workers in the inspection area were also at a higher risk of infection relative to the office area employees. Employees performing tasks other than harvest and livestock product processing had a 54% lower COVID-19 risk relative to office area employees. The risk of COVID-19 was 4.54-fold higher among employees living in dormitories than among those living in private homes.
- For the MSPFs, multivariate analysis revealed that external worker status (OR, 0.17; p=0.013), work in the by-product processing area (OR, 5.21; p=0.011), work in the carcass cutting area (OR, 4.95; p=0.017), and dormitory living (OR, 3.34; p<0.001) were significant risk factors for COVID-19. External workers had an 83% lower COVID-19 risk relative to contractor employees. Employees working in the by-product processing area and carcass cutting area had 5.21-fold and 4.95-fold higher risks of infection, respectively, relative to those working in the office area. Additionally, those living in dormitories had a 3.34-fold higher risk of COVID-19 than those living in private homes (Table 2).
- Comparison Between Native Korean and Foreign Employees
- A contingency table was prepared to verify the difference in the proportion of symptomatic and asymptomatic patients by nationality among the employees confirmed to have COVID-19. Among the foreign workers at PSPFs, 61 (66.3%) were asymptomatic and 31 (33.7%) were symptomatic, whereas among the native Korean workers, 12 (40.0%) were asymptomatic and 18 (60.0%) were symptomatic. Among the foreign workers at MSPFs, 42 (60.0%) were asymptomatic and 28 (40.0%) were symptomatic, whereas among the native Korean workers, 36 (40.9%) were asymptomatic and 52 (59.1%) were symptomatic. The chi-square test was conducted to determine the statistical significance of the association of symptoms with nationality. The presence of symptoms differed significantly by nationality for both PSPFs and MSPFs (p<0.05). The proportion of asymptomatic cases was higher among the foreign than the native Korean employees (Table 3).
- To examine whether the high proportion of asymptomatic patients among foreign employees influenced the delay in COVID-19 testing, an independent samples t-test was conducted on the RT-PCR Ct values to verify whether the viral load differed significantly according to nationality. The average Ct values of the foreign employees in the PSPFs and MSPFs were 3.0 points and 2.7 points higher than those of the native Korean employees, respectively, constituting a significant difference (p<0.05) (Figure 3).
Results
- Comparing the daily slaughter processing capacity and attack rate of COVID-19 at 5 SPFs with outbreaks between January and June 2021 revealed that higher slaughter processing capacity was associated with a lower COVID-19 attack rate. In Korea, the Slaughterhouse Restructuring Act was implemented in 2009 to modernize, automate, and expand SPFs. However, smaller SPFs still face problems, such as outdated facilities and low sanitation levels [17]. Thus, the relatively low COVID-19 attack rates in higher-capacity SPFs were attributed to the lower density of employees due to automation as well as the improved working conditions associated with a modernized facility, such as better ventilation and sanitation. In contrast, in a study by Taylor et al. [7] of outbreaks in abattoirs in the US, greater processing capacity was associated with a higher COVID-19 attack rate. Larger abattoirs in the US employ more people and involve more activities than smaller operations. Moreover, because such facilities require a larger physical space, employees must shout louder to communicate, leading to increased droplet generation. Therefore, according to that US study, employees in larger facilities are particularly vulnerable to respiratory virus transmission. Furthermore, in outbreaks in Irish slaughterhouses, 0.5% of small slaughterhouses managed by local governments and 15.3% of large slaughterhouses managed by the central government had COVID-19 outbreaks, demonstrating that larger facilities are more vulnerable than smaller facilities to COVID-19 transmission [18].
