Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 11(4); 2020 > Article
-
Original Article
Secondhand Smoking Among Children in Rural Households: A Community Based Cross-Sectional Study in Bangladesh - Rishad Choudhury Robina, Narongsak Noosornb, Sheikh Mohammad Alifc
-
Osong Public Health and Research Perspectives 2020;11(4):201-208.
DOI: https://doi.org/10.24171/j.phrp.2020.11.4.09
Published online: August 31, 2020
aDepartment of Community Health, Faculty of Public Health, Naresuan University, Phitsanulok, Thailand
bFaculty of Public Health, Naresuan University, Phitsanulok, Thailand
cepartment of Epidemiology and Preventive Medicine, School of Public Health and Preventive Medicine, Monash University, Melbourne, Australia
- *Corresponding author: Rishad Choudhury Robin, Department of Community Health, Faculty of Public Health, Naresuan University, Phitsanulok, Thailand, Email: rcrobinbd@yahoo.com
• Received: December 26, 2019 • Revised: February 27, 2020 • Accepted: March 20, 2020
Copyright ©2020, Korea Centers for Disease Control and Prevention
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Abstract
-
Objectives
- This study aimed to determine the factors associated with reducing exposure to secondhand smoke among children in households of rural Bangladesh.
-
Methods
- A cross-sectional study of 410 smokers and non-smokers, in 6 villages of Munshigonj district was conducted. Data were collected randomly using a self-administrative questionnaire. Differences between variables were assessed using Chi-square or Fisher’s exact test (as appropriate). Univariate and multivariate logistic regression models were used to investigate associations. All results were presented as unadjusted and adjusted odds ratios with a 95% confidence interval. The level of statistical significance was reached when p < 0.05.
-
Results
- A smoker in the household was determined to be a risk factor associated with exposure of other household members to secondhand smoke (p < 0.001). Higher education, strict implementation of household smoke-free rules, a higher influence of social norms and culture, as well as moderate knowledge on exposure to secondhand smoke were considered as preventive factors associated with exposure of others in the home to secondhand smoke.
-
Conclusion
- Exposure to secondhand smoke is an extensive and preventable risk factor for children, and reducing exposure to secondhand smoke will have a largely positive effect in the community. An effective public health intervention model may reduce secondhand smoking.
- Exposure to secondhand smoke has no safe limit [1]. Globally, each year, around 890,000 deaths occurred due to secondhand smoking [2]. Children are considered to be the most vulnerable group in a population to be exposed to the harmful effects of secondhand smoke [3]. Though children worldwide are exposed to secondhand smoke in public places, the home is where children are most vulnerable [2,4].
- The prevalence of secondhand smoking amongst children is a potential public health concern worldwide. It was estimated that 41% of children were exposed to secondhand smoke in the United Kingdom, 43% in Australia, 12%-34% in the USA, and 33% in Canada whereas, the highest prevalence of exposure to secondhand smoke was 89% in Turkish children [5]. It has been reported that between 2008–2013 the prevalence for passive smoking in children above 15 years in Indonesia was 80%, whilst in Vietnam it was 75%, and in China it was 67% [6].
- Secondhand smoking contributes to significant health problems in children [1]. Among the 4,000 chemicals inhaled from tobacco smoke, 250 have been identified in secondhand smoke, and 50 of these chemicals are known carcinogens [5]. Apart from cancer, exposure to secondhand smoke has been reported to be associated with several respiratory diseases (including asthma, respiratory infections such as bronchitis and pneumonia, wheezing, coughing), ear infections, sudden infant death syndrome, and slow fetal growth and lung development [1].
- The prevalence of secondhand smoking in Bangladesh is high and thought to be attributable to the low cost availability of cigarettes, leading to high rates of smoking in the population [2]. A previous study in 2011, reported that the prevalence of secondhand smoking among children (< 18 years) in Bangladesh was 40% [7]. Previous studies in 2013 and 2017 identified the prevalence of secondhand smoking was 39% for adults and 31.1% for 13–15 aged children in Bangladesh [8,9]. Furthermore, a recent study in 2017 reported that the secondhand smoking rate increased to 95% in the urban areas of Dhaka, Bangladesh [10]. Although there is despite a reduction of 8% in cigarette smoking from 2009 to 2017 in Bangladesh [8]. However, the overall rates for smoking, including consumption of different tobacco products, including smokeless tobacco, are still high [11].
- Smoking is a common practice among many adults in Bangladesh and people generally have very low concerns regarding the adverse health effects of secondhand smoking [12]. Many people believe that secondhand smoking does not have any adverse effects. Moreover, in Bangladesh, male attitudes and behaviors pose a significant barrier to reducing secondhand smoking [7]. Additionally, gender, age, literacy, household incomes, and number of smokers in the family were influential factors contributing to the exposure of adults who do not smoke [13]. Furthermore, among women, poor socioeconomic status, religious beliefs, educational status, and having children had a significant role in exposure to secondhand smoke [14].
- In Bangladesh, research into secondhand smoking is limited, and exposure of children to secondhand smoke in rural homes has not been explored. This study aimed to determine the factors associated with secondhand smoking in children from rural households of Bangladesh.
Introduction
- 1. Study design and population
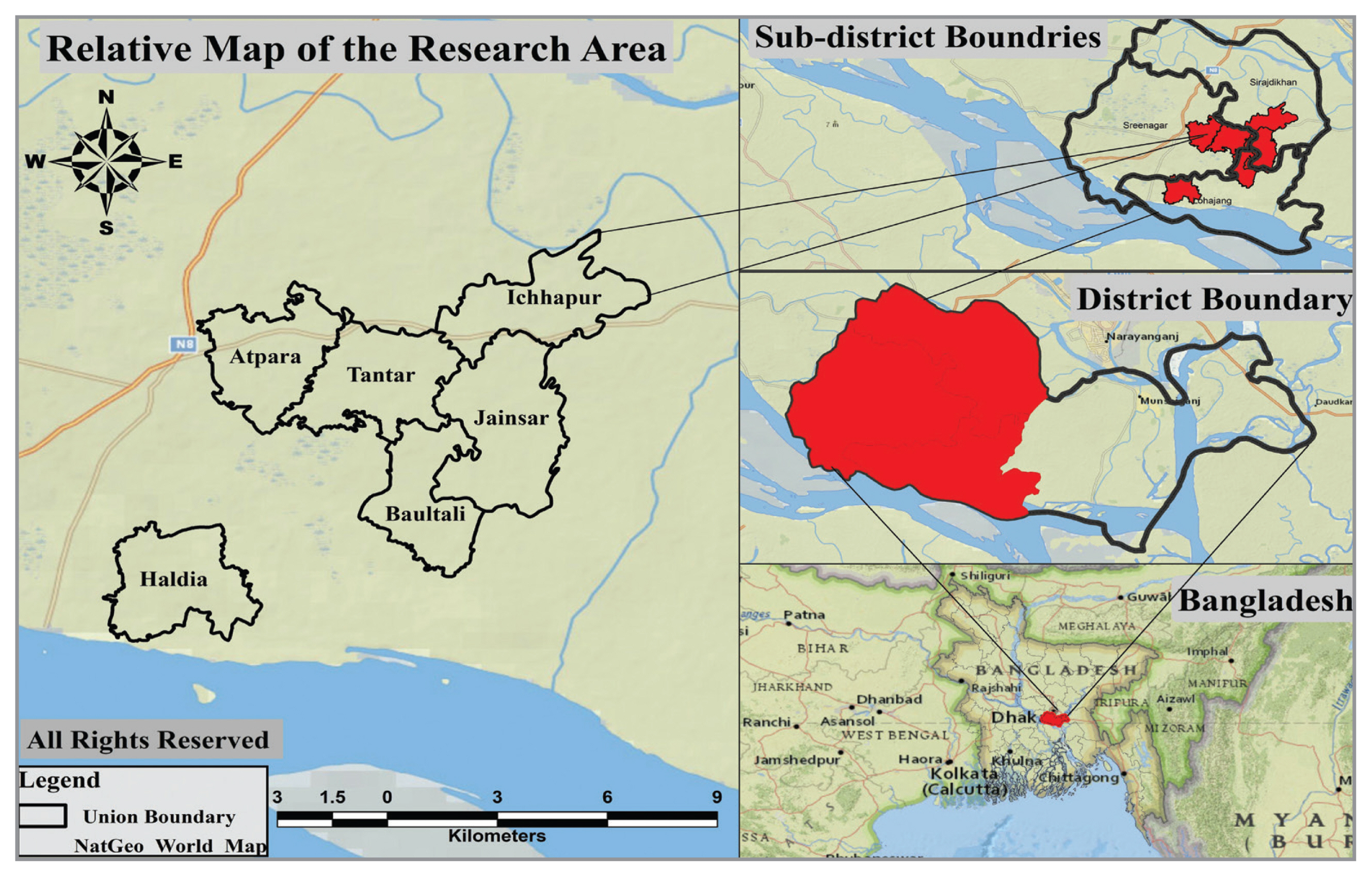
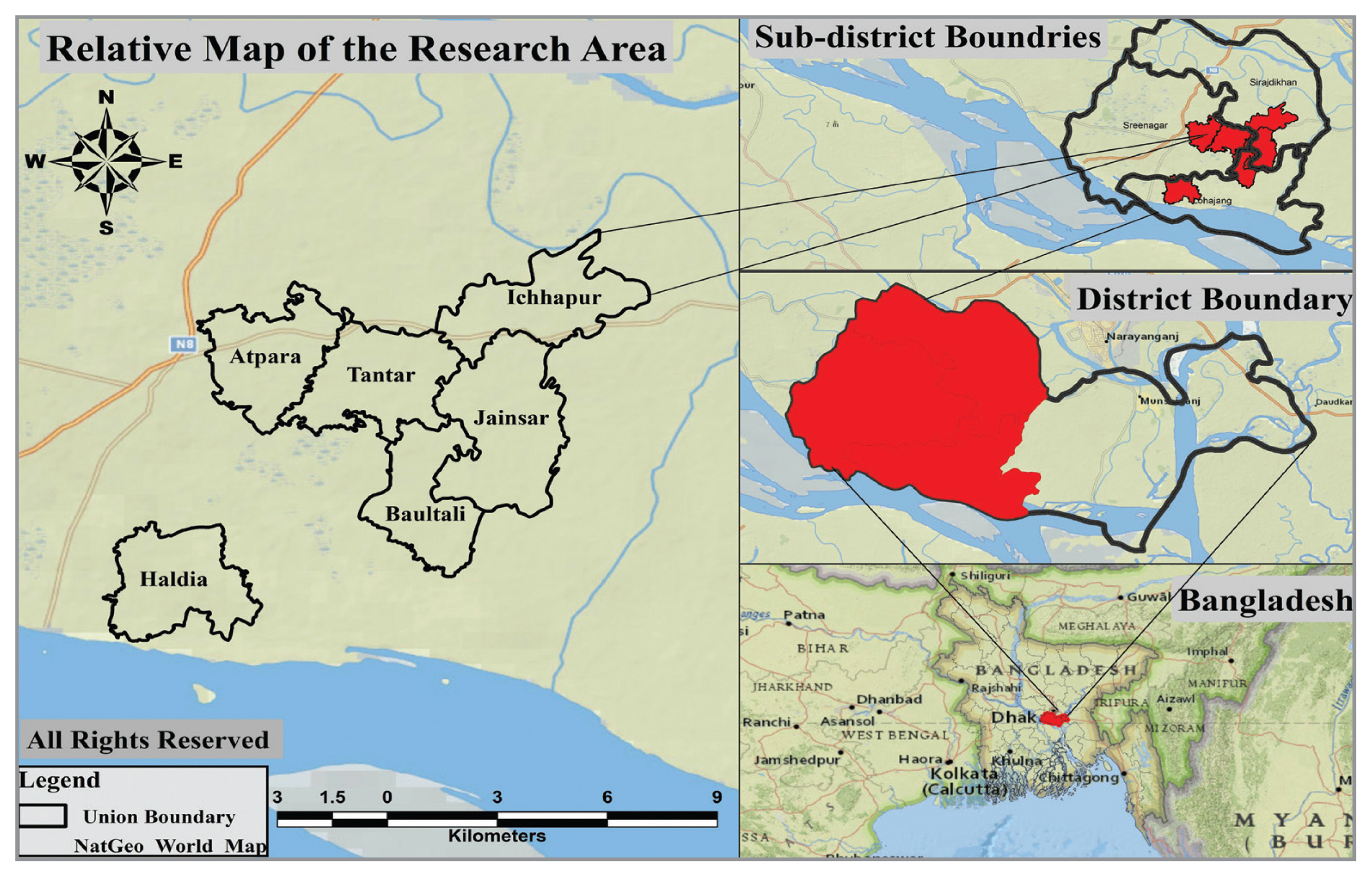
- A cross-sectional study was conducted from July 2018 to October 2018 in the Munshigonj district of Bangladesh. Using Cochran’s formula, there were 410 randomly selected adults (> 18 years) including smokers and non-smokers, with ≥ 1 child in their household [15]. Munshigonj district was randomly identified through the lottery method, as a representative study area. Three districts from the hill tracks, out of 64 districts of Bangladesh, were not included in the lottery for district selection because the ethnic background of the populations in those districts was different [16,17]. Data were collected through multistage sampling from 6 villages of the Munshigonj district (Figure 1). To identify these 6 villages, simple random sampling was used whereby 3 out of 6 sub-districts were selected, then 2 unions from each sub-district and within each union 1 village was selected, leading to 1 respective village of the district. Then, every third household member of selected villages was designated through systematic random sampling whilst considering the inclusion criteria. This consisted of both the smoker and non-smoker, who were aged > 18 years, exposed to secondhand smoke, and lived in a household that had ≥ 1 child. The percentage of the total population of each village was used to determine the number of participants from each village.
- Ethical approval was obtained from Naresuan University Institutional Review Board (COA no.: 675/2018, IRB no.: 0502/61), and all participants provided informed consent before participation.
- 2. Data collection
- An interviewer administrated questionnaire was used for data collection on a range of factors including demographics and status of smoking in the household. The dependent variable was denoted as self-reported exposure inside the household, and the independent variable was represented by exposure to secondhand smoke, and constructs from the theory of planned behavior (TPB). The questionnaire was developed in English and translated into Bengali (the national language of Bangladesh). The interview was conducted by a local interpreter who translated from Bengali into the local language. The status of smoking included the frequency and number of cigarettes smoked per day, and the age at which smoking began.
- Self-reported secondhand smoking was defined as “exposure to another person’s tobacco smoke weekly, more than once, for at least 15 minutes inside the household, in the past 30 days [18].” This study assessed exposure of children to secondhand smoke from the self-report of the adult in the household [7,19]. The exposure was measured as either exposed or non-exposed to secondhand smoke in the household. A score of 1 (exposed) or 0 (non-exposed) was assigned.