- Multivariate logistic regression analysis showed that the high-risk areas for COVID-19 transmission in the SPFs were the refrigeration/freezing area, the by-product processing area, and the carcass cutting area, with 12.1-fold, 5.2-fold, and 5.0-fold higher risks of COVID-19, respectively, than the office area. Potential contributors to the risk of respiratory viral outbreaks in these areas include a low-temperature environment, a low ventilation rate and continuous air recirculation, stainless steel machinery and equipment, proximity between workers, and intense physical labor [19]. Studies have reported that SARS-CoV-2 survives longer in environments with higher relative humidity and lower temperature, as well as on stainless steel surfaces, resulting in an increased risk of COVID-19 [20,21]. Moreover, complying with infectious disease prevention and control measures is difficult when working in proximity to coworkers, as is wearing masks due to the intense physical work required [22]. Furthermore, Iulietto et al. [22] found that the noise level of machines in the workplace was 85 to 100 dB, and workers had to shout at 85 dB or louder to communicate. This reportedly increases the risk of COVID-19 by promoting droplet production [23]. In a German slaughterhouse, similar to our study, the infection risk was 2.4 times and 2.3 times greater for carcass cutting and slaughter workers, respectively, compared with their counterparts working in the office [24]. Additionally, in a mass outbreak in a slaughterhouse in the US, the incidence of COVID-19 was higher among employees cutting carcasses, processing livestock products, and slaughtering than in those who worked in other departments; this was attributed to the difficulty keeping a safe distance from coworkers [25]. Overall, these results indicate that the working environment is a major risk factor for infection transmission. Employees in charge of inspection have limited exposure to COVID-19 because they rarely enter the slaughtering area, as their role involves inspecting the pathological conditions of the slaughtered livestock. In overseas cases, the inspection staff who rarely entered the slaughtering area were not infected [26]. However, in the present study, infection was confirmed in 2 inspection staff members in facility B among the 5 SPFs. During breaks and at lunchtime, employees leave their work areas and gather in cafeterias and break rooms to remove their masks and eat. These common areas are conducive to the spread of viruses among employees [27]. Therefore, the inspection staff were assumed to have been infected with COVID-19 in this public area.
- The risk of COVID-19 was 2.1 times higher among employees of subcontractors than among contractor employees. The contractor provides the slaughterhouse facilities and offers tasks to subcontractors according to consumer demand. Subcontractors manage contracting with producers, slaughtering, and processing. Therefore, the core activities of an SPF, such as receiving livestock, slaughtering, deboning, refrigeration/freezing, cutting, processing, and packaging, are primarily performed by subcontractors. These activities are conducted in work environments with a high risk of COVID-19, and because they require intense labor, they provide a constant risk of occupational diseases such as musculoskeletal disorders. Therefore, it is difficult to distinguish between symptoms of COVID-19 and those of occupational diseases, hindering the early-stage detection of COVID-19 and resulting in a high risk of outbreak [27]. According to a study by Mallet et al. [27], the risk of COVID-19 among subcontractor employees was 3 times higher than that among contractor employees in a French abattoir facility. In a German slaughterhouse in the study by Finci et al. [23], the risk of COVID-19 among the employees of subcontractors was 1.4 times higher than that among employees of the contractor. A study in the US showed that the cumulative incidence of COVID-19 was 1.8 times higher in non-regular workers at a slaughterhouse facility than in regular workers [25]. The findings of this study also showed that the risk of COVID-19 was higher among the employees of subcontractors than among contractor employees.
- Foreign workers had 5.3-fold and 3.0-fold higher risk of COVID-19 than native Korean workers in PSPFs and MSPFs, respectively. The proportions of asymptomatic cases were 66.3% and 60.0% among foreigners working in PSPFs and MSPFs, respectively; these were higher than those of their native Korean counterparts (40.0% and 40.1%, respectively). According to a study by He et al. [28], the proportion of asymptomatic cases among patients with COVID-19 was estimated to be 15% to 20%, and the present study reported a high proportion of asymptomatic cases in the SPFs. To verify whether the delay in COVID-19 detection impacted the proportion of asymptomatic cases, for both PSPFs and MSPFs, the viral loads of the employees confirmed to have COVID-19 were compared using RT-PCR. The results showed that the average Ct value was higher among foreign employees than native Korean employees. This suggests that COVID-19 confirmation took longer in foreign employees than in the native Korean workers. Thus, it was assumed that foreign employees had either had no symptoms, had mild symptoms in the past that went unrecognized, or had symptoms but did not report them, resulting in the spread of COVID-19. Additionally, the fact that many of the foreign employees lived in dormitories may have affected the viral spread. These results show that foreign workers are an important factor in COVID-19 transmission. The number of foreign employees in Korea is increasing due to the sharp drop in the working population following low birth rates in this rapidly aging society [29]. Foreign workers, who primarily hold non-regular positions, engage in physically demanding tasks and are susceptible to infectious diseases due to their communal living arrangements in dormitories [30]. These residences are often located on the outskirts of the city, inside the workplace, or in a factory, where access to hospitals or medical welfare facilities is difficult [31]. Furthermore, foreign workers’ use of medical institutions may be limited due to treatment costs, poor protection of rights, and communication difficulties. Those without a residence permit have limited access to medical services and often avoid treatment and consultations for infectious diseases out of fear of being deported [32].