- Independent variables were related to secondhand smoking exposure and constructs of TPB. There were 8 variables of exposure to secondhand smoke including household smoke free rules, social norms and culture, environmental impact, religious beliefs, social awareness, and the influence of the media [measured by a score of 1 (positive answer) or 0 (negative answer)]. Knowledge of secondhand smoking was categorized as a binary variable [1 (true) or 0 (false)]. Perception of secondhand smoking and 4 constructs of TPB including intention, attitude, social support and perceived behavior control, were measured by a 3 points Likert scale (3 signified agree, 2 signified neither agree nor disagree, and 1 signified, disagree) [20].
- Bloom’s theory was used to classify the level of knowledge of secondhand smoking into 3 groups including ≤ 60% (low), > 60%–80% (moderate), and > 80% (high). Household smoke free rules, the influence of the media, social norms and culture, beliefs, environmental impact, religious beliefs, social awareness, perception of secondhand smoking and TPB constructs were categorized using mean scores using Best’s theory [21].
- The quality of the research tool was determined by item objective congruence (IOC) and Cronbach alpha. Three experts in the field of tobacco research examined the questionnaire item-by-item. The total IOC index was calculated as 0.87. Additionally, for reliability tests, a pilot survey was conducted on 40 samples (10% of the original sample size) of comparable features with the targeted population for the study. The Cronbach alpha coefficient for reliability was calculated to be 0.79 using SPSS Version 20 for Windows (IBM Corp., Armonk, NY). Both the IOC and the overall Cronbach alpha scores were acceptable values [22,23].
- 3. Statistical analysis
- The data were analyzed using SPSS Version 20 for Windows (IBM Corp., Armonk, NY, USA). Descriptive statistics were used for basic socio-demographic characteristics, whereas differences between categorical variables were assessed for significance using the Chi-square or Fisher’s exact test where appropriate. Univariate and multivariate logistic regression models were used to investigate the association between independent and dependent variables. Age, gender, education, household income, presence of a smoker in the household, household smoke free rules, social norms and culture, attitudes, knowledge of secondhand smoking, religious beliefs, and perceived behavior control, were confounders to determine the significant association of variables with secondhand smoking. Logistic regression (Enter method) was applied to determine the associations between potential factors. All results were presented as unadjusted and adjusted odds ratio (OR) with 95% confidence intervals (CI). Where p < 0.05, the difference was considered to be statistically significant.
Material and Methods
2.1. Dependent variables
2.2. Independent variables
2.3. Quality of the research tool
- 1. Sample characteristics
- Of the 410 participants, the majority (70.7%) were males. The mean (± SD) age of the study population was 40.39 (± 11.449) years. A large proportion (86.6%) were married and, 37.4% had completed secondary school. A quarter of the participants were unemployed (27.3%). Almost half of the participants had a moderate income (45.4%). Almost one third (30.0%) of households had at least 1 child.
- This study observed that gender, education, family income and type of housing had a significant association with secondhand smoking. In addition, it was determined that participants aged 25–50 years were more likely to be exposed to secondhand smoke (25.8%) and the majority were married (31.2%). There were 27.5% who were employed, and 14.5% had completed secondary school as well as belonging to the moderate-income group (19.0%). Households that had 2–4 children, which accounted for 24.4%, were more likely to be exposed to secondhand smoke (Table 1).
- 2. Smoker characteristics
- There were 109 participants (26.6%) who smoked, of which 1.5% were female. It was observed that 72.5% of smokers were regular smokers, and 35.7% started smoking between the ages of 16 to 20 years, which was followed by the age group 21–25 years (20.2%) and 26–30 years (19.3%). Among the smokers, 56.0% smoked < 5 cigarettes per day, and 29.4% smoked 5 to 10 cigarettes per day. The local shop was the most convenient place (91.7%) for smokers to purchase tobacco products compared with street vendors (Table 2).
- 3. Household practices for smoking in the household
- Out of the 410 households of our study, more than half of the households (53.4%) did not allow smoking inside the household and very few (5.4%) households had a specific area for smoking. Additionally, 22.7% of households had experienced smoking every day, 5.6% at least once a week whereas, 53.3% of households had never experienced smoking. Furthermore, 18.8% of household’s children were experienced smoking in front of them, and 4.4% of children of the household were sent to shops to buy smoking products by their household members (Table 3).
- 4. Associations between independent and dependent variables using univariate and multivariate analysis
- It was observed that households with a smoker significantly exposed other household members to secondhand smoke, which was observed using univariate (OR 70.050, 95% CI 35.722–137.365; p < 0.001) and multivariate (OR 48.382, 95% CI 20.18–115.959; p < 0.001) analysis. A significant association was determined using univariate analysis, between secondary education (OR 0.196, 95% CI 0.068–0.564; p = 0.002), and completion of college (OR 0.135, 95% CI 0.042–0.432; p = 0.001), with exposure to secondhand smoke. In addition, those household members who had completed a university education, had a significantly reduced chance of exposure to secondhand smoke in the home, as determined by univariate (OR 0.034, 95% CI 0.010–0.114; p < 0.001), and multivariate analysis (OR 0.106, 95% CI 0.013–0.843; p = 0.034). Furthermore, implementing strict smoke-free rules in the home significantly reduced exposure of household members to secondhand smoke, as determined by univariate (OR 0.006, 95% CI 0.001–0.046) and multivariate (OR 0.012, 95% CI 0.001–0.116; p < 0.001) analysis. Where there was a high influence of social norms and culture, there was an association with exposure of household members to secondhand smoke using multivariate analysis (OR 0.135, 95% CI 0.023–0.804; p = 0.028). Moreover, a moderate level of knowledge about secondhand smoking (OR 0.418, 95% CI 0.248–0.705; p = 0.001), or a high level of knowledge (OR 0.239, 95% CI 0.117–0.485; p < 0.001) was associated with exposure to secondhand smoke in the home using univariate analysis. In multivariate analysis of a moderate level of knowledge about secondhand smoking, an association was observed with exposure to secondhand smoke in the home (OR 0.385, 95% CI 0.149–0.997; p < 0.001) (Table 4).
Results
- This study is among a small number of studies that are related to secondhand smoking among children in households of rural Bangladesh. There were 5 factors in this study that were significantly associated with the reduction in exposure of children to secondhand smoke. Among them, the presence of a smoker in the household was a risk factor. The households that did not have a smoker, were 48.38 times less likely to expose members of the household to secondhand smoke. This finding is in line with a study conducted in primary school aged children in the capital of Bangladesh where a significant association between living with a smoker and exposure to secondhand smoke was reported [10]. Similar findings have been reported, among children and adolescents in Germany, which is considered a developed country [24]. Smokers in these households should be viewing this behavior as risky practice to smoke at home.
- Participants who graduated from university were less likely to be exposed to secondhand smoke. This finding was similar to a study conducted in 2011 in Bangladesh, where women who did not have a formal education were exposed to secondhand smoke at a level 3.93 times higher than women who had higher education [14]. In another report from 2008 to 2010, 60% of reproductive aged women, with no formal education were exposed to secondhand smoke compared with 26.1% who had completed higher education [25]. Similarly, in the WHO global adult tobacco survey data of Bangladesh, 2009, it was reported that amongst smokers, 62.9% did not have a formal education, which indicated that a lower level of education was associated with exposure to secondhand smoke [26]. This finding was consistent with research from India, Philippines, Thailand, and Egypt [25]. For individuals with higher education, there may be a better understanding of secondhand smoking which promotes the tendency to adopt home smoking restrictions and to make the household smoke free. This current study also observed that those households who practiced smoke-free rules were less likely to be exposed to secondhand smoking. A previous study conducted in urban Bangladesh also reported smoke-free rules reduced exposure to secondhand smoke [27]. This result was also consistent with the findings of a study conducted in China [28] which reflected that smoke-free house rules may be helpful in the reduction of exposure to secondhand smoke in the household.
- This current study also revealed that high practice of social norms and culture, was more likely to reduce secondhand smoking. Every country has its cultural norms, and in Bangladesh, especially in rural areas, it is very unusual to smoke in front of an older person out of respect. This same attitude towards children would help reduce their exposure to secondhand smoke. This data was unique to this current study. Additionally, this study also observed that restricted cultural norms prevented women from asking their husband not to smoke inside the house. Removing this barrier by empowering women may reduce their exposure to secondhand smoke. The findings in this current study are in line with the qualitative study conducted among rural Bangladeshi and urban Indian women, which observed male attitudes were a significant predictor to reduce smoking [29]. Moreover, the cultural norms of Bangladesh perpetuate a superior social status for men enabling them to smoke in the house if they choose to do so which increases exposure of the household members to secondhand smoke [7].
- This current study revealed that a moderate level of knowledge of secondhand smoking would reduce the exposure of others in the home to secondhand smoke. Smoking is a common practice in rural Bangladesh. People with a high level of knowledge about secondhand smoking may be reluctant to stop smoking inside the household or in front of children, because they know that they are harming themselves through smoking. However, those who have a moderate level of knowledge may question their behavior and stop smoking in the household or in front of children. This point of view is very controversial but nevertheless was a factor raised by this study.
- The study had some limitations in that cross-sectional analysis was performed and therefore causal relationships could not be determined from this study. In addition, self-reported exposure to smoke may lead to misclassification (differential and non-differential) due to recall and reporting bias. Moreover, the self-reported exposure to smoke was not validated with cotinine levels in study participants due to lack of funding. Furthermore, the study only accounted for self-reported exposure to smoke in the household. Other settings, such as restaurants, workplaces, or public places were not considered in this study as potential places for exposure to secondhand smoke.
- An effective public health intervention model can be developed by using the findings of this to reduce the exposure of children in the rural area of Bangladesh to secondhand smoke.
Discussion
-
Acknowledgements
- The first author acknowledges Naresuan University, Thailand, for awarding him a Naresuan University International Student Scholarship in 2016 to pursue a Doctorate in Public Health. All authors also acknowledge the anonymous reviewers for their critical and constructive comments for the development of the manuscript.