- This study had some limitations. First, only 5 SPFs that reported outbreaks between January and June 2021 had COVID-19 test records for all employees. Thus, the results may not be representative of all SPFs with an outbreak during that period in Korea. Second, the calculated risks of COVID-19 for contractors and subcontractors may have been underestimated. Foreign workers are often hired by main contractors through a human resource agency. In some cases, the foreign workers, who are non-regular workers, are classified as employees of the main contractor even though they are employees of subcontractors. Therefore, considering that slaughterhouse facilities have many confirmed foreign workers, the risk of subcontractors may have been underestimated; hence, caution is needed in future analysis. Third, data may have been omitted regarding confirmed cases of community transmission. A limit exists to tracking the people classified as close contacts after an SPF employee or visitor moves to another area, which may contribute to more cases of community spread and additional outbreaks. Therefore, the attack rate is likely an underestimate of the actual prevalence. Fourth, SARS-CoV-2 transmission can occur through multiple routes in SPFs. Identifying risk factors in facilities with many confirmed cases can be difficult due to the extensive transmission that has already occurred. Additionally, regression analysis may be insufficient to identify higher risk factors in situations where ventilation systems, workplace density, and housing arrangements for workers differ. Consequently, analyzing epidemiological data from each facility is necessary to identify high-risk work environments in a facility-specific manner. Fifth, Ct values exhibit notable variability, and in patients infected with SARS-CoV-2, they decrease gradually during the first week of infection and subsequently increase progressively over time [33]. Nevertheless, in this study, it was assumed that all patients with COVID-19 from 1 of the 5 facilities had contracted the virus through contact with other confirmed cases within the same facility, and that uniform sample amounts were collected from identical locations. Moreover, a higher Ct value was presumed to correspond to a longer infection period. Sixth, personal information collection for contacts was not explicitly stated in the Infectious Disease Control and Prevention Act, limiting the ability to adjust for demographic characteristics such as sex and age, which are recognized risk factors. Consequently, this study reports risk factor findings based on the social and spatial characteristics of SPF employees, including the type of employment, working area, and type of residence.
Discussion
- Between January and June 2021, 402 COVID-19 cases were reported at 5 domestic SPFs, with 280 people infected in the facilities and 122 infected by community transmission due to outbreaks. In contrast with overseas studies, the attack rate of COVID-19 in domestic SPFs was lower in larger facilities than in smaller facilities, and additional research is needed to determine the cause of this finding. SPFs are associated with many potential risk factors for COVID-19, including social and spatial factors. The risk levels of COVID-19 in the refrigeration/freezing, by-product processing, and carcass cutting areas were 12.1 times, 5.2 times, and 5.0 times higher than that in the office area, respectively. Therefore, to prevent a COVID-19 outbreak, it is important to conduct periodic preemptive testing and symptom monitoring of those working in spaces with a high risk of COVID-19 exposure and to continuously disinfect common spaces. Social risk factors include employer type and foreign worker status (nationality). At PSPFs, the COVID-19 risk was 2.1 times higher among the employees of subcontractors than the employees of contractors. Regarding nationality, foreign workers in PSPFs and MSPFs had 5.3-fold and 3.0-fold higher risk of COVID-19, respectively, than domestic workers. Therefore, in the event of a confirmed COVID-19 case, an outbreak can be prevented by isolating a wide range of contacts or by conducting preemptive COVID-19 testing of all employees in the facility. Foreign workers are an important part of domestic industrial activities as well as slaughterhouse facilities and will gradually become more relied upon in the future. However, in the context of infection control, they face difficulties in daily life, including challenges receiving treatment at domestic medical institutions and communication issues. Therefore, to manage infectious diseases efficiently in domestic SPFs, continuous efforts to improve the infection control system and environmental risk factors within each facility are warranted, as well as a better understanding of the effects of viral transmission, especially via foreign workers.
Conclusion
- • Between January and June 2021, 402 COVID-19 cases were reported at 5 domestic livestock slaughtering and processing facilities (SPFs) with 280 people infected in the facilities and 122 infected by community transmission due to outbreaks.
- • To efficiently manage infectious diseases in domestic SPFs, continuous efforts to improve infection control systems and address environmental risk factors within each facility are warranted, as is an improved understanding of the effects of viral transmission, particularly via foreign workers.
HIGHLIGHTS
-
Ethics Approval
This study was approved by the Korea Disease Control and Prevention Agency Institutional Review Board (IRB No: 2022-10-2-PE-A).
-
Conflicts of Interest
The authors have no conflicts of interest to declare.
-
Funding
None.
-
Availability of Data
The data used in this study are protected under the Personal Information Protection Act.
-
Authors’ Contributions
Conceptualization: all authors; Date curation: all authors; Formal analysis: all authors; Investigation: SC; Methodology: all authors; Project administration: YKL, TJS; Resources: all authors; Software: all authors; Supervision: TJS; Validation: all authors; Visualization: all authors; Writing-original draft: SC; Writing-review & editing: YKL, TJS. All authors read and approved the final manuscript.
-
Additional Contributions
We thank the relevant ministries, including those at local and provincial levels, for their effort in responding to COVID-19 outbreaks.
Article information
Supplementary Material
Table S2.


| Characteristic |
PSPFs |
MSPFs |
||||||
|---|---|---|---|---|---|---|---|---|
| No. of workers | No. of patients | OR (95% CI) | p | No. of workers | No. of patients | OR (95% CI) | p | |
| Type of employment | ||||||||
| Contractora) employee | 375 | 26 | Ref. | 181 | 52 | Ref. | ||
| Subcontractorb) employee | 517 | 91 | 2.09 (1.14–3.85) | 0.018* | 446 | 101 | 1.22 (0.43–3.42) | 0.710 |
| External workerc) | 257 | 5 | 0.04 (0.01–0.18) | <0.001*** | 231 | 5 | 0.17 (0.04–0.69) | 0.013* |
| Working area | ||||||||
| Office | 86 | 7 | Ref. | 87 | 4 | Ref. | ||
| Harvest | 45 | 18 | 1.82 (0.60–5.54) | 0.291 | 29 | 8 | 2.99 (0.76–11.82) | 0.119 |
| By-product processing | 44 | 7 | 0.41 (0.12–1.45) | 0.167 | 180 | 80 | 5.21 (1.46–18.59) | 0.011* |
| Refrigeration/freezing | 95 | 12 | 12.09 (3.47–42.16) | <0.001*** | 78 | 4 | 0.40 (0.08–1.93) | 0.251 |
| Carcass cutting | 115 | 15 | 0.41 (0.14–1.21) | 0.107 | 79 | 30 | 4.95 (1.33–18.43) | 0.017* |
| Meat processing | 420 | 58 | 0.48 (0.19–1.25) | 0.133 | 236 | 23 | 0.82 (0.22–3.04) | 0.770 |
| Inspection | 19 | 2 | 34.38 (3.63–325.40) | 0.002** | 32 | 1 | 2.38 (0.20–28.65) | 0.494 |
| Othersd) | 325 | 3 | 0.46 (0.14–0.65) | 0.011* | 137 | 8 | 1.29 (0.36–4.61) | 0.693 |
| Residence | ||||||||
| Private home | 726 | 30 | Ref. | 670 | 86 | Ref. | ||
| Dormitory | 423 | 92 | 4.54 (2.56–8.04) | <0.001*** | 188 | 72 | 3.34 (2.16–5.16) | <0.001*** |
Data were adjusted for several variables (type of employment, working area, and residence) using logistic regression analysis.
PSPF, poultry slaughtering and processing facility; MSPF, mammal slaughtering and processing facility; OR, odds ratio; CI, confidence interval; Ref. reference.
a) A company that performs work on a contract basis and arranges to supply materials.
b) A company that signs a contract to perform some or all of the obligations of the contractor.
c) Inspectors (e.g., veterinarians), cafeteria staff, environmental service workers, security workers, etc.
d) Workers performing tasks other than slaughtering livestock and processing livestock products.