Acknowledgments
- 1. Centers for Disease Control and Prevention [Internet]. Health Effects of Secondhand Smoke Atlanta (GA): Centers for Disease Control and Prevention; 2018 [cited 2019 Mar 30]. Available from: https://www.cdc.gov/tobacco/data_statistics/fact_sheets/secondhand_smoke/health_effects/index.htm.
- 2. World Health Organization [Internet]. Tobacco Geneva (Switzerland): World Health Organization; 2019 [cited 2019 Mar 30]. Available from: https://www.who.int/news-room/fact-sheets/detail/tobacco.
- 3. Chao MR, Cooke MS, Kuo CY, et al. Children are particularly vulnerable to environmental tobacco smoke exposure: Evidence from biomarkers of tobacco-specific nitrosamines, and oxidative stress. Environ Int 2018;120:238−45. PMID: 10.1016/j.envint.2018.08.006. PMID: 30103123.ArticlePubMed
- 4. Mbulo L, Palipudi KM, Andes L, et al. Secondhand smoke exposure at home among one billion children in 21 countries: Findings from the Global Adult Tobacco Survey (GATS). Tob Control 2016;25(E2). e95−e100. PMID: 10.1136/tobaccocontrol-2015-052693. PMID: 26869598. PMID: 5488799.ArticlePubMedPMC
- 5. Ekerbicer HC, Celik M, Guler E, et al. Evaluating environmental tobacco smoke exposure in a group of Turkish primary school students and developing intervention methods for prevention. BMC Public Health 2007;7:202PMID: 10.1186/1471-2458-7-202. PMID: 17692111. PMID: 2048514.ArticlePubMedPMCPDF
- 6. Eriksen M, Mackay J, Schluger N, et al. The Tobacco Atlas. New York (NY): World Lung Foundation; 2015.
- 7. Zafar UAN, Huque R, Akter S, et al. Children’s exposure to second-hand smoke at home in Bangladesh: A community survey. BMJ 2013;3(11). e003059. Article
- 8. World Health Organization [Internet]. Global Adult Tobacco Survey Fact Sheet Bangladesh Geneva (Switzerland): World Health Organization; 2017 [cited 2019 Apr 2]. Available from: http://www.searo.who.int/bangladesh/gatsbangladesh2017fs14aug2018.pdf?ua=1.
- 9. World Health Organization [Internet]. Global Youth Tobacco Survey Bangladesh Report Geneva (Switzerland): World Health Organization; 2013 [cited 2019 Apr 2]. Available from: https://apps.who.int/iris/bitstream/handle/10665/164335/9789290224815-GYTS-TFI.pdf?sequence=1&isAllowed=y.
- 10. Shah S, Kanaan M, Huque R, et al. Secondhand smoke exposure in primary school children: A survey in Dhaka, Bangladesh. Nicotine Tob Res 2019;21(4). 416−23. PMID: 10.1093/ntr/ntx248. PMID: 6472694.ArticlePubMedPDF
- 11. World Health Organization [Internet]. Global Adult Tobacco Survey Comparison Fact Sheet Bangladesh 2009 and 2017 Geneva (Switzerland): World Health Organization; [cited 2019 Apr 2]. Available from: http://bbs.portal.gov.bd/sites/default/files/files/bbs.portal.gov.bd/page/57def76a_aa3c_46e3_9f80_53732eb94a83/GATS_BAN_2017_Comparison_Fact%20Sheet.pdf.
- 12. Rabeya SJA, Nasreen N, Mithila F, et al. Perceptions about the health effects of passive smoking among Bangladeshi young adults. Int J Stat Med Res 2016;5(4). 248−54. PMID: 10.6000/1929-6029.2016.05.04.3.Article
- 13. Abdullah AS, Driezen P, Sansone G, et al. Correlates of exposure to secondhand smoke (SHS) at home among non-smoking adults in Bangladesh: Findings from the ITC Bangladesh survey. BMC Pulm Med 2014;14:117PMID: 10.1186/1471-2466-14-117. PMID: 25027238. PMID: 4107590.ArticlePubMedPMCPDF
- 14. Fischer F, Minnwegen M, Kaneider U, et al. Prevalence and determinants of secondhand smoke exposure among women in Bangladesh, 2011. Nicotine Tob Res 2015;17(1). 58−65. PMID: 10.1093/ntr/ntu129.ArticlePubMed
- 15. Cochran WG. Sampling Techniques. 3rd ed. New York (NY): John Wiley & Sons; 1977.
- 16. Bangladesh National Portal [Internet]. District List [cited 2019 Apr 4]. Available from: http://www.bangladesh.gov.bd/site/view/district-list/District-List.