* p<0.05,
** p<0.01,
*** p<0.001.
| Facility type | Symptoms |
Nationality |
p | |
|---|---|---|---|---|
| Foreign | Native | |||
| PSPF | Total | 92 (100.0) | 30 (100.0) | 0.017* |
| Asymptomatic | 61 (66.3) | 12 (40.0) | ||
| Symptomatic | 31 (33.7) | 18 (60.0) | ||
| MSPF | Total | 70 (100.0) | 88 (100.0) | 0.025* |
| Asymptomatic | 42 (60.0) | 36 (40.9) | ||
| Symptomatic | 28 (40.0) | 52 (59.1) | ||
- 1. Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun 2020;109:102433. ArticlePubMedPMC
- 2. Tsang HF, Chan LW, Cho WC, et al. An update on COVID-19 pandemic: the epidemiology, pathogenesis, prevention and treatment strategies. Expert Rev Anti Infect Ther 2021;19:877−88.ArticlePubMed
- 3. Asghar A, Imran HM, Bano N, et al. SARS-COV-2/COVID-19: scenario, epidemiology, adaptive mutations, and environmental factors. Environ Sci Pollut Res Int 2022;29:69117−36.ArticlePubMedPMCPDF
- 4. Liu T, Gong D, Xiao J, et al. Cluster infections play important roles in the rapid evolution of COVID-19 transmission: a systematic review. Int J Infect Dis 2020;99:374−80.ArticlePubMedPMC
- 5. Hong K, Yum S, Kim J, et al. Epidemiology and regional predictors of COVID-19 clusters: a Bayesian spatial analysis through a nationwide contact tracing data. Front Med (Lausanne) 2021;8:753428. ArticlePubMedPMC
- 6. Waltenburg MA, Victoroff T, Rose CE, et al. Update: COVID-19 among workers in meat and poultry processing facilities. United States, April-May 2020. MMWR Morb Mortal Wkly Rep 2020;69:887−92.PubMedPMC
- 7. Taylor CA, Boulos C, Almond D. Livestock plants and COVID-19 transmission. Proc Natl Acad Sci U S A 2020;117:31706−15.ArticlePubMedPMC
- 8. Bae S, Kim H, Jung TY, et al. Epidemiological characteristics of COVID-19 outbreak at fitness centers in Cheonan, Korea. J Korean Med Sci 2020;35:e288.ArticlePubMedPMCPDF
- 9. Song R, Kim HS, Yoo SJ, et al. COVID-19 in nursing facilities: experience in Republic of Korea. Osong Public Health Res Perspect 2020;11:164−9.ArticlePubMedPMCPDF
- 10. Park SY, Kim YM, Yi S, et al. Coronavirus disease outbreak in call center, South Korea. Emerg Infect Dis 2020;26:1666−70.ArticlePubMedPMC
- 11. Shin SH, Park E, Kim S, et al. COVID-19 outbreak and risk factors for infection in a taekwondo gym in the Republic of Korea. Osong Public Health Res Perspect 2022;13:162−70.ArticlePubMedPMCPDF
- 12. Chen K, Pun CS, Wong HY. Efficient social distancing during the COVID-19 pandemic: integrating economic and public health considerations. Eur J Oper Res 2023;304:84−98.ArticlePubMed
- 13. Saha S, Samanta G, Nieto JJ. Impact of optimal vaccination and social distancing on COVID-19 pandemic. Math Comput Simul 2022;200:285−314.ArticlePubMedPMC
- 14. Jang YY, Kim SW. Basic research on guidelines of estimation of optimum spatial size of the slaughtering plants in Korea. J Archit Inst Korea 2009;25:115−26. Korean.
- 15. Berkowitz DE, Fagel MJ. Meatpacking/processing [Internet]. Encyclopaedia of Occupational Health and Safety; 2011 [cited 2023 Apr 19]. Available from: https://iloencyclopaedia.org/part-x-96841/food-industry/food-processing-sectors/item/860-meatpacking/processing.
- 16. Ashdown T. Poultry processing [Internet]. Encyclopaedia of Occupational Health and Safety; 2011 [cited 2023 Apr 19]. Available from: https://iloencyclopaedia.org/part-x-96841/food-industry/food-processing-sectors/item/861-poultry-processing.
- 17. Government of Ireland. Investigation into a series of outbreaks of COVID-19 in meat processing plants in Ireland, 2020 [Internet]. Government of Ireland; 2020 [cited 2023 Apr 19]. Available from: https://assets.gov.ie/95603/8c23ae9c-9a30-4c01-9ebf-f624f2c99702.pdf.