- 17. Uddin N. Politics of cultural difference: Identity and marginality in the Chittagong hill tracts of Bangladesh. South Asian Surv 2010;17(2). 283−94. PMID: 10.1177/097152311201700206.Article
- 18. Yang L, Tong EK, Mao Z, et al. Exposure to secondhand smoke and associated factors among non-smoking pregnant women with smoking husbands in Sichuan province, China. Acta Obstet Gynecol Scand 2010;89(4). 549−57. PMID: 10.3109/00016341003713851. PMID: 20367430. PMID: 3759004.ArticlePubMedPMC
- 19. Avila-Tang E, Elf JL, Cummings KM, et al. Assessing secondhand smoke exposure with reported measures. Tob Control 2013;22(3). 156−63. PMID: 10.1136/tobaccocontrol-2011-050296. PMID: 3639349.ArticlePubMed
- 20. Srithongthum J. Factors affecting exercise behavior of people exercising at Lumpini park. Bangkok: Srinakharinwirot University; 2007.
- 21. Worasathit R, Wattana W, Okanurak K, et al. Health education and factors influencing acceptance of and willingness to pay for influenza vaccination among older adults. BMC Geriatr 2015;15:136PMID: 10.1186/s12877-015-0137-6. PMID: 26503289. PMID: 4620638.ArticlePubMedPMCPDF
- 22. Turner R, Carlson L. Indexes of Item-Objective Congruence for multidimensional items. 2003. pp 163−71.
- 23. Phetphum C, Pongpreecha B, Hangsantea J, et al. Predicting Factors for Smoking Behavior among Women Who Frequent Nightlife Entertainment Venues around a University in the Northern Region of Thailand. Subst Abuse 2018;12:1178221818804530PMID: 30305795. PMID: 6176538.ArticlePubMedPMC
- 24. Kuntz B, Lampert T. Social disparities in parental smoking and young children’s exposure to secondhand smoke at home: A time-trend analysis of repeated cross-sectional data from the German KiGGS study between 2003–2006 and 2009–2012. BMC Public Health 2016;16:485PMID: 10.1186/s12889-016-3175-x.ArticlePubMedPMC
- 25. Centers for Disease Control and Prevention [Internet]. Current Tobacco Use and Secondhand Smoke Exposure Among Women of Reproductive Age — 14 Countries, 2008–2010 Atlanta (GA): Centers for Disease Control and Prevention; 2012 [cited 2019 Apr 7]. Available from: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6143a4.htm.
- 26. World Health Organization [Intenret]. Global Adult Tobacco Survey Bangladesh Report 2009 Geneva (Switzerland): World Health Organization; [cited 2019 Apr 7]. Available from: https://www.who.int/tobacco/surveillance/global_adult_tobacco_survey_bangladesh_report_2009.pdf?ua=1.
- 27. Huque R, Dogar O, Cameron I, et al. Children learning about second-hand smoking: A feasibility cluster randomized controlled trial. Nicotine Tob Res 2015;17(12). 1465−72. PMID: 10.1093/ntr/ntv015. PMID: 25634936.ArticlePubMedPDF
- 28. Zheng PP, Berg CJ, Kegler MC, et al. Smoke-free homes and home exposure to secondhand smoke in Shanghai, China. Int J Environ Res Public Health 2014;11(11). 12015−28. PMID: 10.3390/ijerph111112015. PMID: 25419875. PMID: 4245657.ArticlePubMedPMC
- 29. Jackson C, Huque R, Satyanarayana V, et al. “He doesn’t listen to my words at all, so i don’t tell him anything”—a qualitative investigation on exposure to second hand smoke among pregnant women, their husbands and family members from rural Bangladesh and urban India”. Int J Environ Res Public Health 2016;13(11). E1098PMID: 10.3390/ijerph13111098. PMID: 27834841. PMID: 5129308.Article
References
Table 1Socio-demographic characteristics (N = 410).
| Characteristics | n (%) | Exposed (%) | Not exposed (%) | p |
|---|---|---|---|---|
| Age (y) | 0.683* | |||
| 18–24 | 47 (11.5) | 19 (4.6) | 28 (6.8) | |
| 25–50 | 300 (73.2) | 106 (25.8) | 194 (47.4) | |
| ≥ 50 | 63 (15.3) | 25 (6.1) | 38 (9.3) | |
|
|
||||
| Marital status | 0.652* | |||
| Single | 55 (13.4) | 22 (5.4) | 33 (8.0) | |
| Married | 355 (86.6) | 128 (31.2) | 227 (55.4) | |
|
|
||||
| Education | < 0.001* | |||
| No formal schooling | 21 (5.1) | 16 (3.9) | 5 (1.4) | |
| Primary | 82 (20.0) | 49 (11.8) | 33 (8.2) | |
| Secondary | 153 (37.4) | 59 (14.5) | 94 (22.3) | |
| College | 53 (12.9) | 16 (3.9) | 37 (9.2) | |
| University | 101 (24.6) | 10 (2.6) | 91 (22.2) | |
|
|
||||
| Employment | 0.421† | |||
| Employed | 298 (72.7) | 113 (27.5) | 185 (45.1) | |
| Unemployed | 112 (27.3) | 37 (9.1) | 75 (18.3) | |
|
|
||||
| Family income (BDT) | < 0.001* | |||
| Low income group | 124 (30.2) | 52 (12.7) | 72 (17.5) | |
| Moderate income group | 186 (45.4) | 78 (19.0) | 108 (26.4) | |
| High income group | 100 (24.4) | 20 (4.9) | 80 (19.5) | |
|
|
||||
| No. of Children in the Household | 0.945 * | |||
| 1 child | 123 (30.0) | 44 (10.6) | 79 (19.6) | |
| 2–4 children | 272 (63.3) | 100 (24.4) | 172 (41.7) | |
| 5 or more children | 15 (3.7) | 6 (1.5) | 9 (2.2) | |
|
|
||||
| Type of housing | < 0.001* | |||
| Building | 121 (29.5) | 34 (8.3) | 87 (21.2) | |
| Tin shade house | 282 (68.8) | 115 (28.0) | 167 (40.8) | |
| Fence/slum | 71.7 (1.7) | 1 (0.2) | 6 (1.5) | |
Table 2Smoker’s characteristics (N = 109).