- 18. Gunther T, Czech-Sioli M, Indenbirken D, et al. SARS-CoV-2 outbreak investigation in a German meat processing plant. EMBO Mol Med 2020;12:e13296.PubMedPMC
- 19. Dietz L, Horve PF, Coil DA, et al. 2019 Novel Coronavirus (COVID-19) pandemic: built environment considerations to reduce transmission. mSystems 2020;5:e00245−20.ArticlePubMedPMCPDF
- 20. Chin AW, Chu JT, Perera MR, et al. Stability of SARS-CoV-2 in different environmental conditions. Lancet Microbe 2020;1:e10.ArticlePubMedPMC
- 21. Dyal JW, Grant MP, Broadwater K, et al. COVID-19 among workers in meat and poultry processing facilities: 19 States, April 2020. MMWR Morb Mortal Wkly Rep 2020;69.
- 22. Iulietto MF, Sechi P, Gaudenzi CM, et al. Noise assessment in slaughterhouses by means of a smartphone app. Ital J Food Saf 2018;7:7053. ArticlePubMedPMCPDF
- 23. Finci I, Siebenbaum R, Richtzenhain J, et al. Risk factors associated with an outbreak of COVID-19 in a meat processing plant in southern Germany, April to June 2020. Euro Surveill 2022;27:2100354. ArticlePubMedPMC
- 24. Steinberg J, Kennedy ED, Basler C, et al. COVID-19 outbreak among employees at a meat processing facility: South Dakota, March-April 2020. MMWR Morb Mortal Wkly Rep 2020;69:1015−9.ArticlePubMedPMC
- 25. Brandt MP, Jager W, Epple S, et al. SARS-CoV-2 outbreak in medical employees in a large urologic department: Spread, containment and outcome. Am J Infect Control 2021;49:674−7.ArticlePubMedPMC
- 26. Klinkenberg P. EFFAT Report Covid-19 outbreaks in slaughterhouses and meat processing plants [Internet]. European Federation of Trade Unions in the Food, Agriculture and Tourism; 2020 [cited 2023 Apr 19]. Available from: https://policycommons.net/artifacts/1910215/effat-report-covid-19-outbreaks-in-slaughterhouses-and-meat-processing-plants/2661391/.
- 27. Mallet Y, Pivette M, Revest M, et al. Identification of workers at increased risk of infection during a COVID-19 outbreak in a meat processing plant, France, May 2020. Food Environ Virol 2021;13:535−43.ArticlePubMedPMCPDF
- 28. He J, Guo Y, Mao R, Zhang J. Proportion of asymptomatic coronavirus disease 2019: a systematic review and meta-analysis. J Med Virol 2021;93:820−30.ArticlePubMedPDF
- 29. Won YH, Choi SH. A study on the effects of medical service supports on adaptation of foreign workers into Korean society. J Community Welf 2011;38:29−50. Korean.
- 30. Noh JC. Problems and solutions of foreign workers undocumented. J Labor Law 2010;18:37−90. Korean.
- 31. Lee JM. The housing and living conditions of immigrant workers and their policy implications. Health Welf Policy Forum 2021;295:57−72. Korean.
- 32. Lee BW, Ko ZK. Study on conditions and problems of the medical services (the health and medical care) for the foreign workers. Hanyang Law Rev 2010;21:323−52. Korean.
- 33. Fang FC, Naccache SN, Greninger AL. The laboratory diagnosis of Coronavirus disease 2019: frequently asked questions. Clin Infect Dis 2020;71:2996−3001.ArticlePubMedPDF
References
Figure & Data
References
Citations

- Figure
- Related articles
-
- Risk factors for transmission in a COVID-19 cluster infection in a high school in the Republic of Korea
- Vaccine effectiveness and the epidemiological characteristics of a COVID-19 outbreak in a tertiary hospital in Republic of Korea
- Risk factors for deaths associated with COVID-19 according to the cause of death classification in Republic of Korea
- Early countermeasures to COVID-19 at long-term care facilities in Gwangju Metropolitan City, Republic of Korea
- COVID-19 outbreak and risk factors for infection in a taekwondo gym in the Republic of Korea



 Cite
Cite