Table 3Characteristics of smoking practices in the household (N = 410).
Table 4Univariate and multivariate analysis to determine the association of the independent (secondhand smoking) and dependent variables (N = 410).
| Dependent variables | n (%) | Unadjusted univariate analysis | Adjusted* multivariate analysis | ||
|---|---|---|---|---|---|
|
|
|
||||
| OR (95% CI) | p | OR (95% CI) | p | ||
| Smoker present in the household | |||||
| No | 238 (58.04) | Reference | |||
| Yes | 171 (41.70) | 70.050 (35.722–137.365) | < 0.001 | 48.382 (20.18–115.959) | < 0.001 |
|
|
|||||
| Education | |||||
| No formal schooling | 21 (5.12) | Reference | |||
| Primary school completed | 82 (20.00) | 0.464 (0.155–1.390) | 0.170 | 0.655 (0.100– 4.286) | 0.659 |
| Secondary school completed | 153 (36.58) | 0.196 (0.068 –0.564) | 0.002 | 0.370 (0.057–2.406) | 0.298 |
| College completed | 53 (12.92) | 0.135 (0.042–0.432) | 0.001 | 0.255 (0.033–2.001) | 0.194 |
| University completed | 101 (24.63) | 0.034 (0.010–0.114) | < 0.001 | 0.106 (0.013–0.843) | 0.034 |
|
|
|||||
| Smoke free rules in the household | |||||
| Low implementation | 58 (14.14) | Reference | |||
| High implementation | 351 (85.60) | 0.006 (0.001–0.046) | < 0.001 | 0.012 (0.001–0.116) | < 0.001 |
|
|
|||||
| Social norms and culture | |||||
| Low influence | 19 (4.63) | Reference | |||
| Moderate influence | 86 (20.97) | 0.966 (0.357–2.614) | 0.946 | 0.172 (0.025–1.155) | 0.070 |
| High influence | 304 (74.14) | 0.550 (0.217–1.396) | 0.209 | 0.135 (0.023–0.804) | 0.028 |
|
|
|||||
| Knowledge of secondhand smoking | |||||
| Low | 74 (18.04) | Reference | |||
| Moderate | 262 (63.90) | 0.418 (0.248–0.705) | 0.001 | 0.385 (0.149–0.997) | 0.049 |
| High | 73 (17.80) | 0.239 (0.117–0.485) | < 0.001 | 0.729 (0.217–2.450) | 0.609 |
Figure & Data
References
Citations
Citations to this article as recorded by 

- Second Hand Smoke Exposure among Children in Indian Homes: Findings from the Global Adult Tobacco Survey
Jaya Prasad Tripathy
Behavioral Medicine.2024; 50(1): 75. CrossRef - Exposure to secondhand smoke is associated with poor sleep quality among non-smoking university students in Bangladesh: a cross-sectional survey
Md. Hasan Al Banna, Keith Brazendale, Mohammad Hamiduzzaman, Bright Opoku Ahinkorah, Mohammad Tazrian Abid, M. A. Rifat, Mst. Sadia Sultana, Justice Kanor Tetteh, Satyajit Kundu, Md Shaheenur Rahman Shekhar, Md Khaleduzzaman, Md. Nazmul Hassan
Scientific Reports.2023;[Epub] CrossRef - Need for sensitization on serious threats of second-hand smoke: Findings from a national study in Mauritius, a small island developing state in the Indian Ocean
Marie Chan Sun, Urmila D. Beeharry Panray, Jayrani Cheeneebash, Raj Gunesh
Preventive Medicine Reports.2022; 25: 101667. CrossRef - Muslim Communities Learning About Second-hand Smoke in Bangladesh (MCLASS II): a combined evidence and theory-based plus partnership intervention development approach
Ian Kellar, Zunayed Al Azdi, Cath Jackson, Rumana Huque, Noreen Dadirai Mdege, Kamran Siddiqi
Pilot and Feasibility Studies.2022;[Epub] CrossRef - Social measures for reducing exposure to secondhand
smoke in migrant workers of sugarcane harvest in the lower
northern region of Thailand
Narongsak Noosorn, Anukool Manoton, Rishad Choudhury Robin
Tobacco Induced Diseases.2021; 19(September): 1. CrossRef


 PubReader
PubReader ePub Link
ePub Link Cite
Cite